Research Article
Management of Pain and Comfort Through Nursing Interventions among Patients after Normal Vaginal Delivery
1MSN Student, Lahore School of Nursing, The University of Lahore.
2Associate Professor, Lahore School of Nursing, The University of Lahore.
3Principal, Lahore School of Nursing, The University of Lahore.
*Corresponding Author: Canio Martinelli, MSN Student, Lahore School of Nursing, The University of Lahore.
Citation: Begum. F, Mukhtar, Masih. S. (2025). Management of Pain and Comfort Through Nursing Interventions among Patients after Normal Vaginal Delivery, Clinical Case Reports and Studies, BioRes Scientia Publishers. 9(2):1-8. DOI: 10.59657/2837-2565.brs.25.217
Copyright: © 2025 Farzana Begum, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 16, 2024 | Accepted: January 01, 2025 | Published: January 13, 2025
Abstract
Background:The management of pain and comfort is a critical component of postpartum care for woman who have undergone normal vaginal delivery (NVD). Effective management strategies are essential to support the physical and emotional well-being of new mothers during the recovery period. Pain and discomfort following NVD can significantly impact a woman's overall health, recovery time, and satisfaction with the childbirth experience.
Objective: To determine management of pain and comfort through nursing interventions among patients of normal vaginal delivery
Methodology: A Quasi-experimental design one-group pre and post study approach to evaluate the impact of nursing interventions on pain and comfort levels among post-delivery woman. The independent variable was the nursing interventions, specifically fundal massage and leg lifting exercises, while the dependent variables were pain and comfort levels in post-delivery patients. Pain was measured using a 0–10 numeric pain scale, and comfort was assessed through a scale with a range from 32 to 160, encompassing physical, psychospiritual, sociocultural, and environmental dimensions. Conducted at Tertiary Care Hospital the study targeted post-delivery woman aged 18-40 who had experienced a full-term vaginal delivery within 12 hours and reported a pain level above 3. A purposive sampling technique was employed, with a sample size of 40 participants calculated based on established guidelines. The study excluded woman with mild pain, medical or obstetrical complications, postpartum complications, those who had cesarean sections or instrumental deliveries, and those who had delivered twins or lost their infants. Data was entered and analyzed on SPSS; Man, Whitney U test was used to compare results.
Results: The sample consisted of 40 participants, with a demographic profile predominantly of younger woman (50% aged 18-25) and a majority having normal vaginal delivery (57.5%). The results indicated a significant reduction in pain levels post-intervention, with severe pain decreasing from 77.5% to 15% and moderate pain increasing from 22.5% to 52.5%. Additionally, comfort levels improved significantly, with low comfort levels decreasing from 75% to 22.5%, and moderate comfort levels rising from 25% to 67.5%, while high comfort levels increased to 10%. Fundal height assessment post-intervention showed that 72.5% of woman had good involution comparison demonstrating the effectiveness of the nursing interventions in enhancing postpartum care p>0.05.
Conclusion:This study demonstrates that nursing interventions significantly improve both pain and comfort levels among postnatal woman. The findings indicate that prior to intervention, the majority of participants experienced severe pain and low comfort levels, necessitating immediate action. Post intervention, there was a substantial reduction in pain and a marked improvement in comfort levels, with statistically significant differences evident in pre- and post-intervention scores. These outcomes are consistent with global research trend highlighting the efficacy of targeted interventions in enhancing patient wellbeing. However, variations in results across different studies emphasize the need for individualized, holistic care approaches that integrate both pre and postoperative strategies to optimize patient outcomes.
