Research Article
Maternal Healthcare Services Utilization and Associated Factors among Childbearing Age of Women in Liben District, East Borena Zone, Oromia Regional Health Bureau, Ethiopia
1Negelle Borena Health SciencesCollege, Department of Public health,East Borena Zone, Oromia regional Health Bureau, Ethiopia.
2Adama Hospital Medical College, Department of Public Health, Oromia regional Health Bureau, Ethiopia.
*Corresponding Author: Godana Arero, Adama Hospital Medical College, Department of Public Health, Oromia regional Health Bureau, Ethiopia.
Citation: Desta M, Serawit Mengistu S., Arero G. (2024). Maternal Healthcare Services Utilization and Associated Factors among Childbearing Age of Women in Liben District, East Borena Zone, Oromia Regional Health Bureau, Ethiopia, Journal of BioMed Research and Reports, BioRes Scientia Publishers. 4(2):1-11. DOI: 10.59657/2837-4681.brs.23.057
Copyright: © 2024 Godana Arero, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 28, 2023 | Accepted: December 29, 2023 | Published: January 19, 2024
Abstract
Background: Utilization of maternal healthcare services is a fundamental health intervention for preventing maternal morbidity and mortality. Despite its importance, the utilization of maternal healthcare services in Ethiopia is low, especially in rural pastoralist communities. Thus, this study aimed to assess maternal healthcare services utilizations and its associated factors in the Liben district of Guji zone, Oromia region, Southern Ethiopia.
Methods: A community-based cross-sectional study was conducted with 416 randomly identified mothers in Liben in September, 2020. The respondents were mothers who had given birth 12 months prior to the survey. The data were collected using interviewer administered questionnaires. The data were entered into Epi-data version 4.1 and analyzed using SPSS version 20. Descriptive, bivariate and multivariate logistic regression analyses were also performed.
Result: Sixty percent of mothers had received antenatal care at least once. In this study, only 21.2% and 17.5% of women had delivered their babies at health institutions and utilized early postnatal care services respectively. Maternal education [AOR=2.43(95%CI: 1.22–4.89)], decision making power [AOR=2.40(95% CI: 1.3–23.3)], perceived compassionate & respectful care [AOR=0.30(95%CI: 0.18–0.50)], and planned current pregnancy [AOR=0.22(95% CI: 0.12–0.37)] were significantly associated with utilization of antenatal care. Mother’s age [AOR=3.73(95% CI: 1.53–6.04)], time to travel to health facilities [AOR=1.74(95% CI:1.02– 3.08)], knowledge of danger signs [AOR=3.77(95% CI:2.16–6.57)] and perceived compassionate and respectful care were significantly associated with institutional delivery, whereas recent antenatal care utilization[AOR=5.34(95%CI:1.96–8.65)], planned current pregnancy and knowledge of danger signs [AOR=2.93(95%CI:1.59–5.41)] were found to be significantly associated with postnatal care utilization.
Conclusion: Overall, the prevalence of maternal healthcare services utilization was far below the national and regional targets in the study area. Therefore, considering the identified associated factors and providing information and training on these issues to the community could improve and sustain maternal healthcare services utilization.
Keywords: liben district; maternal healthcare service utilization; antenatal care; institutional delivery; postnatal care
Introduction
Every year, an estimated 289,000 women die during pregnancy and, childbirth, or soon after worldwide, 2.6 million women suffer stillbirths and 2.9 million infants die in the first month of life. Developing countries account for 99% of global maternal deaths. Sub-Saharan Africa alone accounts for 62% of the global burden of maternal death. In less developed countries, poor women in remote areas are least likely to receive adequate maternal healthcare services. Although most maternal deaths are avoidable, African women face unequal risks of death or disability due to pregnancy and childbearing simply because of where they live [1-4]. The large number of maternal deaths that occur during labor, delivery, and in the first couple of days after childbirth, specifically in low and middle-income countries, is due to the low level of maternal healthcare service utilization. Proper care during pregnancy and delivery is important for the health of both the mother and baby. The provision of skilled care during pregnancy, childbirth, and the postpartum period, preferably at a healthcare facility, is vital. For optimum safety, every woman, without exception, needs professional skilled care when giving birth in an appropriate environment that is close to where she lives and respects her birthing culture [4-6].
