Case report
Multiple Meningocele in Klippel-Feil Syndrome: Case Report
- Radhi Hafed *
- Labib O
- Chebaatha A
- Oukessou Y
- Rouadi S
- Abada R
- Roubal M
- Mahtar M
Department of ENT, University of Hassen II, Casablanca, Morocco.
*Corresponding Author: Radhi Med El Hafed, Department of ENT, University of Hassen II, Casablanca, Morocco.
Citation: R Hafed, Labib O, Chebaatha A, Oukessou Y, Rouadi S, et al. (2022). Multiple Meningocele in Klippel-Feil Syndrome: Case Report. International Journal of Medical Case Reports and Reviews, BRS Publishers. 1(1); DOI: 10.59657/2837-8172.brs.22.001
Copyright: © 2022 Radhi Med El Hafed, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: October 23, 2022 | Accepted: November 08, 2022 | Published: November 12, 2022
Abstract
Klippel–Feil syndrome (KFS) is a rare congenital skeletal malformation characterized by the fusion of various cervical and occasionally thoracic and lumbar vertebrae. It may be seen as the fusion between two vertebras of all cervical vertebras, Congenital cervical fusion occurs as a result of failure in normal segmentation of cervical summits. Cause of this failure is unknown and occurs at second-eight weeks of gestation.
25 years old, patient presented to our counseling center with a 4-month history of progressive dysphagia. Ent exam showed a soft retropharyngeal mass displacing the left tonsil measuring a little about 6 cm with no sign of ulceration or local inflammation, a short neck was noted with a limitation of flexion and extension movement and low-lying hairline with a psychomotor retardation; which raises the suspicion of Klippel Feil syndrome undiagnosed.
Cervical magnetic resonance imaging (MRI) was done which showed a cervical cystic formation compressive oval well limited with regular contours and fluid content with dark aspect in T1 weighted sequences and bright in T2 weighted sequences with regular wall enhanced after injection of gadolinium measuring 8.2*4.3 cm spread over 8.9 cm high This formation appears to continue with the subarachnoid spaces of the posterior cerebral fossa through the hypoglossal nerve canal with doubt about involvement of the jugular foramen.
Thoracic CT scan demonstrated a lateral cystic mass exiting out of the intervertebral foramen of T6-T7 showing the same characteristics as the cervical formation above.
Klippel-Feil syndrome is a rare congenital skeletal malformation characterized by fusion of several cervical and sometimes thoracic and lumbar vertebrae, leading to a low hairline and a short neck.
The pathological feature is congenital fusion of two or more cervical vertebrae. The fusion is thought to be associated with reduced expression of the Pax gene in sclerotomes during chondrification of the vertebra.
Klippel-Feil syndrome is usually diagnosed in childhood. However, associated abnormalities may delay diagnosis. The challenge for the specialist is to recognize concomitant abnormalities and perform the appropriate work-up for the diagnosis of Klippel-Feil syndrome.
Keywords: klippel–feil syndrome; meningoceles; posterior cerebral fossa; para pharyngeal space
Introduction
Klippel–Feil syndrome (KFS) is a rare congenital skeletal malformation characterized by the fusion of various cervical and occasionally thoracic and lumbar vertebrae. It may be seen as the fusion between two vertebras of all cervical vertebras, Congenital cervical fusion occurs as a result of failure in normal segmentation of cervical summits. Cause of this failure is unknown and occurs at second-eight weeks of gestation [1].
Incidences are estimated to be approximately one out of 40000-42000 births and are seen more frequently in females [2].
The diagnosis is based on the clinical triad of a short neck, low posterior hairline and limited neck movement. Less than 50% of patients present with this clinical triad and a wide range of associated anomalies may be present. This heterogeneity has complicated the clarification of the genetic etiology and management of the syndrome [2].
Meningoceles through the posterior cerebral fossa is exceptional, and their association with thoracic myelomeningocele has never been cited in the literature. here we rapport the first case of cervical meningocele through the posterior cerebral fossa associated with thoracic myelomeningocele in a Klippel-Feil syndrome.
Case Report
The patient is 25 years old, presented to our counseling center with a 4-month history of progressive dysphagia. She didn’t have any history of any chronic diseases or anterior medications or allergies or any toxic consumption nor any familial history of genetic diseases. She didn’t have any surgical history. she was cachectic with a BMI of 15.4, slightly asthenic, not keeping eye contact with a depressive demeanor.
A Ent exam showed a soft retropharyngeal mass displacing the left tonsil measuring a little about 6 cm with no sign of ulceration or local inflammation (fig1), a cervical palpation showed a same consistency mass in the upper left cervical area with no cervical lymphadenopathies associated and a flexible nasendoscope examination showed a reduction of the upper airway. a short neck was noted with a limitation of flexion and extension movement and low-lying hairline a thorough neurological examination including cranial nerves, sensory, motor, and reflexes, and gait testing was normal with a psychomotor retardation was noted which raises the suspicion of Klippel Feil syndrome undiagnosed. The rest of the examination showed a thoracic scoliosis, multiple cafe-au-lait macules were noted on the trunk and the back no neurofibromas. The cardiac exam was normal, as the pulmonary and abdominal exam. An eye examination with fundus showed no abnormalities.
