Case Report
Massive Spontaneous Fetomaternal Hemorrhage: A Case Report
- Mallmann K
- Arlindo EM
- Sá CPN
- Barth MB
- Santos RB
- Reveilleau SM
- Cunha Filho EV *
Gynecology and Obstetrics Service - Moinhos de Vento Hospital - Porto Alegre, Brazil.
*Corresponding Author: Cunha Filho EV, Gynecology and Obstetrics Service - Moinhos de Vento Hospital - Porto Alegre, Brazil.
Citation: Mallmann K, Arlindo EM, Sá CPN, Barth MB, Cunha Filho EV, et al. (2023). Massive Spontaneous Fetomaternal Hemorrhage: A Case Report, Journal of Women Health Care and Gynecology, BioRes Scientia publishers. 2(3):1-4, DOI: 10.59657/2993-0871.brs.23.016
Copyright: © 2023 Cunha Filho EV, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: September 11, 2023 | Accepted: September 16, 2023 | Published: October 07, 2023
Abstract
Spontaneous fetomaternal hemorrhage (FMH) is defined as fetomaternal bleeding with no history of trauma and no clinical or histopathological evidence of placental abruption. Due to its rarity and lethality, we present a case of massive spontaneous fetal maternal hemorrhage in which the diagnosis was suspected after the report of reduced fetal movement, abnormal cardiotocography tracing and increased peak systolic velocity in the middle cerebral artery. This article will review current literature and the obstetric management of pregnancies complicated by FMH.
Keywords: fetomaternal transfusion syndrome; fetomaternal hemorrhage; fetal anemia
Introduction
Fetomaternal hemorrhage (FMH) or fetomaternal transfusion syndrome is the leakage of fetal red blood cells into the maternal circulation. It is a rare phenomenon that occurs during pregnancy, in which there is an exchange of blood between the fetus and the mother through the placenta. It may be responsible for 3.4% of unexplained stillbirths and 0.04% of neonatal deaths [1]. The incidence of spontaneous massive fetomaternal hemorrhage (FMH) is not totally known and its clinical manifestation is unpredictable with nonspecific signs and symptoms. The vast majority of spontaneous FMH are small volume bleeds of no hemodynamic significance, but they may lead to alloimmunization. If FMH is acute and massive, it can result in rapid fetal hemodynamic collapse and death [2].
Case Report
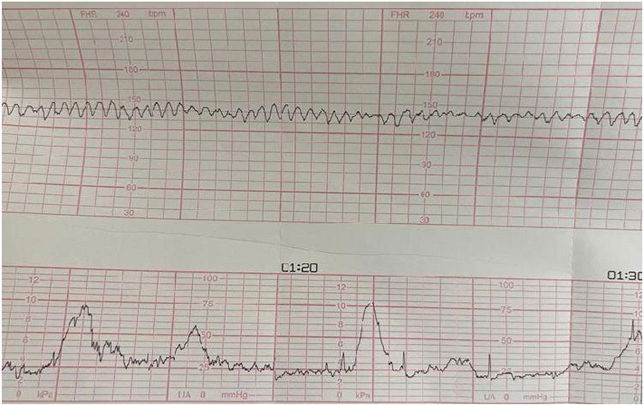
A 42-year-old woman, gravida 4 para 1 abortus 2, blood type O positive, 34 weeks and 6 days of gestational age presented at our hospital with a decrease in fetal movements. Previous history of hypothyroidism (Hashimoto’s disease) controlled with levothyroxine 100mcg. Due to the risk of pre-eclampsia, she made use of acetylsalicylic acid 100mg and calcium 1000mg daily. The patient was investigated for antiphospholipid syndrome due to the history of two miscarriages, but presented normal exams. She had a normal non-invasive prenatal testing (NIPT) early in prenatal care. Besides, she also had a normal first and second trimester morphological ultrasounds and a normal fetal echocardiogram. The fetal was growing at 50th percentile in the last ultrasound performed at 32 weeks. Prenatal care was being uneventful. The patient went to the obstetric emergency because she felt a decrease in fetal movements. Cardiotocography showed sinusoidal heart rate pattern - category 3 (figure 1), and Doppler Ultrasonography showed a middle cerebral artery peak systolic velocity of 91 cm/s (1.79 MoMs), suggesting moderate to severe fetal anemia.
