case report
Metachronous Ovarian Cancer after a Radical Hysterectomy with Ovarian Conservation for Early-Stage Cervical Cancer: A Case Report
- Colman Mayomba 1
- Godfrey Kaizilege 1
- Richard Kiritta 1
- Dismas Matovelo 1
- Patrick Ngoya 2
- Oscar Ottoman 3
- Edgar Ndaboine 1*
1Department of Obstetrics and Gynecology, Bugando Medical Centre, Catholic University of Health and Allied Sciences, Mwanza, Tanzania.
2Department of Radiology, Bugando Medical Centre, Catholic University of Health and Allied Sciences, Mwanza, Tanzania.
3Department of Pathology, Bugando Medical Centre, Catholic University of Health and Allied Sciences, Mwanza, Tanzania.
*Corresponding Author: Edgar Ndaboine,Department of Obstetrics and Gynecology, Bugando Medical Centre, Catholic University of Health and Allied Sciences, Mwanza, Tanzania
Citation: Mayomba C, Kaizilege G, Kiritta R, Matovelo D, Ndaboine E, et.al. (2023). Metachronous ovarian cancer after a radical hysterectomy with ovarian conservation for early-stage cervical cancer: a case report. International Journal of Medical Case Reports and Reviews, BRS Publishers. 2(4); DOI: 10.59657/2837-8172.brs.23.023
Copyright: Edgar Ndaboine, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 14, 2023 | Accepted: June 28, 2023 | Published: July 31, 2023
Abstract
Introduction: Cervical cancer is the fourth most common disease in women worldwide and the leading cause in Tanzania, with 9,772 new cases and 6,695 deaths annually. Surgery is better than radiation or chemotherapy for early-stage cervical cancer (stages IA2–IIA1). Due to the risks of oophorectomy in young women, ovarian conservation is crucial. Metachronous ovarian cancer is understudied, however, ovarian conservation does not enhance cervical cancer mortality. Clinical presentation: We report a rare case of recurrent metachronous ovarian cancer in a 42-year-old female, Para 3, Living 3, who had her ovaries conserved following a radical hysterectomy and bilateral lymph node dissection for stage IB2 cervical cancer at 37 years old in April 2017. The final biopsy showed a well-differentiated, invasive cervical adenocarcinoma. Stage IV ovarian cancer with significant ascites and pleural effusion was detected in July 2018, 14 months post-surgery. Six chemotherapy treatments and total tumor debulking succeeded. Despite the most effective cytoreduction surgery, the patient experienced two further recurrences in 2020 and 2022. After additional surgeries and chemotherapy, she is currently in complete remission and will be followed up.
Conclusion: Young women undergoing radical hysterectomy for early-stage cervical cancer must preserve their ovaries, but metachronous ovarian cancer is a risk. Thus, metachronous ovarian cancer risks, challenges, and outcomes must be understood.
Keywords: metachronous cancer; cervical cancer; ovarian cancer; ovarian conservation; case report
Introduction
Metachronous tumors are defined as two (or more) separate primary malignancies that appeared more than six months after the first malignancy was diagnosed. These might occur in the same or distinct organs [1]. Young women with stage I cervical cancer who underwent surgery are very unlikely to develop metachronous ovarian cancer; the likelihood of this happening is less than 1% [2]. Due to this rarity, little is known about the disease course and outcome of women diagnosed with such cancers. However, ovarian conservation does not increase mortality of cervical cancer and also ovarian conservation is very important in young premenopausal women because oophorectomy is associated with adverse effects in this young group [3]. We report a rare case of recurrent metachronous ovarian tumor in a 42-year-old female who had ovaries conserved after radical hysterectomy and bilateral pelvic lymph nodes dissection due to stage IB2 cervical cancer so as to re-emphasize the need for meticulous follow-up of patients after surgery in a resource-limited setting. Approaches to management, risk factors, and literature review will also be discussed.
