Case Report
Management of Aberrant Frenae-A Case Series
Assistant Professor, Department of Periodontology, Government Dental College and Hospital, Mumbai, India.
*Corresponding Author: Gulnar Sethna,Assistant Professor, Department of Periodontology, Government Dental College and Hospital, Mumbai, India.
Citation: Sethna G. (2024). Management Of Aberrant Frenae-A Case Series. Dentistry and Oral Health Care, Biores Scientia Publishers. 3(3):1-5. DOI: 10.59657/2993-0863.brs.24.035
Copyright: © 2024 Gulnar Sethna, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 10, 2024 | Accepted: May 25, 2024 | Published: June 22, 2024
Abstract
The frenum of the oral vestibule is a fold of mucous membrane that includes muscle and connective tissue fibbers, connecting the lip and cheek to the alveolar mucosa, gingiva, and periosteum. Aberrant labial and buccal frenula can negatively impact facial aesthetics by affecting the interdental papilla, leading to issues such as a median diastema, gingival recession, reduced vestibular depth, restricted lip movement, and compromised oral hygiene. This article provides an overview of the labial and lingual frenum and explores various treatment modalities for managing an aberrant frenum. These treatments include several frenectomy techniques such as Miller's technique, Z-Pasty, and lingual frenectomy using both cold blade instruments and thermal sources like electrocautery and diode laser.
Keywords: frenum; frenectomy; diode laser; electrocautery; ankyloglossia
Introduction
A frenum is often described as a triangular fold of mucous membrane and connective tissue or muscle fibers that attach the lip and cheek to the alveolar mucosa and/or gingiva, as well as the underlying periosteum [1-3]. Histological evaluations of the labial frenum vary: some studies identify the presence of epithelium and muscle fibers, while others report elastic and muscle fibers [4,5]. However, Henry et al. found dense collagenous tissue and elastic fibers, but no muscle fibers in the frenulum. [6] Based on the anatomical attachment site, Placek et al [7].established a clinical and morphological classification of maxillary frenum attachment, categorizing it into four types:
Mucosal: Fibers attached up to the mucogingival junction.
Gingival: Fibers inserted within the attached gingiva.
Papillary: Fibers extending into the interdental papilla.
Papilla penetrating: Fibers crossing the alveolar process and extending up to the palatine papilla.
Papillary and papilla penetrating frenae are often considered pathological and have been associated with loss of papilla, recession, diastema, and plaque accumulation [8,9]. Aberrant labial and buccal frenula can negatively impact facial aesthetics by involving the interdental papilla, leading to issues such as a median diastema, gingival recession, decreased vestibular depth, restricted lip movement, and interference with oral hygiene. [1-3]. The tongue, in conjunction with the lingual frenum, plays a crucial role in speech articulation, phonetics, and tongue movements. The lingual frenum is characterized by a median fold connecting the tongue to the floor of the mouth, comprising fibrous tissue and superior fibers of the genioglossus. Aberrant positioning or increased thickness of the lingual frenum can adversely affect tongue movements and may cause mandibular anterior gingival recession. [10,11].
Treatment
Several techniques are employed for managing an aberrant frenum, including frenectomy and frenotomy. Frenectomy is defined as the complete removal of the frenum, including its attachment to the underlying bone, while frenotomy involves the relocation of the frenal attachment [12]. These procedures can be performed using conventional cold blade instruments as well as thermal sources like electrocautery, diode laser, and radiofrequency ablation.
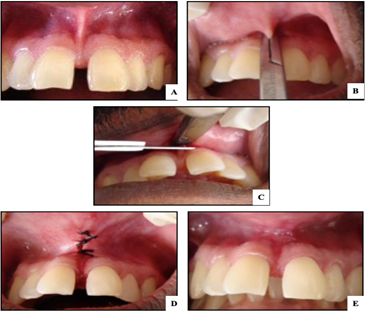
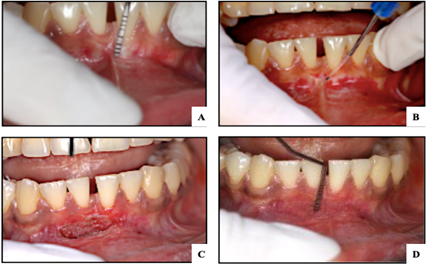
Clinical Cases: Case 1
Classical Frenectomy [2,13]. The classical technique, introduced by Archer (1961) and Kruger (1964), was initially recommended for cases with midline diastema to remove muscle fibers connecting the orbicularis oris with the palatine papilla. In this case, a 30-year-old patient presented with a papillary -penetrating type of frenal attachment. (Figure -1A) On clinical examination, there was a probing pocket depth of 6 mm with grade 1 mobility of the maxillary central incisors. The tension test was positive. After obtaining informed consent, local anaesthesia (2% lignocaine with 1:80,000 adrenaline) was administered. A haemostat was inserted into the vestibule to engage the frenum, (Figure -1B) and two incisions were made flush with the superior and inferior planes of the haemostat until the frenum was disengaged. (Figure -1C) Blunt dissection was performed to relieve any fibrous attachment, and the edges of the diamond-shaped wound were sutured using 4-0 black silk with interrupted sutures. (Figure -1D) The area was covered with a periodontal dressing, which, along with the sutures, was removed one week postoperatively, revealing good healing at the surgical site (Figure -1E).