Figure 1: Para pharyngeal mass displacing the left tonsil
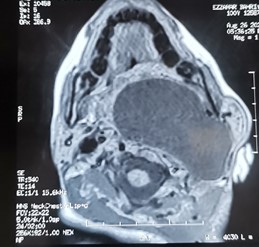
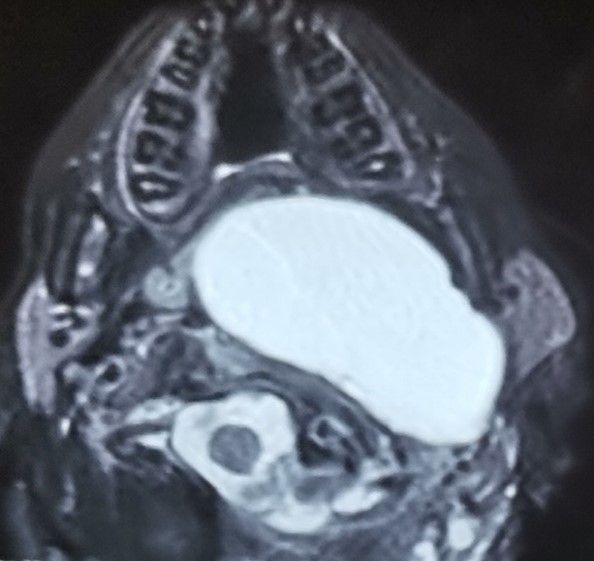
Cervical magnetic resonance imaging (MRI) was done which showed a cervical cystic formation compressive oval well limited with regular contours and fluid content with dark aspect in T1 weighted sequences (fig2) and bright in T2 weighted sequences with regular wall enhanced after injection of gadolinium measuring 8.2*4.3 cm spread over 8.9 cm high (fig3). This formation appears to continue with the subarachnoid spaces of the posterior cerebral fossa through the hypoglossal nerve canal with doubt about involvement of the jugular foramen.
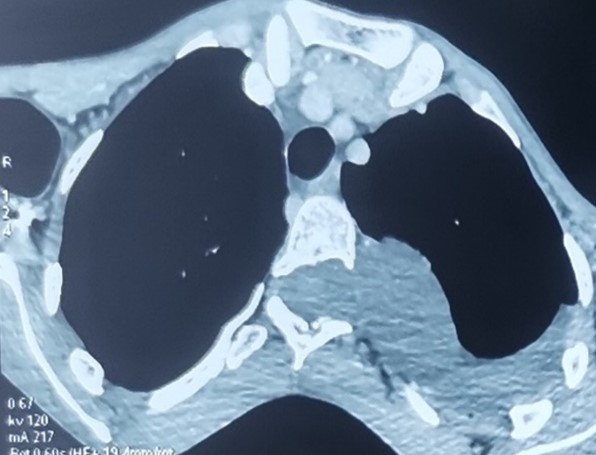
Thoracic CT scan demonstrated a lateral cystic mass exiting out of the intervertebral foramen of T6-T7 showing the same characteristics as the cervical formation above (fig4).
Figure 2: T1 image showed cystic mass hyposignal
Figure 3: T2 bright cystic mass on the Para pharyngeal space
Figure 4: thoracic CT scan showed meningocele through thoracic vertebrae
Serological testing, full blood count, and C-reactive protein were normal. The patient's case was discussed in a multidisciplinary staff concluding that the patient should be referred to the neurosurgery department for possible resection of the mass after a deep enlightenment session on the risks and possible complications of the surgery, the patient refused to be operated and she opted for therapeutic abstention with regular monitoring by the two ENT and neurosurgical teams.
During the three first months, the patient did not express any worsening of dysphagia and the clinical assessment of the mass seems to be constant, MRI exam and genetic counseling were scheduled in the next month.
Discussion
Klippel-Feil syndrome is a rare congenital skeletal malformation characterized by fusion of several cervical and sometimes thoracic and lumbar vertebrae, leading to a low hairline and a short neck. Although KFS has been described as early as the 16th century, Maurice Klippel and André Feil were the first to describe the complete picture of the syndrome in a case report of a 46-year-old French tailor with a short, immobile neck with massive fusion of the upper cervical and thoracic vertebrae [3].
The pathological feature is congenital fusion of two or more cervical vertebrae. The fusion is thought to be associated with reduced expression of the Pax gene in sclerotomes during chondrification of the vertebra. Mutations in the GDF6 gene locus have also induced similar bone defects in a mouse model [1,4].
Patients with Klippel-Feil syndrome can be divided into three groups according to the location of the vertebral fusions. In type 1, there is fusion of all or almost all cervical vertebrae and the upper thoracic vertebrae. In type 2, there is fusion into double or triple segments. In type 3, fusion of the lower vertebrae accompanies fusion of the cervical vertebrae. While types 1 and 3 are autosomal recessive, type 2 is autosomal dominant. Although type 2 is more associated with skeletal abnormalities, the skeletal system abnormalities have more serious consequences [1,5,6].