Patient Information, Diagnostic Assessment and Therapeutic Intervention
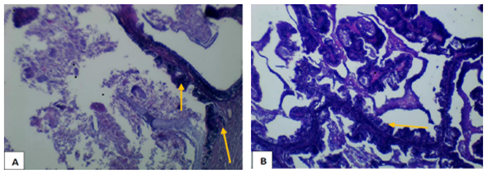
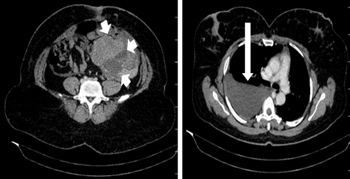
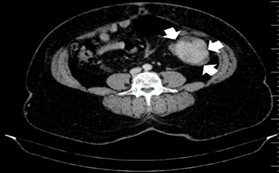
A 42-year-old woman, para 3, living 3, was diagnosed with cervical cancer stage 1B2 in April 2017 at the age of 37. She underwent radical hysterectomy and bilateral pelvic lymph node dissection in the same year; both ovaries were preserved as they appeared healthy. A final biopsy revealed a well differentiated invasive adenocarcinoma of the cervix and a histological report revealed all dissected pelvic nodes and the parametrium were free from malignancy. The tumor was 3 cm in size, limited to the uterine cervix and no lymphovascular invasion (LVI). She was then kept on three-monthly follow-ups, during which she remained without evidence of a recurrence of cervical cancer. Unfortunately, she had abdominal distention, chest pain, and difficulty breathing one year later (14 months post-surgery) in July 2018. This necessitated a quick assessment at our facility. She exhibited stable vital signs, somewhat dyspneic and enlarged abdomen, and a right complex solid pelvic mass with limited mobility. A vaginal examination indicated no abnormalities. A chest, abdomen, and pelvic computed tomography (CT) scan showed a right pleural effusion with normal lung fields, a solid right ovarian tumor with significant ascites, and normal liver and spleen. Additionally, serum CA 125 levels were raised to 800 U/ml (normal range 0-35). The ultrasound-guided biopsy of the ovarian mass revealed a well-differentiated adenocarcinoma. She then underwent complete tumor debulking surgery preceded by six cycles of neoadjuvant chemotherapy (a combination of carboplatin and paclitaxel). During the surgery, a 6x6 cm solid right ovarian tumor attached to the back of the pelvic wall was found, and the right ureter was very close to the tumor. Total tumor debulking and removal of the contralateral ovary were performed together with the total omentectomy and appendicectomy. There were no signs of residual disease left, and the vaginal stamp was normal. According to the final histopathology report, both ovaries had mucinous cystadenocarcinoma and the omentum was disease-free. After treatment, CA 125 levels returned to normal at 27U/ml. Despite the optimal cytoreductive surgery, the patient experienced another 2 episodes of recurrences in 2020 and 2022, respectively and was managed accordingly with six cycles of chemotherapy followed by secondary debulking surgery in all recurrent episodes. Her histological biopsy revealed the mucinous papillary cysta-adenocarcinoma (Figure 1). The most recent surgery, performed in May 2022, revealed a 5x7 cm confided mass in the pelvis, which was removed surgically after 6 cycles of chemotherapy (Figure 2). The CT imaging of the patient following a year 2022 recurrence of ovarian cancer prior to neo-adjuvant chemotherapy is revealed in Figure 3, with the CT control after 6 cycles of chemotherapy and prior to surgery in Figure 4. Indicating severe right pleural effusion, ascites, and a huge left lower abdominal mass prior to treatment and the disappearance of pleural effusion, ascites, and a significant reduction in tumor size after chemotherapy.
Figure 1: (A) Showing invasive papillary adenocarcinoma infiltrate the capsule pointed by yellow arrow (x10 HPF). (B) Showing papillary arrangement lined by neoplastic columnar cell with mucin secretion pointed by yellow arrows (x 40 HPF) (H&E stain).
Figure 2: Gross specimen of the surgically resected left flank mass.
Figure 3: Contrasted CT axial soft tissue dense window images prior to chemotherapy, demonstrating a left iliac fossa enhancing intra-abdominal intra-peritoneal mass with posterior area of necrosis and lobulated margins on the left (short white arrows) and right sided pleural effusion (long white arrow).
Figure 4:Contrasted CT axial soft tissue dense window image post-chemotherapy, demonstrating a residual left flank enhancing intra-abdominal intra-peritoneal mass with lobulated margins on the left (white arrowheads). Right sided pleural effusion had completely resolved (image not shown).
Follow Up And Outcomes
However, in all recurrences, the patient was found in stage IV of the disease with pleural effusion, abdominal mass (as displayed in Figure 3), and an elevated CA 125. She is currently 9 months post 4th relaparotomy for recurrent ovarian cancer, in addition to the first radical hysterectomy. She is currently disease-free with neither ovarian cancer nor cervical cancer, and she is on surveillance follow-up.