Figure 1
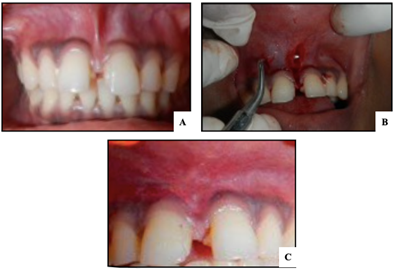
Case 2
Frenectomy Using Lateral Pedicled Flap (Miller’s Technique) [2,14]. A 20-year-old female patient, referred from the Department of Orthodontics, presented with a papillary-penetrating frenum attachment. (Figure 2A) After administering local anaesthesia, a horizontal incision was made to separate the frenum from the base of the interdental papilla. A second vertical parallel incision was made 2 mm apical to the marginal gingiva, extending to the vestibule. (Figure 2B) A partial-thickness flap was raised and displaced laterally towards the midline, then sutured with resorbable 4-0 Vicryl sutures. A periodontal dressing was placed and removed after one week, showing minimal scarring postoperatively (Figure 2C).
Figure 2
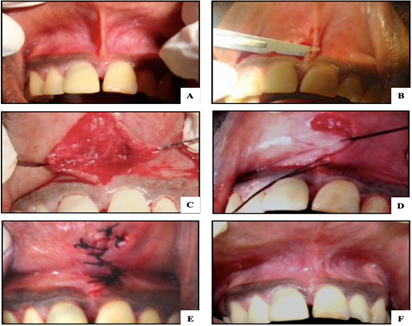
Case 3
Z-Plasty: A 20-year-old male presented with a progressively increasing midline space between the upper central incisors. Examination revealed a thick aberrant labial frenum extending into the interdental papilla and a short vestibule. (Figure 3A) After local anaesthesia administration, a vertical incision was made along the frenum's entire length with a no.15c blade. (Figure 3B) Two horizontal incisions at the ends of the vertical incision, angulated between 60° and 90°, created triangular flaps. (Figure 3C) These flaps were transposed through 90° (Figure 3D) and sutured with black silk (4-0) sutures. (Fig 3E) Healing was uneventful with minimal scarring (Fig 3F).
Figure 3
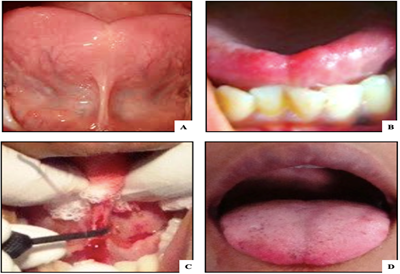
Case 4
Lingual Frenectomy with Electrocautery. A 35-year-old male with Kotlow’s ankyloglossia (Class III) reported difficulty in speech since birth. [16] (Figure 4A) He was unable to protrude his tongue to the lower lip. [Figure 4B] Under local anaesthesia, a lingual frenectomy was performed using electrocautery. A curved haemostat clamped the frenum, and a loop electrode made incisions at the superior and inferior aspects of the haemostat. .[Figure 4C] Muscle fibers were relieved with the haemostat, and minimal bleeding required no sutures. Postoperative tongue movements were significantly improved, and the patient was advised to perform tongue exercises.
Figure 4
Case 5
Laser-Assisted Mandibular Labial Frenectomy. A 22-year-old female presented with a fiber pull from the labial frenulum and a narrow zone of keratinized gingiva. (Figure 5A) To prophylactically reduce the risk of labial recession on the mandibular left central incisor, a diode laser frenectomy was planned. Under local anaesthesia, a 940 nm diode laser (Ezlase TM, Biolase technology, USA) with a 400-micrometer fiber optic tip was used. (Figure 5B) The frenum was excised using sweeping vertical and lateral motions, resulting in a protein coagulum occupying the healing area after one week (Figure 5C) and complete epithelialization after two weeks. A follow-up after six months showed excellent tissue healing and a 5 mm increase in vestibular depth (Figure 5D).