Figure 1: Cardiotocography - sinusoidal heart rate pattern
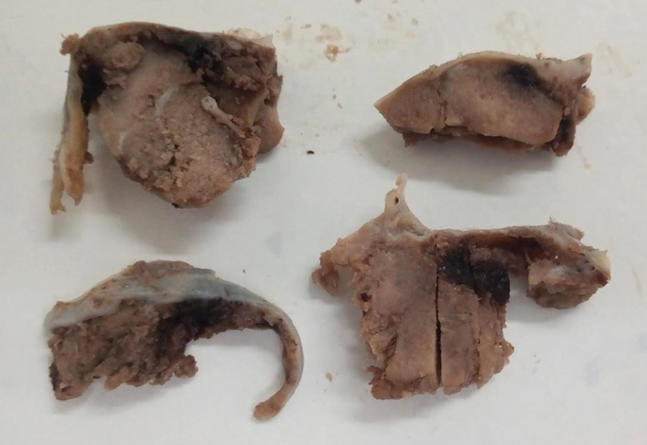
Emergency cesarean section was indicated immediately due to a non-reassuring fetal situation. Birth of a male newborn, weighing 2.460 grams (50th percentile), APGAR 5/7, showing pallor and cold extremities, slow perfusion, and hemoglobin of 1.7 g/dL. The newborn was referred to the neonatal intensive care and proceeded with transfusion of blood products, progressing to death after 24 hours. The placenta was sent for anatomopathological study and showed pallor at macroscopy (figure 2). The microscopic showed countless intervillous hematomas with normoblasts, fetal stromovascular injury, villous edema associated with increased normoblasts and delayed maturation of villi, in addition to villous infarcts and a 4.6 fetoplacental ratio. These findings confirmed the hypothesis of fetal-maternal hemorrhage.
Figure 2: Macroscopy of the placenta - pallor
Discussion
Spontaneous FMH is defined as fetal maternal bleeding with no history of trauma and no clinical or histopathological evidence of abruption. The bidirectional passage of minimal amounts of red blood cells across the placenta is a normal physiological event.2 The pathogenesis of spontaneous massive FMH is unclear. The vast majority of spontaneous FMH are small volume bleeding without hemodynamic significance, but they can lead to alloimmunization [3]. The frequency and volume of these types of bleeding increase with advancing gestational age and are greater at birth [2,3]. Spontaneous massive FMH is much less common. If the FMH is acute and massive, it can result in rapid fetal hemodynamic collapse and death. If the FMH is not massive but chronic, fetal anemia and hydrops fetal may result over time, depending on the ability of the fetus to increase red blood cells production and compensate for ongoing blood loss [3]. Due to the rarity of acute FMH and because we have put together a rich documentation of the fetal and placenta evaluation, we decided to report this case. As FMH is a condition with serious adverse outcomes, therefore a high index of suspicion with prompt investigation and appropriate management may improve the perinatal outcomes after a massive fetal maternal transplacental hemorrhage.
This definition is limited because it does not consider the rate of blood loss or the chronicity of bleeding, which are additional but not measurable factors that affect the fetal outcomes [2]. In the case described above, where blood loss was not measured, the severity criterion was evidenced by doppler ultrasonography with an alterated middle cerebral artery peak systolic velocity, associated with severe fetal anemia [2-5].
The diagnosis can be made by detecting fetal cells in the maternal circulation, using the Kleihauer-Betke (KB) test. The treatment of FMH depends on the severity of the hemorrhage and the gestational age. In severe cases, intrauterine transfusion may be necessary [1,2,6]. The KB test was not performed in our case and the diagnosis was presumed by clinical appearance of sudden onset, cardiotocography with a sinusoidal pattern and doppler ultrasonography with an alternated middle cerebral artery peak systolic velocity. Infectious causes were ruled out. The diagnosis was confirmed by anatomopathological findings in the placenta consistently associated with massive fetomaternal hemorrhage (pallor, intervillous hematomas, and normoblasts). In the third trimester, one of the best parameters of fetal wellbeing is the fetal movement reported by the pregnant woman, which is reduced in cases of hypoxemia, hence its evaluation is extremely important. When abrupt changes in the pattern of movement are reported, they may reveal fetal compromise [7,8]. Maternal perception of decreased fetal movement has traditionally been considered a marker for pregnancies with increased risk of stillbirth and other adverse outcomes [9]. Randomized trials have not compared specific approaches to assessment and management of patients complaining of decreased fetal movement, like physical examination, cardiotocography, stress testing, ultrasonography (fetal biophysical profile), doppler velocimetry, screening for fetal maternal hemorrhage (Kleihauer-Betke test), and amnioscopy [9].