Discussion
Cervical cancer is the fourth most prevalent cancer in women worldwide, with an estimated 500,000 new cases and 250,000 fatalities per year [4]. There are an alarming 9,772 new cases of cervical cancer and 6,695 fatalities from the disease per year in Tanzania [5]. Surgery is preferred over radiation with or without chemotherapy for the treatment of early-stage cervical cancer (stages IA–IIA). The stage of the disease determines the type of surgery, whether extrafacial, modified radical, or radical hysterectomy with pelvic-lymphadenectomy [6]. In early-stage cervical cancer, having primary radiation with or without chemotherapy is associated with a decreased quality of life (poor bowel function, urinary incontinence, sexual dysfunctions, and pelvic pain) than having primary surgery [7]. Primary radiation therapy with or without chemotherapy in early stage cervical cancer is reserved for patients who are not surgical candidates due to medical comorbidities, poor functional level, or inadequate health resources [6]. We chose a radical hysterectomy and pelvic lymphadenectomy with ovarian preservation over chemoradiation since the patient was diagnosed with cervical cancer stage IB2, was young, and sexually active. Ovaries were spared because they appeared healthy during surgery and to protect ovarian function. Young women who have had surgery for early-stage cervical cancer usually need to keep one or both of their ovaries. This is because there is more and more evidence that removing both ovaries can cause surgical menopause. The loss of the cardio-protective benefits of ovarian hormones, notably estrogen, has also been shown to significantly raise the risk of cardiovascular disease morbidity and mortality in young premenopausal women who undergo early oophorectomy [3]. Ovarian preservation during hysterectomy for young women with early-stage cervical cancer is not associated with cervical cancer mortality (0.5% for stage I squamous type and 3% for stage I adenocarcinoma type), despite the fact that ovarian involvement from cervical cancer is a concern [8]. Therefore, it is beneficial to try to protect the ovary, provided that doing so does not result in a rise in the mortality rate from cervical cancer. We decided not to remove the patient's ovaries during her initial surgery for early-stage cervical cancer because of her young age and our concerns about the effects of surgical menopause on her. Although our patient's recurrent metachronous ovarian cancer was successfully treated, this is an extremely unusual occurrence, and the risk factors for cervical and ovarian cancer are distinct. It wasn’t very clear whether this was a metastatic disease from the cervix or a new primary ovarian cancer; in the literature, mucinous epithelial ovarian cancer is commonly a metastatic disease [9]. Approximately 80% of mucinous ovarian carcinomas (MOC) are metastatic, while 80% of original tumors are stage I. The most common main sites that metastasis to the ovary are the gastrointestinal system (45%), pancreas (20%), cervix and endometrial (18%), and breast (8%) [9]. As it is histologically extremely similar to other mucinous carcinomas, particularly colorectal carcinoma, the diagnosis of primary MOC necessitates thorough pathological evaluation. Recognizing the microscopic characteristics and comprehending the immunohistochemistry (IHC) profile of MOC is crucial for establishing a definitive diagnosis, which leads to the provision of appropriate treatment and an accurate prognosis [9]. Our patient had no endometrial, breast, or gastrointestinal malignancy; furthermore, we were unable to undertake IHC to validate the originality of the disease; hence, we continue to assume that this was an entirely new ovarian cancer. After ovarian preservation, the incidence of metachronous ovarian cancer in women with stage I cervical cancer is less than 1%. Adenocarcinoma histology, adjuvant radiation, older age, and non-White ethnicity are all linked to an increased risk of metachronous ovarian cancer [2]. The only risk our patient had for metachronous ovarian cancer was that it was adenocarcinoma; she was young and had never been treated with radiotherapy; as a result, it is extremely difficult to predict. Even though there is an increasing push toward ovarian conservation at the time of surgery for young women with early-stage cervical cancer, not much is known about the challenges involved and the risk of getting ovarian cancer again after ovarian conservation [2]. Our patient developed recurrent metachronous ovarian cancer and was successfully managed with three surgeries, and every major surgery was preceded by neo-adjuvant combination chemotherapy, luckily, she has been platinum sensitive in all relapses because she had a platinum-free interval (PFI) of more than 6 months. Literatures reports that there is a significant benefit for secondary surgical cytoreduction in recurrent ovarian cancer due to prolonged survival with surgery compared to the use of combination salvage chemotherapy without surgery [10]. This is clear in our patient, who has had recurrent ovarian cancer for the past 5 years despite earlier operations and chemotherapy. Cancer that recurs is difficult to treat in Tanzania, where resources are scarce. According to reports, there are few oncologists in the country, and even fewer gynecologic oncologists. This woman is fortunate to have survived for more than 5 years with two cancers since she was treated at our hospital, Tanzania's only tertiary hospital offering comprehensive cancer care along the Lake Zone [5]. This is the first time that metachronous ovarian cancer following radical hysterectomy for cervical cancer has been reported at our center or in Tanzania in general. When performing a radical hysterectomy for cervical cancer in its early stages, it is crucial to consider the risks and benefits of ovarian preservation.
