Review Article
More Orally Transmitted Aphorisms (OTA’s-2) in Dentistry
McGill University, Faculty of Dental Medicine and Associated Oral Health Sciences, Canada
*Corresponding Author: Louis Z.G. Touyz,McGill University, Faculty of Dental Medicine and Associated Oral Health Sciences, Canada
Citation: Louis Z.G. Touyz. (2023). More Orally Transmitted Aphorisms (OTA’s-2) in Dentistry. Dentistry and Oral Health Care, Biores Scientia Publishers, 2(2):1-4. DOI: 10.59657/2993-0863.brs.23.011
Copyright: © 2023 Louis Z.G. Touyz, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 31, 2023 | Accepted: August 14, 2023 | Published: August 18, 2023
Abstract
Background: Dentistry training is based on biomedical sciences. Previous clinical experience has produced principles that influence the practice of dentistry. Some of these oral advisories have been recorded.
Aim: This article reports some more important orally transferred aphorisms (OTAs: Tapping-tooth-pain, Vertical Movement, Biopsies, Recognition, Ruboffable, ODD principle, and Show-up plaque), Assumption, and deconstructs their implications, reasons and significance.
Discussion: These reported OTAs evolve from clinical expertise and each act as a guiding policy in the execution of dentistry.
Conclusion: OTA’s have been inherited from succedaneous progressive generations of dentists; those reported here may be supplemented in future as long as dentistry evolves as a profession to produce more accumulating wisdom among dental health care workers.
Keywords: aphorisms; antibiotics; cosmetic; dentistry; oral; treatment; teaching; transgenerational; wisdom
Introduction
Dentistry training is based on biomedical sciences, as insights derived from these biomedical disciplines form the foundations of practicing medicine. Dentistry is a sub-specialty of Medicine, dealing with all aspects relating to the oral cavity, the head and neck, and as to how they influence the whole human body and also human behavior. Verbal passing on of observations, insights, diagnostic skills, interpretations and foundational wisdom, may be lost if not codified for future generations. Previous clinical experience, procured by practicing dental professionals over centuries, has produced principles that influence the modern practice of dentistry. Some of these of these oral advisories have been recorded as Orally Transmitted Aphorisms (OTAs) [1,2].
Aim
This report records more OTAs: Tapping-tooth-pain, Vertical Movement, Biopsies, Recognition, Ruboffable, The ODD principle, and Show-up plaque, and Assumption, in the hope of advancing and refining clinical acumen by facilitating recollection of principles that dictate the practice of dentistry.
Orally Transmitted Aphorisms
“Tapping a tooth should not induce pain.” If tapping a tooth gently with an instrument, like the solid handle of a mouth mirror, and the tapping induces pain, this indicates the tooth has a periodontitis, and the cause for that must be investigated. This sign most commonly derives from traumatic injury and consequent inflammation of the tooth’s periodontal ligament. A traumatic periodontitis frequently arises from ‘high-spots’ on restorations. These are usually treated by locating the area by biting on a blue occlusal ribbon, or biting on a thin, soft wax- wafer, marking the areas of contact, and then grinding down the affected area. This is done without local analgesia and relief is usually immediate. The tapping pain sign may also present often produced by spreading infection from a peri-apical or periodontal abscess. Draining the abscess is indicated followed by endodontic and/or periodontal therapy respectively. Any tooth with a cracked root may also have pain induced when chewing or with tapping. This tapping-tooth pain from infected causes all too frequently results in exodontia [2].
“Any noticeable vertical movement on a natural tooth or implant indicates a poor prognosis and implies extraction.” Natural tooth movement in the alveolar bony socket has been measured at between zero, if ankylosed, and 0.2mm. This small amount of movement may decrease during the day with mastication, and teeth will move slightly both horizontally and vertically. Exceeding this distance will fracture intact periodontal ligament fibers and allow macroscopic visually detectable vertical movement. With some coronal alveolar bone loss, lateral movement is feasible on natural teeth, but the remaining intact periodontal ligament will constrain vertical movement in the socket. With successful Osseo integrated implants, there is a fusion between bone and implant, a type of induced ankylosis; this must be intact, and no detectable movement is a positive sign of success. However, any movement, (vertical or horizontal) on an OI indicates the necessity for removal and possible replacement [5,4].