The low utilization of maternal healthcare services is a great challenge in most low-resource settings, and Ethiopia is no exception. Despite the government’s commitment to delivering healthcare facilities to the doorsteps of the common people through the Health Extension Service Package (HESP), the country has faced challenges in increasing utilization of good quality maternal healthcare services. Healthcare services and facilities are inadequate and poorly equipped in remote pastoral areas of Ethiopia. The few existing health centers are not adequately equipped with basic medicaments, equipment, and supplies [7-9]. A previous study clearly demonstrated that utilization of available maternal healthcare services is also very low in Brazil. According to a recent mini-Ethiopia Demographic Health Survey (EDHS) 2019 report, 70% of rural women received at least one antenatal care (ANC) visit from a skilled provider, including health extension workers. Only 40% and 29% of rural women delivered at health facilities and received early postnatal care, respectively [10]. In general, the utilization of maternal healthcare services is a complex behavioral phenomenon influenced by several factors at both individual and community levels. Therefore, to improve maternal and child health, barriers limiting the utilization of maternal healthcare services must be identified and addressed at all levels of the healthcare system. Thus, the purpose of this study was to understand the current status of the utilization of maternal health care services by elucidating the various factors influencing the use of these services in the study area.
Methods
Study setting, design and population
A community-based, cross-sectional study was conducted among childbearing women who had given birth in the 12 months prior to the survey of residents of Liben district, Guji Zone, southern Ethiopia. The total population of the district is 191,494 people, of whom 95,195 are women. The estimated total number of women of reproductive age in the district is 19,990. Six health centers and 16 health posts are available in the district. This study was conducted from 15 to 23 September 2020.
Sample size and sampling technique
The required sample size of eligible mothers was determined using a single-population proportion formula. The following assumptions were made: the proportion of institutional delivery in the rural community of Oromia region, according to the mini-EDHS-2019 report, was 40% [10], with a 95% confidence level, a 5% margin of error, and an expected 10% non- response rate. The final sample size was calculated to be 416. The participants were selected using the following steps: first, six rural kebeles (the smallest administrative unit) were selected from the 16 kebeles in the district using a simple random sampling technique. The census was carried out in the selectedkebeles to identify motherswho had given birthin the year prior to the survey. The proportional distribution of the sample size for each selected kebele was determined. Finally, mothers were selected using a systematic random sampling method.
Inclusion and exclusion criteria
Women who hadgiven birth in the last 12 months and had been residentsof the Liben district for at least six months were included. Mothers who were critically ill and unable to respond to interview were excluded.
Operational definition
Maternal healthcare services include antenatal, delivery, and postnatal care services.
Antenatal care: refers to care received from healthcare professionals at least once during pregnancy.
Institutional delivery refers to childbirth either in public or private healthcare facilities attended by skilled attendants such as midwives, nurses, doctors, and health officers.
Postnatal care refers to care given to mothers after childbirth by healthcare professionals in the first 48 hours after delivery at a health facility.
Data collection tool and method
Quantitative data were collected using a structured and semi-structured questionnaire. The questionnaire was based on a review of relevant previous studies and literature. Face-to-face interviews were conducted at respondents’ homes. The main contents of the tool included socio- demographic characteristics, maternal obstetric characteristics, health facility-related factors, and maternal healthcare service utilization.
Data management and quality
After extensive revision, the final version of the English questionnaire was translated into the local language and then back into English for consistency. Then, the tool was pretested on 5% of a similar population in Hare-kello town, 25km from the actual study setting. Six diploma nurses who were fluent in speaking local languages were involved in data collection. Two BSc healthcare professionals were recruited as supervisors. All data collectors and supervisors were trained for two days during the data-collection process, based on the guide developed by the principal investigator. The principal investigators and supervisors monitored each activity closely and provided further clarification and support to the data collectors. The data were checked daily for missing information and inappropriate responses. Then, the data were cleaned and entered into Epi Data version 4.1 and analyzed using SPSS version 20.
Statistical analysis
Summary statistics of means and percentages were used to describe the study population. Bivariate and multivariate logistic regression analyses were performed to identify associations between independent and outcome variables. Variables with a p-value of ≤0.25 on bi-variable regression analysis were further entered into the multivariable binary logistic regression model to control for possible confounding variables. The Hosmer–Lemes how test was used, and the model adequately fit the data at a p-value of >0.05. Multi-collinearity between the independent variables was assessed using a variance inflation factor of less than 10. Crude and adjusted odds ratios with 95% CI were used to determine the strength of association between the outcome variables and independent variables. Statistical significance was set at p less than or equal to 0.05.