The disparity in levels between the fused vertebrae and cysts in some patients is best explained by the suggestion that, during the development of the mediastinum, caudal migration occurs and the vertebral and intraspinal anomalies are left behind [7].
The cyst wall linings range from a simple cuboidal to columnar to pseudostratified epithelial layer resting on a thin layer of fibrous connective tissue. Goblet cells, giving a positive reaction with Alcian blue stain, and ciliated cells are commonly observed in varying proportions [8].
Our patient can be classed type 2, with two segment involvement; however, the protrusion of meningocele through the hypoglossal nerve canal to the Para pharyngeal space remain unclear in contrast with etiopathogenetic of Klippel-Feil syndrome.
KFS is usually diagnosed in childhood. However, associated abnormalities may delay diagnosis. The challenge for the specialist is to recognize concomitant abnormalities and perform the appropriate work-up for the diagnosis of KFS. Key considerations in the management of KFS include radiographic evaluation of hypermobile cervical segments, recognition of high-risk patterns of skeletal abnormalities, and proper referral of associated abnormalities.
In our case misdiagnosed of Klippel Feil syndrome can conduct to biopsy of the Para pharyngeal masse, which can conduct to meningitis and death.
Beside orthopedics clinical evaluations, patients with Klippel- Feil syndrome should be assessed by anteroposterior and lateral cervical flexion/extension and thoracolumbar radiographies, abdominal ultrasonography, and were subjected to systemic examination to detect any urological, cardiological, otorhinolaryngological, neurological and psychiatric finding. Computed tomography and magnetic resonance imaging where necessary [9].
In patients with hypermobility on non-fused vertebrae, prophylactic fusion should not be performed unless the patient has neurological problems due to a disc problem that may develop later. Severely affected patients have a good prognosis if cardiopulmonary, genitourinary and auditory problems are treated early [10]. In occipito-cervical passage anomalies, the high morbidity and mortality rates have been frightening, as the cervical cord and brain stem are very close to each other [11]. In the present case, we found a voluminous meningocele cyst in Para pharyngeal space which surgery can be complicated due to noble structure around.
Conclusion
Our case is of great interest because of the extremely uncommon occurrence of anterior meningocele into the Para pharyngeal space. To the best of our knowledge, this is the first case reported in the literature. Cervical meningocele could also be associated with multiple other spinal abnormalities, which highlights the importance of comprehensive preoperative radiological examinations.
Patients with Klippel Feil Syndrome should be assessed for associated systemic abnormalities beside cervical fusion, and such cases should be identified and treated at an early stage to minimize cosmetic & social stigma to the patient.
References
- Tracy MR, Dormans JP, Kusumi K. (2004). Klippel-Feil syndrome: clinical features and current understanding of etiology. Clin Orthop Relat Res. 424:183-190.
Publisher | Google Scholor - Frikha R. (2020). Klippel-Feil syndrome: a review of the literature. Clinical Dysmorphology. 29(1):35-37.
Publisher | Google Scholor - Klippel M, Feil A. (1912). Anomalie de la colonne vertebrale par absence des vertebres cervicales. Cage thoracique remontant jusqua la base du crane. Bull Mem Soc Anat Paris. 87:185.
Publisher | Google Scholor - Settle SH Jr, Rountree RB, Sinha A, et al. (2003). Multiple joint and skeletal patterning defects caused by single and double mutations in the mouse Gdf6 and Gdf5 genes. Dev Biol. 254:116-130.
Publisher | Google Scholor - Thomsen M, Krober M, Schneider U, Carstens C. (2000). Congenital limb deficiences associated with Klippel-Feil syndrome: a sur- vey of 57 subjects. Acta Orthop Scand. 71:461-464.
Publisher | Google Scholor - Thomsen MN, Schneider U, Weber M, Johannisson R, Niethard FU. (1997). Scoliosis and congenital anomalies associat- ed with Klippel-Feil syndrome types I-III. Spine. 22:396-401.
Publisher | Google Scholor - Tekkok IH, Palaoglu S, Erbengi A, Onol B. (1992). Intra- medullary epidermoid cyst of the cervical spinal cord associated with an extraspinal neuroenteric cyst: case report. Neurosurgery 31:121-125.
Publisher | Google Scholor - Savage JJ, Casey JN, McNeill IT, Sherman JH. (2010). Neurenteric cysts of the spine. J Craniovertebr Junction Spine. 1:58-63.
Publisher | Google Scholor - Nagib MG, Maxwell RE, Chou SN. (1985). Klippel-Feil syndrome in children: clinical features and management. Child Nerv Syst. 1(5):255-263.
Publisher | Google Scholor - Pizzutillo PD, Woods M, Nicholson L, MacEwen GD. (1994). Risk factors in Klippel-Feil syndrome. Spine. 19:2110-2116.
Publisher | Google Scholor - Herring JA. (2002). Disorder of the neck. Tachdjian’s pediatric orthopaedics. 1(3):173-187.
Publisher | Google Scholor