“When finding a lesion, and you do not recognize it, refer to a specialist.” Modern dentists are trained to develop their observation skills. Although the dentist’s major focus will be on the mouth, general observation of the entire patient is a highly desirable acquired skill. Overall observation will reveal much about the patient and frequent co-morbidities of the face and exposed parts of the arms, hands, head and neck may be detected. It is not unusual for dentists to refer patients to dermatologists for suspected skin lesions like keratoacanthomas, nevi or basal cell carcinomas on the face. Not only does this clinical acumen apply to corporeal, facial and peri-oral observations, but for all Oral Health Care Workers (OCHWs) act as screening doctors to detect intra-oral cancer and other intra- and peri-oral pathologies [5].
“You see what you look for and recognize what you know”: There are at least ten subspecialties to the dental profession. It is virtually impossible to know everything. That is the prime motivation for establishing subspecialties in the practice of dentistry. The longer professional OHCW’s practice and the more they study, so too does their knowledge, experience, judgment, insight and recognition of challenges and problems increase. Ongoing professional development after graduation is essential for ongoing improvement of dentistry. 5 In practice OHCW’S will manage lesions and situations arising with which they are familiar and treat them according to evidence based teaching. The amount of personal knowledge accumulated applied and used, determines experience and judgment, and clinical acumen for diagnosis should improve exponentially after qualifying to practice as a professional. Recognition of a something facilitates recall and eases mentally remembering differential diagnoses. Should something be missed in an orofacial examination, it is because the examiner either does not know what they are looking for or does not recognize a lesion because they do not know what it is. Accordingly, “You see what you look for and recognize what you know.”
“For a definitive diagnosis, take a biopsy for histopathology.” Presenting lesions often may be something unexpected. Macroscopic appearances are deceptive, especially in the mouth as the effects of saliva, chewing and ingested food may cause changes in presentation. Accordingly, taking an incisional (partial) or excisional biopsy for histopathology will determine the exact diagnosis and ensure mistakes are avoided [5].
“Is it Ruboffable?” This question (pronounced in one word with the accent on the second syllable …rub-BOFFable) is used when assessing white lesions in the mouth. If the presenting condition can easily be rubbed off, it is advisable to look at the offscouring under the microscope. More often than not, it will reveal some Candida fungal hyphae and or spores: staining with a dye like toluidine blue, iodine, or erythrosine highlights the diagnosis. If the white lesion is adherent to its base and does not easily rub off, a wider differential diagnosis is indicated. The differential diagnosis could include anything from frictional keratosis to leukoplakia with severe dysplasia. Again, taking an incisional or excisional biopsy for histopathology will determine the exact diagnosis [5].
“The ODD principle”: Recognizing any tissues within the range of normal is an acquired clinical skill which is honed into the armamentarium of accurate diagnosis. If something appears abnormal or different it warrants further investigation. Any “Other demonstrable Differences” (ODD) implies some pathology exists and has to be investigated accurately diagnosed for effective management and /or therapy. If something is noticed that is odd, ‘The ODD principle’ as an aphorism applies [6].
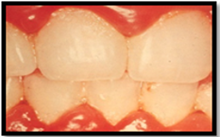
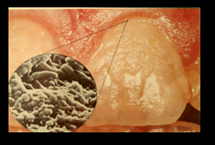
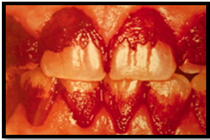
“Show Up the Plaque”: Oral biofilm is the accumulation of planktonic or sessile microbial plaques in the mouth. Stagnant sessile plaques developing on teeth and gingivae have been clearly shown to be the major cause of tooth decay and gum diseases. Because caries and gingivitis/periodontitis are the most prevalent global diseases of Mankind, and a major cause of morbidity, plaque control through oral hygiene and professional care have evolved as the main prophylactic measures to prevent tooth-decay and gum disease, and to sustain the whole dentition in good health well into old age. Accordingly, to identify the biofilm microbial plaque, disclosing solutions are used. Disclosing solutions can be used professionally and at home to facilitate plaque removal and sustain behavioral rituals. Colored dyes or luminescent liquid with ultraviolet light may be used to demonstrate exactly where the biofilm is located, and subsequent removal is facilitated through oral hygiene methods [7,8]. See Figures 1-A, B, C, D.
A
B
c
D
Figure A-B-C-D: ‘Show up the plaque’: A. Biofilm is usually not visible. B. However the biofilm is constituted by microbial colonies. C. Disclosing dyes reveal Biofilm presence. D. Tooth-brush, Toothpaste and dental-floss are the most common and ubiquitous paraphernalia for home-plaque removal [8].