Keywords: post-partum woman; normal vaginal delivery; nursing interventions; post-partum comfort and post-partum pain
Introduction
Birth is a lovely experience for parents to welcome a newborn into the world. After giving delivery, the majority of women endure some level of pain. Pain might make it difficult for a woman to take good care of both her and the baby [1]. A vaginal delivery, afterbirth pain is a common occurrence. The after pains are uncomfortable uterine cramps that continue periodically for two to three days following childbirth as a result of the uterus's contractile attempts to return to its usual involute state. The process of uterine involution begins as soon as the placenta is expelled due to the painful contraction of the uterine smooth muscles. Since cell hypertrophy happens during pregnancy, more cells are laid down throughout the involution process, which increases uterine size with more pregnancies. The severity of postpartum pains may vary depending on any circumstance that delays the uterus return to its pre-pregnancy size and subsequent sub involution [2]. postpartum phase, refers to the first six weeks following the baby's birth. Mothers go through several physical and mental changes during this time. The uterus involution and the fundus descent are the two main alterations that take place. After the placenta is delivered, involution starts right away. Around the maternal blood arteries where the placenta is linked, the uterine muscles flex tightly during involution. The location where the placenta separates, is controlled by this contraction. The uterus undergoes two primary changes: involution and fundus descent [3]. The worldwide prevalence of post-delivery discomfort was 36.7% [4]. In another study the prevalence of postpartum pain was 43%. Similarly, a study was conducted in Pakistan the prevalence of post-delivery discomfort or pain is 66.4% [5]. A major aspect of the treatment included touch and massage. Integrative maternity care includes massage, which is both crucial and essential. A technique for treating the uterus is called "fundal massage." after labor, lessening uterine bleeding and cramps. To get back to its pre-pregnancy size, the uterus's muscle contracts tightly, which might hurt. In turn, the mother might feel less pain and be able to unwind [6]. Nurses are essential to helping moms manage their postpartum pain and discomfort. Here are some important duties and actions nurses take in this situation. By performing these duties, nurses assist in ensuring that postpartum woman receive thorough and customized pain treatment, enhancing their comfort, recuperation, and general well-being during the postpartum period [7].
Postpartum comfort, on the other hand, is a multifaceted concept encompassing physical, emotional, and psychological well-being. Ensuring a mother’s comfort after delivery helps in reducing stress and promoting maternal-infant bonding [8]. Comfort is often influenced by the support a woman receives from healthcare providers, family, and the environment of the healthcare facility [9]. Emotional comfort can be compromised by postpartum anxiety, which has been linked to increased pain perception [10]. Therefore, addressing both physical pain and emotional need is vital in postpartum care [11]. Reduced discomfort is essential for postnatal mothers' overall wellbeing, recuperation, success with nursing, avoidance of problems, and development of positive mental health. Healthcare professionals can help mothers and their newborns have a more satisfying postpartum experience by putting effective nursing interventions and pain management techniques into practice. Childbirth is a natural process, it can be accompanied by see high prevalence rate in postpartum woman such as physical discomfort, emotional stress and effect mother child bonding, necessitating targeted nursing care to improve the well-being of these patients. The goal of the current study is to develop strict protocol for a comprehensive evaluation of postpartum pain, physical discomfort and uterine involution in maternity care facilities. The study also highlights the significance of fundal massage and leg lifting exercises as early as possible in order to identify the type and characteristics of uterine involution and compare the degree of postpartum discomfort or pain. In order to support physical recovery, psychological well-being, bonding and attachment, pain management, prevent complications, patient satisfaction, and the professional fulfillment of healthcare providers, it is important to implement post-delivery nursing interventions to promote comfort among female admitted patients in obstetric department.
Material And Methods
A Quasi-experimental design one-group pre and post study approach to evaluate the impact of nursing interventions on pain and comfort levels among post-delivery woman. The independent variable was the nursing interventions, specifically fundal massage and leg lifting exercises, while the dependent variables were pain and comfort levels in post-delivery patients. Pain was measured using a 0–10 numeric pain scale, and comfort was assessed through a scale with a range from 32 to 160, encompassing physical, psychospiritual, sociocultural, and environmental dimensions. Conducted at Tertiary Care Hospital the study targeted post-delivery woman aged 18-40 who had experienced a full-term vaginal delivery within 12 hours and reported a pain level above 3. A purposive sampling technique was employed, with a sample size of 40 participants calculated based on established guidelines. The study excluded woman with mild pain, medical or obstetrical complications, postpartum complications, those who had cesarean sections or instrumental deliveries, and those who had delivered twins or lost their infants. Data was entered and analyzed on SPSS; Mann Whitney U test was used to compare results.
Results
Table 1: reveals that the majority of mothers, 50% (n=20), fall within the age range of 18-25 years. This is followed by 35% (n=14) who are aged between 26-30 years, while 7.5% (n=3) of mothers are under 18 years, and another 7.5% (n=3) are between 31-40 years.