Results
Socio-demographic characteristics
A total of 416 women of reproductive age who had given birth in the year prior to the survey were interviewed, with a response rate 100%. Of these respondents, 261 (63%) were aged 20–34 years, with a mean (+SD) age of 26.5(±6.5) years. Of study participants, 399(96%) were married. The dominant ethnic group was Oromo, which accounted for 84% of total respondents; 60% were Wake-feta (the indigenous religion of Oromo people) and 32% were Muslim. More than two-thirds (78%) had never attended school and most (85%) were housewives. Regarding decision-making regarding maternal healthcare service utilization, the majority (61%) reported that such decisions were made jointly by husband and wife (Table 1).
Table 1: Socio-demographic Characteristics of the Study Participants in Liben District, Southern Ethiopia, September, 2020 (n=416).
| Socio-demographic characteristics | Frequency | Percentage | |
| Age of respondents | 15 – 19 years | 91 | 22 |
| 20 – 34 years | 261 | 63 | |
| 35- 49 years | 64 | 15 | |
| Marriage Status | Currently Married | 399 | 96 |
| Divorced & widowed | 17 | 4 | |
| Wake-Feta | 250 | 60 | |
| Religion | Muslim | 134 | 32 |
| Christian | 32 | 8 | |
| Ethnicity | Oromo | 322 | 83.7 |
| Somali | 89 | 21 | |
| Others | 5 | 1.3 | |
| Women Education | No Education | 330 | 78 |
| Primary & above | 86 | 22 | |
| Husband education | No Education | 270 | 65 |
| Primary& above | 146 | 35 | |
| House Wife | 352 | 84.6 | |
| Women occupation | Merchant | 35 | 8.4 |
| Civil Servant | 17 | 5.1 | |
| Students | 12 | 2.9 | |
| Poor | 152 | 37.6 | |
| Family wealth index | Medium | 133 | 32 |
| Rich | 131 | 31.4 | |
| Family size | 1-3 | 29 | 7 |
| 4- 5 | 128 | 31 | |
| 6 & above | 259 | 62 | |
| Decision maker for MHSU | Women alone | 60 | 14 |
| Husband alone | 101 | 25 | |
| Jointly husband &wife | 255 | 61 | |
| Travel time to health facility | < 1hour | 210 | 51 |
| >1hour | 206 | 49 | |
| Access to emergency ambulance | Yes | 142 | 34 |
| No | 274 | 66 |
Table 2: ObstetricCharacteristic of the Study Participants, Liben District, Southern Ethiopia, September, 2020, (n=416).
| Variable | Frequency | Percentage (%) | |
| Age at first pregnancy | >18 Years | 167 | 40 |
| 19-24 Years | 216 | 52 | |
| >25 Years | 33 | 8 | |
| Gravidity | 1 | 56 | 13 |
| 2-4 | 149 | 36 | |
| >5 | 211 | 51 | |
| Stillbirth history | Yes | 15 | 3.6 |
| No | 401 | 96.4 | |
| Abortion history | Yes | 11 | 2.6 |
| No | 405 | 97.4 | |
| Planned current pregnancy | Yes | 244 | 59 |
| No | 172 | 41 | |
| Attended ANC in last pregnancy | Yes | 249 | 60 |
| No | 167 | 40 | |
| Frequency of antennal care (n=249) | < 4> | 139 | 56 |
| >4 Visits | 110 | 44 | |
| First ANC Visit (n=249) | Before 16 Weeks | 61 | 25 |
| 16- 36 Weeks | 178 | 69 | |
| After 36 Weeks | 10 | 4 | |
| Place of last delivery | Home | 328 | 78.8 |
| Health Facility | 88 | 21.2 | |
| Utilized Postnatal care with 48 hrs | Yes | 73 | 17.5 |
| No | 343 | 82.5 | |
| Know at leastone danger signs | Yes | 163 | 39 |
| No | 253 | 61 | |
| Experienced severe illnessin last pregnancy | Yes | 105 | 25 |
| No | 311 | 75 | |
| Felt Clients Privacy is maintained at HF | Yes | 183 | 44 |
| No | 233 | 56 | |
| Is working time of HF is convenient | Yes | 331 | 80 |
| No | 85 | 20 | |
| Felt Compassionate and respectful health care at HF | Yes | 219 | 53 |
| No | 197 | 47 | |
| Main reason for last home delivery (328) | Long Distance Of HF | 156 | 47 |
| Wish To Deliverwith Family | 58 | 18 | |
| Prefer TBAs | 46 | 14 | |
| Not Trust HF | 39 | 12 | |
| Others | 29 | 9 | |
Obstetric characteristics of respondents
Regarding obstetric history, 167 respondents (40%) became pregnant for the first time before the age of 19. Almost half (51%) had had five or more pregnancies. Fifteen women (3.6%) had experienced a stillbirth. For 244 respondents (59%), their most recent pregnancy was planned and intentional (Table 2).