Fetal outcome depends on the rate and volume of bleeding in relation to the total volume of fetoplacental blood [2,10]. Fetal death may be the presenting sign of massive acute bleeding [10]. Hydrops, abnormal fetal heart rate patterns, and decreased fetal movements may be the presenting signs of a massive but non-lethal acute FMH [2-5,11]. Decreased fetal movement is the most common prenatal presentation of this condition, seen in approximately ¼ of all cases [2]. In most cases, the diagnosis of massive FMH is unexpected and immediate intervention is required to avoid unfavorable outcomes [2,11]. In cases of severe fetal anemia, gestational age is extremely important. In pregnancies around 32-34 weeks or more, immediate delivery is indicated, with blood available for neonatal transfusion. The morbidity of preterm delivery at this gestational age is likely to be less than the risk of in utero transfusion or recurrent FMH during expectant management. In pregnancies less than 32 weeks, fetal transfusion by cordocentesis can be performed to correct fetal anemia, as transfusion is probably associated with lower morbidity and mortality than birth [2,11].
In our case report, the definitive diagnosis was made by anatomopathological study of the placenta, which showed pallor, intervillous hematomas and normoblasts, findings that are consistently associated with massive fetal maternal hemorrhage.
Conclusion
Fetomaternal hemorrhage can be a serious complication with severe consequences for neonate. This case report highlights the importance of physician’s awareness on detecting this life-threatening entity. The accurate diagnostic suspicion and prompt intervention may be determining factors for the resolutive success of the case.
References
- Krywko DM, Yarrarapu SNS, Shunkwiler SM. (2022 ). Kleihauer Betke Test.
Publisher | Google Scholor - Kenneth J Moise Jr. (2022). Spontaneous massive fetomaternal hemorrhage.
Publisher | Google Scholor - Bowman JM, Pollock JM, Penston LE. (1986). Fetomaternal transplacental hemorrhage during pregnancy and after delivery. Vox Sang, 51(2):117-121.
Publisher | Google Scholor - de Almeida V, Bowman JM. (1994). Massive fetomaternal hemorrhage: Manitoba experience. Obstet Gynecol, 83(3):323-328.
Publisher | Google Scholor - Bellussi F, Perolo A, Ghi T, Youssef A, Pilu G, Simonazzi G. (2017). Diagnosis of Severe Fetomaternal Hemorrhage with Fetal Cerebral Doppler: Case Series and Systematic Review. Fetal Diagn Ther, 41(1):1-7.
Publisher | Google Scholor - Corrêa RRM, Salge AKM, Ribeiro GA, Ferraz MLF, Reis MA dos, Castro EC da C, et al. (2006). Alterações anatomopatológicas da placenta e variações do índice de Apgar. Rev Bras Saude Mater Infant, 6(2):239-243.
Publisher | Google Scholor - Hubinont C. (2016). Is fetomaternal haemorrhage still a major obstetric complication despite new technologies management? BJOG, 123(12):1907.
Publisher | Google Scholor - Cozzolino M, Magro Malosso ER, Perelli F, Franchi C, Coccia ME. (2017). Keep in mind foetomaternal haemorrage in case of reduced foetal movements: a successful obstetric management. J Obstet Gynaecol, 37(1):100-102.
Publisher | Google Scholor - Ruth C Fretts. (2023). Decreased fetal movement: diagnosis, evaluation and management.
Publisher | Google Scholor - Sifakis S, Koukoura O, Konstantinidou AE, Kikidi K, Prezerakou M, Kaminopetros P. (2010). Sonographic findings in severe fetomaternal transfusion. Arch Gynecol Obstet, 281(2):241-245.
Publisher | Google Scholor - Maier JT, Schalinski E, Schneider W, Gottschalk U, Hellmeyer L. (2015). Fetomaternal hemorrhage (FMH), an update: review of literature and an illustrative case. Arch Gynecol Obstet, 292(3):595-602.
Publisher | Google Scholor