Conclusion
Ovarian preservation is critical in young women undergoing radical hysterectomy for early-stage cervical cancer but fraught with risk of metachronous ovarian cancer. Hence, it is crucial to know the risks, challenges, and outcomes of metachronous ovarian cancer.
Patient’s perspective
The care given was prompt, and a follow-up plan was detailed along with a thorough description of the diagnosis and prognosis.
Acknowledgments
The Obstetrics/Gynecology, Pathology, and Radiology Departments of Bugando Medical Centre (BMC) and Catholic University of Health and Allied Sciences, Tanzania (CUHAS) have generously supported and encouraged us, and we sincerely appreciate it.
Timeline
The patient was admitted for the first time in 2017 and all the management were done timely on all her recurrent episodes of cancer relapse. She is currently on surveillance to see if there will be any relapse.
Author’s Contribution
CM, GK, RK, DM, PN, OO, and EN contributed equally to the creation of this case report. CM prepared the initial draft of the case; GK, RK, DM, and EN participated in the management of the patient; PN interpreted radiological imaging; and OO reviewed pathological reports. CM and EN reviewed the literature and finalized the manuscript. All authors read and approved the final manuscript.
Funding
This patient's medical insurance paid for all of the services rendered to her. The authors and the Catholic University of Health and Allied Sciences shared the expense of putting this manuscript together.
Ethical approval and consent to participate
The patient provided written informed consent in order for this case report to be published, and the collaborative Catholic University of Health and Allied Sciences/Bugando Medical Centre Research and Ethical review board gave its approval.
Consent for publication
The patient gave written approval to publish this case and associated photograph. The Journal Editor-in-Chief can review the written consent. This work was also approved by the Catholic University of Health and Allied Sciences Directorate of Research and Publication. The Journal Editor-in-Chief can also review the clearance document.
Competing interests
The authors report having no competing interests.
References
- De Luca A. et al. (2019). Breast cancer and multiple primary malignant tumors: case report and review of the literature. in vivo, 33(4):1313-1324.
Publisher | Google Scholor - Matsuo, K, et al. (2017). Risk of metachronous ovarian cancer after ovarian conservation in young women with stage I cervical cancer. American journal of obstetrics and gynecology, 217(5): 580-590.
Publisher | Google Scholor - Lyu. J, T. Sun, and X. Tan. (2014). Ovarian preservation in young patients with stage I cervical adenocarcinoma: a surveillance, epidemiology, and end results study. International Journal of Gynecologic Cancer, 24(8).
Publisher | Google Scholor - Arbyn M. et al. (2020). Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. The Lancet Global Health, 8(2):191-203.
Publisher | Google Scholor - Runge A.S, et al. (2019). Cervical cancer in Tanzania: A systematic review of current challenges in six domains. Gynecologic oncology reports, 29:40-47.
Publisher | Google Scholor - Abu-rustum NR, A.S, Cripens MA, Dupont N,et al. (2021). Clinical Practice Guidelines in Oncology. National institute of Health.
Publisher | Google Scholor - Elghamrawi K.A, M.H. Haggag, and E.E. Habib. (2011). Treatment complications among long-term survivors of cervical cancer: treated by surgery or radiotherapy. Oncology Reviews, 5:261-266.
Publisher | Google Scholor - Shimada M., et al. (2006). Ovarian metastasis in carcinoma of the uterine cervix. Gynecologic oncology, 101(2):234-237.
Publisher | Google Scholor - Babaier A. and P. (2020). Ghatage, Mucinous cancer of the ovary: overview and current status. Diagnostics, 10(1):52.
Publisher | Google Scholor - Munkarah A. and R. (2004). Coleman, Critical evaluation of secondary cytoreduction in recurrent ovarian cancer. Gynecologic oncology, 95(2):273-280.
Publisher | Google Scholor