Maternal healthcare services utilization
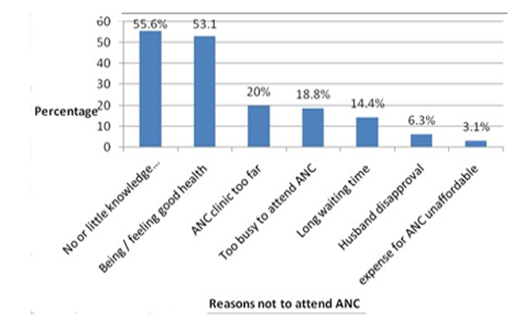
Of all respondents included in the study, 249(60%) had received at least one ANC service during their last pregnancy. Of these, 138 (55%) had received the service from health extension workers at healthcare clinics. Nearly 25% of the women made their first antenatal visit during the first 16 weeks of pregnancy. Among the ANC service users, 56% had made fewer than four antenatal visits (Table 2). Women cited different reasons for not attending ANC in their recent pregnancies. Little or no knowledge, a feeling of healthiness, a long distance from home to healthcare facilities, work overload at home, and long waiting times for services at healthcare facilities were the major reasons reported for not attending ANC services (Figure 1). Among respondents, only 88(21.2%) were delivered of their baby at a healthcare center/hospital with the assistance of skilled healthcare workers. The majority (78.8%) delivered at home with the assistance of a traditional birth attendant (TBA) and relatives. Women cited different reasons for wanting to deliver at home, such as long distance to healthcare facilities, wish to deliver in the presence of family, preferring TBAs, and not trusting healthcare facilities (Table 2). Regarding postnatal care service utilization, only 73(17.5%) of respondents received postnatal care services within 48 hours of delivery at a healthcare facility (Table 2). ANC: antenatal care, PNC: postnatal care, HF: Health facility. (Figure.1).
Figure 1: Reasons cited by the study participants for not attending ANC services, Liben district, Southern Ethiopia, September, 2020.
Table 2: Obstetric Characteristic of the Study Participants, Liben District, Southern Ethiopia, September, 2020, (n=416).
| Variable | Frequency | Percentage (%) | |
| Age at first pregnancy | >18 Years | 167 | 40 |
| 19-24 Years | 216 | 52 | |
| >25 Years | 33 | 8 | |
| Gravidity | 1 | 56 | 13 |
| 02-Apr | 149 | 36 | |
| >5 | 211 | 51 | |
| Stillbirth history | Yes | 15 | 3.6 |
| No | 401 | 96.4 | |
| Abortion history | Yes | 11 | 2.6 |
| No | 405 | 97.4 | |
| Planned current pregnancy | Yes | 244 | 59 |
| No | 172 | 41 | |
| Attended ANC in last pregnancy | Yes | 249 | 60 |
| No | 167 | 40 | |
| Frequency of antennal care | < 4> | 139 | 56 |
| (n=249) | >4 Visits | 110 | 44 |
| First ANC Visit (n=249) | Before 16 Weeks | 61 | 25 |
| 16- 36 Weeks | 178 | 69 | |
| After 36 Weeks | 10 | 4 | |
| Place of last delivery | Home | 328 | 78.8 |
| Health Facility | 88 | 21.2 | |
| Utilized Postnatal care with 48 | Yes | 73 | 17.5 |
| hrs | No | 343 | 82.5 |
| Know at least one danger signs | Yes | 163 | 39 |
| No | 253 | 61 | |
| Experienced severe illness in last pregnancy | Yes | 105 | 25 |
| No | 311 | 75 | |
| Felt Clients Privacy is maintained | Yes | 183 | 44 |
| at HF | No | 233 | 56 |
| Is working time of HF is | Yes | 331 | 80 |
| convenient | No | 85 | 20 |
| Felt Compassionate and | Yes | 219 | 53 |
| respectful health care at HF | No | 197 | 47 |
| Main reason For last home delivery (328) | Long Distance Of HF | 156 | 47 |
| Wish To Deliver With | 58 | 18 | |
| Family | |||
| Prefer TBAs | 46 | 14 | |
| Not Trust HF | 39 | 12 | |
| Others | 29 | 9 | |
Factors Associated with Maternal Healthcare Services Utilization
According to the multivariate logistic regression analysis, maternal education, decision-making power regarding maternal healthcare service utilization, perceived compassionate and respectful care at healthcare facilities, and planned current pregnancy were significantly associated with the utilization of ANC. Mothers who had completed primary and above education were 3.7 times more likely to utilize ANC services when compared to women with no education (AOR=3.69; 95% CI: 2.05, 6.62). Mothers who could decide on maternal healthcare services utilization with their husband were 2.4 times more likely to attend ANC visits than women who could not (AOR=2.4; 95%CI: 1.32, 3.34). Furthermore, women who perceived no compassionate and respectful care at healthcare facilities were 70% less likely to utilize ANC services than women who perceived compassionate and respectful care (AOR=0.30; 95% CI:0.18, 0.50). Respondents who had unplanned current pregnancies were 68% less likely to utilize ANC services when compared those who had planned their pregnancies (AOR=0.78; 95% CI: 0.12, 0.37) (Table 3).