“Assumption is the mother of all foul-ups”. When practicing dentistry, mistakes should never happen or at worst must be kept to an absolute minimum. One serious mistake is one too many. Especially in communication with patients relating to procedures which are finite and irreversible like exodontias or giving injections. That is why a comprehensive Medical History should be presented to patients, which should be a mandatory requirement to be completed by the patient themself, if possible before starting any therapy. Built-in protocols ensure correct optimal treatments are done. For example, when extracting a tooth, the operator should identify the tooth verbally; the assistant should repeat the verbal announcement, and the operator then checks the chart and re-affirms the decision. After selecting the appropriate forceps and placing the extraction forceps on the targeted tooth at the start, repeating the exact tooth by name and number will ensure no mistakes happen. Before administering any injection, the operator should check to confirm that the patient is not allergic to the injection material, in spite of information on the history sheet; a change may have happened after that medical-history was updated, and the operators should always check for themselves. A detailed Treatment Plan should include all the costs of proposed treatments and patients should be made aware of these costs. Confirming that the patient understands why therapy is diagnosed, why it is necessary, and the cost involved ensures a minimum of misunderstanding, resentment, surprises and challenges arising relating to payment. Quote the costs of therapy in writing for the patient before doing any treatment. Don’t assume patients know or will accept the fees linked to therapy. This may not be possible in emergencies, or if the patient is unconscious (by accident or general anesthetic). Once the patient is awake and fully compus-mentis, the necessity for treatment should be explained and the costs and expected payment incurred must be discussed. Options of treatment, costs, time and selection of material should be fully discussed with patients, including the arrangements made for patients to meet their obligations, …. All before commencing treatment. It is always good policy to check facts and data because “Assumption is the mother of all foul-ups”, and action based on assumption rather than evidence, may lead to tragedies and disasters.
Discussion
All these aphorisms apply basic principles that dictate policy for Oral Health Care Workers (OCHW). There are several subspecialties in Dentistry: Preventative Dentistry: Confirmative and Restorative: Prosthodontics; Periodontics; Oral Medicine; Orthodontics; Community dentistry: Oral Pathology; Maxillo-facial Surgery: Maxillo-facial Radiology, Orthognathic surgery, as well as complimentary services of Microbiology, Virology, Parasitology, Dental mechanics and technical services for processing adjuncts like castings or computer generated and/or influenced inlays, overlays and on lays, crowns, bridges, splints, and prostheses. Each will produce its’ own guiding principles and further aphorisms are sure to evolve. OCHW’s have access to all these modalities to optimize their diagnosis, treatment and service, and professional communication often involves speaking an applied aphorism. Costs of back-up specialist apparatus and supportive machines may coerce these services to be placed into group- practices, and/or often they may only be available in hospitals to maximize frequency of use, to amortize their costs and to keep professional fees as low as possible. Practicing Health Care workers must never assume all is in order or will be within health limits. Checking, confirming information and continual observation and vigilance will minimize, even optimize, outcomes of practicing dentists.
Conclusion
OTA’s have been inherited from succedaneous progressive generations of dentists; those reported here may be supplemented in future as long as dentistry evolves as a profession to produce more accumulating wisdom among dental health care workers.
Abbreviations
OI = Osseointegrtaed Implant
ODD = Other Demonstrable Differences
OHCW = Oral Health Care Workers
OTA = Orally Transmitted Aphorisms
Authors statement
The author has no conflict of interests to declare.
References
- Touyz L. Z. G. (2023). Orally Transferred Aphorisms of Dentistry. Dentistry and Oral Health Care, BRS Publishers, 2(2).
Publisher | Google Scholor - Bradley R.M. (1982). in: Basic Oral Physiology. Ch 9; Pain from Dental Structures, 172-118.
Publisher | Google Scholor - Gutman J. (2009). The Evolution of America's Scientific Advancements in Dentistry in the Past 150 Years.,1-46.
Publisher | Google Scholor - Goyal S., Masood M., Le C., Rajendran Y., Nanjapa S., Vaderhobli R. (2021). Comparative Bone Graft Evaluation for Dental Implant Success: An Evidence-Based Review. J Long Term Eff Med Implants, 31(3):33-44.
Publisher | Google Scholor - Laskaris G. (1988) in: Color Atlas of Oral Diseases. Fungal Infections, 77:138-148.
Publisher | Google Scholor - Touyz .(2011). Alternative Medicine and the ‘ODD” principle. Current Oncology, 19: 64-65.
Publisher | Google Scholor - Touyz L.Z.G. (2017). The Pathophysiology of Oral Biofilms and it’s relation to Initial Gum Disease and Caries. J Dent Oral Disord Ther, 5(4):1-6.
Publisher | Google Scholor - Arnim S.S. (1963). The Use of Disclosing Agents for Measuring Tooth Cleanliness. The Journal of Periodontology, 34(3):227-230.
Publisher | Google Scholor