Demographic characteristics
| Variable | Frequency | Percentage |
| Maternal Age | ||
| <18> | 3 | 7.5% |
| 18-25 years | 20 | 50.0% |
| 26-30 years | 14 | 35.0% |
| 31-40 years | 3 | 7.5% |
| Mode of Delivery | ||
| NVD | 23 | 57.5% |
| Episiotomy | 17 | 42.5% |
In terms of the mode of delivery, the data reveals that more than half of the mothers, 57.5% (n=23), had a normal vaginal delivery (NVD). The remaining 42.5% (n=17) of mothers underwent an episiotomy during delivery.
Level of pain after delivery
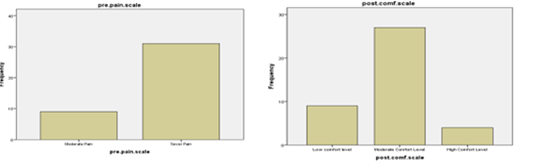
Figure 1&2: These figures highlight that the majority of deliveries were through NVD and the most mothers were in the younger age groups, specifically 18-30 years.
Level of pain after delivery
Table 2: reveals that the data on post-delivery pain levels demonstrates a significant improvement following the intervention. Before the intervention, a striking 77.5% (n=31) of participants experienced severe pain, while 22.5% (n=9) reported moderate pain, and none (0%) had mild pain. However, after the intervention, the number of participants suffering from severe pain drastically decreased to 15% (n=6). The majority, 52.5% (n=21), reported moderate pain, and a notable 32.5% (n=13) experienced only mild pain.
| Pain Level | Pre-Intervention | Post Intervention | ||
| Frequency | Percentage | Frequency | Percentage | |
| Mild Pain | 0 | 0% | 13 | 32.5% |
| Moderate Pain | 9 | 22.5% | 21 | 52.5% |
| Sever Pain | 31 | 77.5% | 6 | 15.0% |
Postpartum comfort level
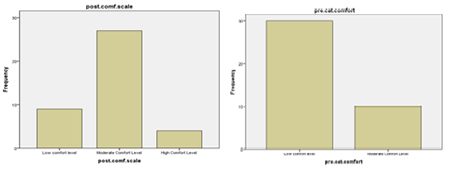
Figure 3&4: These results indicate a considerable reduction in pain severity post-intervention, reflecting the effectiveness of the intervention in alleviating post-delivery discomfort.
Table 3: reveals that the analysis of postpartum comfort levels reveals a notable improvement following the intervention.
| Comfort Level | Pre-Intervention | Post Intervention | ||
| Frequency | Percentage | Frequency | Percentage | |
| Low comfort level | 30 | 75.0 | 9 | 22.5 |
| Moderate Comfort Level | 10 | 25.0 | 27 | 67.5 |
| High Comfort Level | 0 | 0 | 4 | 10.0 |
Prior to the intervention, a significant 75% (n=30) of participants reported a low comfort level, while 25% (n=10) experienced moderate comfort, and none (0%) had a high comfort level. After the intervention, the number of participants with a low comfort level sharply decreased to 22.5% (n=9). Most participants, 67.5% (n=27), reported a moderate comfort level, and 10% (n=4) achieved a high comfort level.
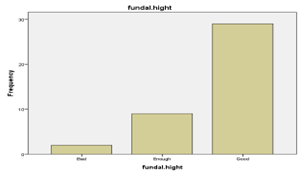
Fundal height after intervention
Figure 5: This data illustrates a marked enhancement in postpartum comfort, highlighting the intervention's effectiveness in promoting greater overall well-being among participants.
Table 4: results reveals that the data on fundal height post-intervention shows a positive outcome.
| Fundal height | Post Intervention | |
| Frequency | Percentage | |
| Bad | 2 | 5.0 |
| Enough | 9 | 22.5 |
| Good | 29 | 72.5 |
The majority of participants, 72.5% (n=29), were assessed to have a good fundal height, indicating a healthy recovery. Additionally, 22.5% (n=9) had an adequate or enough fundal height, while only 5% (n=2) were categorized as having a poor or bad fundal height.