Table 3: Bi-variable and Multivariable Analysis Results of Maternal Healthcare Service Utilization and its Associated Factors among Childbearing Age of Women in Liben District, September, 2020.
| Factors Associated with ANC Utilization | |||||
| Antenatal Care Utilized | COR &95% CI | AOR & 95% CI | |||
| Yes (n=249) | No n=167) | ||||
| Mother Education | No education | 179 | 151 | 1.00+ | 1.00+ |
| Primary& above | 70 | 16 | 3.69[2.05,6.62]* | 2.43[1.21,4.89]* | |
| Decision maker for MHSU | Women alone | 47 | 13 | 5.07[2.44,5.54]* | 4.91[1.93,6.56]* |
| Both Partners | 160 | 95 | 2.36[1.47,3.78]* | 2.40[1.32,3.34]* | |
| Husband alone | 42 | 59 | 1.00+ | 1.00+ | |
| Planned current pregnancy | Yes | 184 | 60 | 1.00+ | 1.00+ |
| No | 65 | 107 | 0.19[0.13,0.30]* | 0.22[0.12,0.37]* | |
| Compassionate & Respectful care | Yes | 168 | 51 | 1.00+ | 1.00+ |
| No | 81 | 116 | 0.21[0.14,0.32]* | 0.30[0.18,0.50]* | |
| Factors Associated withInstitutional Delivery | |||||
| Institutional Delivery | COR & 95% CI | AOR & 95% CI | |||
| Yes (n=88) | No (n=328) | ||||
| Maternal age | 15 – 19 years | 35 | 56 | 3.01[1.38,6.53] * | 3.73[1.53,6.04]* |
| 20 – 34 years | 42 | 219 | 0.92[0.44,1.91] | 0.88[0.39,1.98] | |
| 35- 49 years | 11 | 53 | 1.00+ | 1.00+ | |
| Travel time to HF | <1hr> | 55 | 155 | 1.86[1.14,3.01]* | 1.74[1.02,3.08] * |
| >1hrs | 33 | 173 | 1.00+ | 1.00+ | |
| Compassionate & Respectful care | Yes | 67 | 152 | 3.69[2.16,6.11] * | 2.93[1.58,4.40] * |
| No | 21 | 176 | 1.00+ | 1.00+ | |
| Knowledge of danger signs | Yes | 60 | 103 | 4.68[2.82,7.12] * | 3.77[2.16,6.57] * |
| No | 28 | 225 | 1.00+ | 1.00+ | |
| Factors Associated with Early PNC Utilization | |||||
| Postnatal Care Utilized | COR & 95% CI | AOR & 95% CI | |||
| Yes(n=73) | No(n=343) | ||||
| Recent ANC utilization | Yes | 68 | 181 | 12.1[3.51,19.6]* | 5.34[1.96,8.65]* |
| No | 5 | 162 | 1.00+ | 1.00+ | |
| Planned current pregnancy | Yes | 56 | 188 | 2.71[1.51,4.86]* | 2.19[1.07,4.41]* |
| No | 17 | 155 | 1.00+ | 1.00+ | |
| knowledge of danger signs | Yes | 52 | 111 | 5.17[2.97,6.01]* | 2.93[1.59,5.41]* |
| No | 21 | 232 | 1.00+ | 1.00+ | |
COR, crude odds ratio; AOR: Adjusted odds ratio; CI, confidence interval; MHSU, maternal healthcare service utilization; HF, health facility. *Significant at p-value less than 0.05, 1.00+Reference category.
The likelihood of delivering at a healthcare institution (health center and hospital) was 3.7 times more likely for mothers aged between 15–19 years than for those aged between 35–49 years (AOR=3.73;95% CI: 1.53,6.04). Regarding time to travel to a healthcare facility, mothers who could reach one within an hour were 1.74 times more likely to deliver there (a healthcare center or hospital) compared to those who live further away (AOR=1.74;95% CI: 1.02,3.08). Additionally, mothers who recognized at least one danger sign in pregnancy were 3.7 times more likely to deliver at a healthcare facility (healthcare center or hospital) compared to those who did not (AOR=3.77;95% CI: 2.16,6.57). Regarding early postnatal care utilization, attending antenatal services in recent pregnancy, planned pregnancy, and knowledge of danger signs in pregnancy were variables that showed an association with postnatal care utilization. Accordingly, those mothers who had attended an ANC visit in their last pregnancy were 5.3 times more likely to utilize early postnatal care services than those who had not (AOR=5.34; 95% CI: 1.96, 8.65). The likelihood of utilizing early postnatal care services was 2.2 times more likely for mothers who had planned their pregnancy than for those who had not (AOR=2.19; 95% CI: 1.07, 4.41).
Discussion
This study aimed to assess the level of maternal healthcare service utilization and it associated factors in Liben district, Oromia region, Southern Ethiopia. Evidence from the present study found that utilization of ANC was 60%. This finding is in agreement with a study conducted in Womberma district (64%) [13]. In contrast to the present findings, a study conducted in Enderta district (70%) and Kombolcha district (86%) reported higher utilization of ANC [11,20]. In this study, utilization of institutional delivery care was 21.2%. The majority of women (78.8%) delivered at home with the assistance of TBAs and relatives. This finding is consistent with the study conducted in rural Kombolicha (20.9%) [20]; however, this percentage is lower than the findings of studies conducted in Enderta district (38%), Holeta (61%), and Goba (47%) [11,16, 24]. The study also revealed that utilization of early PNC was very low (17.5%). This finding is in agreement with that of a study conducted in the rural Jabitena district (20%) [22]. However, it is lower when compared to similar community-based studies conducted in Enderta district [11] and Hossana town [17], where 47% and 51% of women received early PNC, respectively. In general, this discrepancy could be due to the time gap between these studies, variation in study settings, and socio-demographic characteristics of the study area. Moreover, this study was conducted in a rural pastoralist district, where women’s education and decision-making power could be major predictors of maternal healthcare service utilization. The number of healthcare facilities in most rural communities is limited and uneven.
This study revealed that maternal healthcare service utilization is associated with socio- demographic characteristics such as maternal education and age. The odds of ANC utilization were 2.4 times higher in women who had completed primary education and above than in those who had no formal education. Furthermore, mothers aged 15–19 years were 3.7 times more likely to utilize institutional delivery than mothers between 35–49years of age. This finding is consistent with previous studies conducted in Enderta, South Omo, and Tigre regions [11, 12, 19]. Furthermore, mothers who could make decisions alone or jointly with their husbands were more likely to utilize ANC than those whose husbands made decisions alone. This result is consistent with studies conducted in Enderta district and Holeta town [11,16]. A possible explanation for this might be that women’s education is a crucial factor in both economic self- sufficiency and ability to make decisions regarding maternal healthcare services, which in turn improves their knowledge of fundamental healthcare services and promotes health-seeking behaviors. We found that women with planned pregnancies were more likely to utilize ANC and PNC, presumably because they were more concerned about their pregnancy and the child’s welfare than those whose pregnancy was not planned. This finding is consistent with those from studies conducted in Wombera, Debre -Tabor town and Abuna-Gindeberet [13,14,23].
This study also showed that the odds of ANC utilization and delivery in a healthcare facility were higher in mothers who perceived compassionate and respectful care provided by health workers than in those who did not. These results are consistent with those in Kombolcha and Ambo districts [20, 25]. This implies that the attitude of healthcare providers towards women’s healthcare has a major influence on women’s decision to use or not use a particular type of maternal healthcare service. In this study, knowledge of obstetric danger signs was a strong predictor of institutional delivery and PNC use. Mothers who were knowledgeable about at least one obstetric danger sign were more likely to use institutional delivery and PNC services than those who did not spontaneously mention any obstetric danger signs. This finding is in agreement with studies conducted in rural Jabitena district [22]. This can be explained by the fact that awareness of obstetric danger signs is an important factor in motivating women and their families to attend healthcare services at the earliest opportunity, with the intention of prevention, early detection, and management of obstetric danger signs. The current study revealed that mothers who could reach the health facility within one hour were 1.74 times more likely to utilize institutional delivery. This finding is in line with that of a study by Enderta and Butajira [11,21]. Women in labor have less time to reach a hospital than those seeking ANC. Moreover, increased distance from health facilities may be associated with a lack of public transportation and transportation costs. Another significant result of the current study revealed that recent ANC utilization increases utilization of PNC, which is similar to the findings in Hossana, Holeta town and Ambo district [16, 17, 25]. This finding implies that ANC is a key entry point for other maternal healthcare services. Women who attend antenatal care services are provided with full information about necessary pregnancy follow-up, as well as the advantages of institutional delivery and early postnatal care. However, none of the mothers who had received antenatal care visits used PNC.