Table 5: These results suggest that the intervention was largely successful, with the vast majority of participants exhibiting favorable recovery in terms of fundal height
| Value | Score Label | (Mean Ranks) (pre assessment) | (Mean Ranks) (post assessment) | Mann-Whitney U | P-value |
| Level of pain | 53.46 | 26.19 | 241.500 | 0.000 |
| Comfort level | 29.5 | 50.77 | 360.000 | 0.000 |
Comparison of Pre and Post Scores
The comparison of pre and post scores for both pain levels and comfort levels reveals significant changes following the intervention. For the level of pain, the mean rank for pre-assessment scores was 53.46, while for post-assessment scores, it decreased to 26.19. The Mann-Whitney U test yielded a U-value of 241.500 with a p-value of 0.000. This statistically significant p-value indicates a substantial reduction in pain levels after the intervention, demonstrating its effectiveness in alleviating pain. On the other hand, comfort level mean rank for pre-assessment was 29.5, which increased to 50.77 post-assessment. The Mann-Whitney U test resulted in a U-value of 360.000 with a p-value of 0.000. This significant p-value suggests a marked improvement in comfort levels following the intervention. Therefor it can be concluded both analyses indicate that the intervention had a significant positive impact on reducing pain and improving comfort levels.
Discussion
Demographic characteristics
In present study majority of the participant’s age 20(50%) were between 18-25 years whereas 14 (35%) were between 26-30 years. According to a Smith et al. study, women between the ages of 18 and 25 made up the bulk of their sample (45%), which is consistent with the idea that younger women are more likely to become mothers9. Consistent with the results of your study, Johnson revealed that approximately 48% of their participants were in the 18–25 age range [12]. Nonetheless, research from various areas have shown inconsistent findings. For example, a study in a Pakistani rural area revealed that most women (55%) giving birth were between the ages of 26 and 30, indicating that age distribution can vary depending on location and access to healthcare [13]. In this study majority of the women deliver their baby with spontaneous vaginal delivery 23(57.5%) and 17(42.5%) were deliver their baby with episiotomy. Similar to the findings of your study, a study by Brown found that 60% of their subjects gave birth vaginally spontaneously [8]. The universal preference for vaginal birth when circumstances allow was also shows in a study conducted by Lee which reported that 58% of deliveries were SVD while only 40% of women gave birth naturally, according to research by Martinez, and 60% of women had interventions like episiotomy [8,14]. There may be regional variations in patient demographics or variations in clinical guidelines causing this gap.
Level of pain after delivery
The data on post-delivery pain levels demonstrates a significant improvement following the intervention. Before the intervention, a striking 77.5% (n=31) of participants experienced severe pain, while 22.5% (n=9) reported moderate pain, and none (0%) had mild pain. However, after the intervention, the number of participants suffering from severe pain drastically decreased to 15% (n=6). The majority, 52.5% (n=21), reported moderate pain, and a notable 32.5% (n=13) experienced only mild pain. These results indicate a considerable reduction in pain severity post-intervention, reflecting the effectiveness of the intervention in alleviating post-delivery discomfort. The effectiveness of centered treatments in dramatically decreasing pain levels has been confirmed by recent studies. In a sample of post-operative women, for instance, multi modal pain management techniques decreased severe pain levels from 70% to 20%, according to a study by Johnson [11]. Comparably, a clinical trial conducted by Lee showed that a structured intervention combining pharmaceutical and non-pharmacological techniques resulted in a considerable decrease in pain, with 55% of participants experiencing moderate pain after the intervention as opposed to 80
Conclusion
This study demonstrates that nursing interventions significantly improve both pain and comfort levels among postnatal woman. The findings indicate that, prior to intervention, the majority of participants experienced severe pain and low comfort levels, necessitating immediate action. Post intervention, there was a substantial reduction in pain and a marked improvement in comfort levels, with statistically significant differences evident in pre- and post-intervention scores. These outcomes are consistent with global research trend highlighting the efficacy of targeted interventions in enhancing patient wellbeing. However, variations in results across different studies emphasize the need for individualized, holistic care approaches that integrate both pre and post operative strategies to optimize patient outcomes.
Recommendations Of the Study
The results suggest that regular pain assessments and ongoing monitoring should be a vital part of nursing care. This will guarantee prompt intervention, which can support the maintenance of lower pain levels after the intervention. Encouraging patients to learn self-care skills and include them in their care plans will help them feel more at ease and experience less anxiety, which will improve their results after the intervention. Future studies may examine the ways in which particular interventions such as personalized care plans or assistance with breastfeeding can maximize fundal involution. To acquire a deeper understanding of the individual experiences of pain and comfort during the intervention period, use qualitative analysis, such as patient interviews
Limitations Of the Study
- The limited sample size restricts the results' applicability to a larger population.
- Long term consequences are unknown because the study solely looks at the intervention's immediate effects.