Strengths and limitations of the study
As the data collection method was interviewer-administered, it contributed to the accuracy of the data collected by explaining unclear points to the respondents. Only the quantitative data collection method was used, and qualitative data collection methods were not triangulated. Therefore, researchers interested in this topic are advised to include qualitative methods.
Conclusion
The overall utilization of maternal healthcare services was far below the targeted health sector growth and transformation plans in the study area. The low utilization of maternal healthcare services in the study area indicates that much work remains to be done to improve women’s health. The study also demonstrated that maternal education, decision-making power, perceived compassionate and respectful care, and current planned pregnancy were significantly associated with ANC utilization. Mothers’ age, time to travel to health facilities, knowledge of danger signs, and perceived compassionate and respectful care were associated with institutional delivery, whereas recent antenatal care utilization, planned current pregnancy, and knowledge of danger signs were significantly associated with PNC utilization. Therefore, considering these identified associated factors and providing information and training on these issues to the community could improve and sustain maternal healthcare service utilization.
Declarations
Ethical considerations
Ethical clearance and approval were obtained from the Ethical Committee of Research and Community Service of the Educational Development Center (EDC) of the Negele Health Science College. Permission was obtained from the district health office. Oral informed consent was obtained from all participants. Confidentiality and anonymity were ensured. The participants were informed that their participation was voluntary.
Author contributions
MD conceived and designed the study MD and SM analyzed the data and interpreted the results. MD prepared the manuscript and assisted with analysis. MD and SM critically reviewed the manuscript. Both authors contributed to the data analysis, drafting, and revision of the article, approved the final version to be published, and agreed to be accountable for all aspects of the work. AG project manager, and corresponding author
Conflicting of interests
The authors declare no potential conflicts of interest with respect to the research, authorship, or publication of this article.
Ethical approval and consent to participate
Ethical clearance and approval were obtained from the Ethical Committee of the Research and Community Service of the Educational Development Center (EDC) of the Negele Health Science College. Permission was obtained from the district health office. Oral informed consent was obtained from all participants. Confidentiality and anonymity were ensured. The participants were informed that their participation was voluntary.
Funding
The authors received no financial support for the research, authorship, or publication of this article.
Informed consent
Verbal informed consent was obtained from all subjects before the study, and written informed consent was obtained from legally authorized representatives before the study.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Supplemental material
Supplemental material for this article is available online.
References
- World Health organization (WHO). (2016). Maternal, Child and Adolescent Health Care, WHO, Geneva. Switzerland.
Publisher | Google Scholor - World Health Organization (WHO). (2015). Trends in Maternal Mortality: 1990 to 2015, World Health Organization, Geneva. Switzerland.
Publisher | Google Scholor - WHO. (2009). Monitoring Emergency Obstetric Care: A Handbook, WHO, UNICEF, UNFPA and AMDD: World Health Organization.
Publisher | Google Scholor - world health Organization [WHO]. (2018). Maternal Mortality Factsheet, 2018, Geneva.
Publisher | Google Scholor - Graham WJ, Ahmed S, Stanton C, Abou-Zahr CL, Campbell OMR. (2008). Measuring maternal mortality: An overview of opportunities, and options for developing countries. BMC Medicine, 6(1).
Publisher | Google Scholor - Nair M, Ariana P, Webster P. (2015). Influences The Decision To Undergo Institutional Delivery By Skilled Birth Attendants In Rural Andhra Pradesh,India. Internatinal Electron J Rural Remote Heal, 1-11.
Publisher | Google Scholor - Olayinka A, Joel A, Bukola D. (2012). Factors influencing utilization of antenatal care services among pregnant women in Ife Central Lga. Osun State Nigeria National Hospital Abuja, 3(3):1309-1315.