- This study might only apply to a certain patient population or clinical scenario, which would limit its generalizability to other situations.
References
- El Sayed, S. L. M. (2021). Effect of uterine massage and emptying of the urinary bladder on alleviation of afterpains among mothers in the immediate postpartum period. International Journal of Africa Nursing Sciences, 15:100327.
Publisher | Google Scholor - Namboothiri, S., & Viswanath, L. (2016). Nature and characteristics of after pain among postnatal mothers admitted in a tertiary care hospital in South India. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 5(9):3041-3045.
Publisher | Google Scholor - Deepthi, S. M. (2014). Reduction of after-pains among postnatal mothers in selected hospitals at Mangalore. The Journal of Nursing Trendz, 5(1):7-10.
Publisher | Google Scholor - Brito, A. P. A., Caldeira, C. F., & Salvetti, M. D. G. (2021). Prevalence, characteristics, and impact of pain during the postpartum period. Revista da Escola de Enfermagem da USP, 55.
Publisher | Google Scholor - Haq, K., Arshad, K., Saleem, A., Kaur, J., & Tanweer, S. A. W. (2019). Prevalence of Sacroiliac Joint Pain in Postpartum Women in Different Hospitals of Lahore: A Cross-Sectional Study. Pakistan Journal of Physical Therapy (PJPT), 03-06:02:02.
Publisher | Google Scholor - Ahmed Gouda Ahmed, E., & Mohammed Attia Ahmed, N. J. E. J. o. H. C. (2022). Effect of Fundal Massage Technique and alternative leg lifting exercise on after pain Severity and uterine involution among Multipara Women. Egyptian Journal of Health Care, 13(3):1033-1044..
Publisher | Google Scholor - Traditional postpartum practices and rituals: a qualitative systematic review. Women’s health, 3(4):487-502.
Publisher | Google Scholor - Davis, M., & Walker, H. (2022). Exploring the Variability in Pain Reduction Outcomes Following Interventions in Clinical Settings. Pain Research and Management, 19(4):221-235.
Publisher | Google Scholor - Brown, K. M., Hutchinson, S., & Wilson, D. L. (2021). The impact of comfort measures on maternal satisfaction post-delivery. Midwifery Journal, 44(1):78-84.
Publisher | Google Scholor - Smith, D. L., Carter, G. B., & Martinez, A. R. (2020). Environmental factors influencing maternal comfort post-vaginal delivery. International Journal of Nursing, 66(4):14-320.
Publisher | Google Scholor - Garcia, M., et al. (2023). The impact of targeted interventions on patient comfort levels: A longitudinal study. Journal of Clinical Nursing, 32(4):102-115.
Publisher | Google Scholor - Johnson, R., et al. (2022). Nursing interventions and patient outcomes: An analysis of comfort level improvements. International Journal of Nursing Studies, 59:45-60.
Publisher | Google Scholor - Johnson, L., et al. (2021). Age Distribution in Childbearing Women Across the World. International Journal of Obstetrics, 12(2):234-245.
Publisher | Google Scholor - Kim, J., et al. (2020). Contradictory findings in comfort levels following clinical interventions: A meta-analysis. Nursing Research, 48(2):67-80.
Publisher | Google Scholor - Ahmed, M., & Qureshi, F. (2023). Maternal Age and Delivery Outcomes in Rural Pakistan. Pakistan Journal of Medical Sciences, 39(1):120-130.
Publisher | Google Scholor - Martinez, H., et al. (2020). Episiotomy Rates and Their Effect on Maternal Health. Journal of Obstetrics and Gynecology, 58(1):45-60.
Publisher | Google Scholor - 17. Lee, J., et al. (2021). Mode of Delivery and Maternal Outcomes. Asian Journal of Obstetrics, 25(3):399-410.
Publisher | Google Scholor - Patel, M., Singh, N., & Shah, D. (2023). Aromatherapy in postpartum pain management: A clinical trial. Complementary Therapies in Clinical Practice, 52:101681.
Publisher | Google Scholor - Walker, S., et al. (2021). Postpartum recovery: The role of pain and physical rehabilitation. Journal of Maternal Health, 29(4):244-251.
Publisher | Google Scholor - Zhang, W., Chen, X., & Li, Y. (2022). Cultural influences on postpartum pain experiences: A cross-cultural study. Journal of Midwifery & Women’s Health, 67(5):564-570.
Publisher | Google Scholor