Publisher | Google Scholor - Fikre and Demissie. (2012). Prevalence of institutional delivery and associated factors in Dodota Woreda, Oromia regional state, Ethiopia. Reproductive Health, 9:33.
Publisher | Google Scholor - Central Statistical Agency (Ethiopia) and ICF International. (2012). Ethiopian Demographic and Health Survey: Addis Ababa. Ethiopia, Calverton, Maryland and USA.
Publisher | Google Scholor - Central Statistical Agency. (Ethipoia). (2019). Ethiopia Mini Demographic and Health Survey 2019. Addis Ababa.
Publisher | Google Scholor - Aregay A. (2014). Factors Associated with Maternal Health Care Services in Enderta District, Tigray, Northern Ethiopia: Am J Nurs Sci. 3(6):117.
Publisher | Google Scholor - Ergano K, Getachew M, Seyum D, Negash K. (2015). Determinants of Community Based Maternal Health Care Service Utilization in South Omo Pastoral Areas Of. J Med Med Sci., 3(2):112-121.
Publisher | Google Scholor - Mulat G, Kassaw T, Aychiluhim M. (2015). Antenatal Care Service Utilization and Its Associated Factors Among Mothers Who Gave Live Birth In The Past One Year In Womberma Woreda. Ethiop J Heal Sci, 1-10.
Publisher | Google Scholor - T. W. Ayalew and A. M. (2017). Nigatu, Focused antenatal care utilization and associated factors in Debre Tabor Town, northwest Ethiopia. BMC Journal, 11(1).
Publisher | Google Scholor - Nair M, Ariana P, Webster P. (2015). Influences The Decision to Undergo Institutional Delivery by Skilled Birth Attendants In Rural Andhra Pradesh, India. International Electron J Rural Remote Heal, 1-11.
Publisher | Google Scholor - Birmeta K, and et al. (2013). Determinants Of Maternal Health Care Utilization in Holeta Town, Central Ethiopia. BMC Health Serv Res., 13(256):1-10.
Publisher | Google Scholor - Dutamo Z, and et al. (2015). Maternal Health Care Use among Married Women in Hossaina. Ethiopia. BMC Health Serv Res., 1-9.
Publisher | Google Scholor - Biza N. (2016). Institutional Delivery Service Utilization among Pastoralists of Dubti District. Sholar J Appl Med Sci., 4:189-195
Publisher | Google Scholor - Gebrehiwot TG, and et al. (2015). The Health Extension Program and Its Association with Change in Utilization of Selected Maternal Health Services in Tigray Region. A Segmented Linear Regression Analysis, 1-15.
Publisher | Google Scholor - D. Z. Ayele, B. Belayihun, K. Teji, and D. (2014). Admassu Ayana, Factors affecting utilization of maternal health Care Services in Kombolcha District, eastern Hararghe zone, Oromia regional state, eastern Ethiopia. International Scholarly Research Notices.
Publisher | Google Scholor - S. D. Hagos, M. Assegid, A. Mekonen, M. A. (2016). Fantahun, and S. Ahmed, Utilization of institutional delivery service at Wukro and Butajera districts in the northern and South-Central Ethiopia. BMC Pregnancy Childbirth, 14:178.
Publisher | Google Scholor - Y. Gebeyehu and D. W. Hailu. (2014). Factors affecting utilization of postnatal care service in Jabitena district, Amhara region, Ethiopia, Science Journal of Public Health, :3169-176.
Publisher | Google Scholor - Birhanu Darega Gela, Nagasa Dida Bedada, Fikru Tafese Jaleta, Shimeles Ololo Sinkie. (2014). Antenatal Care Utilization and Associated Factors from Rural Health Extension Workers in Abuna Gindeberet District, West Shewa, Oromiya Region, Ethiopia. American Journal of Health Research, 2(4):113-117.
Publisher | Google Scholor - Daniel Bogale Odo, Desalegn Markos Shifti. (2014). Institutional Delivery Service Utilization and Associated Factors among Child Bearing Age Women in Goba Woreda, Ethiopia. Journal of Gynecology and Obstetrics, 2(4):63-70.
Publisher | Google Scholor - Mulugeta Mengistu and et al. (2018). Maternal Health Service Utilization and Associated Factors among Mothers with Children under one Year in Ambo District, West Shoa Zone. Central Ethiopia.
Publisher | Google Scholor - S. Weldemariam, A. Kiros, and M. Welday. (2018). Utilization of institutional delivery service and associated factors among mothers in North West Ethiopian. BMC Research Notes, 11:194.
Publisher | Google Scholor