Figure 5
Discussion
While the classical frenectomy technique remains widely used, newer surgical methods such as Miller’s technique, laser surgery, and soft tissue grafts offer significant advantages. The classical technique ensures complete removal of the frenum and associated muscle fibers but may result in unesthetic scarring [14,15,16]. Miller’s technique, proposed for post-orthodontic diastema cases, preserves the transeptal fibers, across the midline without disruption of the fibers which gives a bracing effect and minimizes the chances of relapse after orthodontic treatment [15]. It was concluded that the frenectomy should be performed after the orthodontic movement is complete and about 6 weeks before the appliances are removed. This ensures optimal healing and tissue maturation and permits the clinician to use orthodontic appliances for retaining a periodontal dressing. Z-Plasty, a periodontal plastic surgery, elongates the tissue, redistributes tissue tension and improves scar appearance. [18,19].
Ankyloglossia, or tongue-tie, is a congenital anomaly which is characterized by a short lingual frenulum [20]. The evidence demonstrating that ankyloglossia and abnormal tongue position can influence skeletal development and its association with malocclusions is limited [21]. However, some studies have suggested that a hypertrophic lingual frenum is associated with a high-arched palate and an elongated soft palate [22]. For ankyloglossia, techniques like scalpel surgery, electrosurgery, and laser treatments are available. Electrosurgery minimizes bleeding and postoperative complications but must be used cautiously to avoid burns and other risks. Studies comparing electrosurgery and diode laser techniques have shown varied outcomes, with diode laser associated with more postoperative inflammation and higher relapse rates [23].
Conclusion
Managing aberrant frenae effectively can enhance oral hygiene and prevent periodontal disease progression. Early intervention and appropriate surgical techniques can significantly improve periodontal health and aesthetic outcomes.
References
- Gottsegen R. (1954). Frenum position and vestibule depth in relation to gingival health. Oral Surg Oral Med Oral Pathol. 7(10):1069-1078.
Publisher | Google Scholor - Freedman AL, Stein MD, Schneider DB. (1982). A modified maxillary labial frenectomy. Quintessence Int, 13(6):675-678.
Publisher | Google Scholor - Huang WJ, Creath CJ. (1995). The midline diastema: a review of its etiology and treatment. Pediatr Dent. 17(3):171-179.
Publisher | Google Scholor - The superior labial frenum: a histologic observation. Gartner LP, Schein D. (1991). Quintessence Int. 22:443-445.
Publisher | Google Scholor - Jhaveri Editor. (2006). The Aberrant Frenum. Dr. PD Miller the father of periodontal plastic surgery, 29-34.
Publisher | Google Scholor - Henry SW, Levin MP, Tsaknis PJ. (1976). Histological features of superior labial frenum. J Periodontol 47:25-28.
Publisher | Google Scholor - Placek M, Miroslavs, Mrklas L. (1974). Significance of the labial frenal attachment in the periodontal disease in man. Part1; Classification and epidemiology of the labial frenum attachment. J Periodontol, 45:891-894.
Publisher | Google Scholor - Dewel BF. (1996). The labial frenum, midline diastema, and palatine papilla: A clinical analysis. Dent Clin North Am, 3:175-184.
Publisher | Google Scholor - Díaz-Pizán ME, Lagravère MO, Villena R. (2006). Midline diastema and frenum morphology in the primary dentition. J Dent Child (Chic), 73:11-14.
Publisher | Google Scholor - Miller PD Jr. (1985). The frenectomy combined with a laterally positioned pedicle graft. Functional and esthetic considerations. J Periodontol, 56:102-106.
Publisher | Google Scholor - Komori S, Matsumoto K, Matsuo K, et al. (2017). Clinical study of laser treatment for frenectomy of pediatric patients. Int J Clin Pediatr Dent, 10(3):272-277.
Publisher | Google Scholor - Benias, P.C.; Carr-Locke, D.L. (2019). Principles of Electrosurgery. In ERCP [Internet]; Elsevier: Amsterdam. The Netherlands,86-92.
Publisher | Google Scholor - Archer WH. (1975). Oral surgery for a dental prosthesis. Oral and Maxillofacial surgery. In: Archer WH, editor. Philadelphia: Saunders, 135-210.
Publisher | Google Scholor - Miller PD. (1985). Frenectomy, combined with a laterally positioned pedicle graft-functional and esthetic considerations. J Periodont, 56:102-106.
Publisher | Google Scholor - Archer WH, editor. (1961). Oral Surgery – A Step-by-Step Atlas of Operative Techniques. W. B. Saunders Co, 192.
Publisher | Google Scholor - Brzęcka D, Garbacz M, Micał M, Zych B, Lewandowski B. (2019). Diagnosis, classification and management of ankyloglossia including its influence on breastfeeding. Dev Period Med, 23(1):79-87.
Publisher | Google Scholor - Kruger GO, editor. Oral C.V. Mosby Co. (1961). 46.
Publisher | Google Scholor - Denonvillers M. Blepharoplastie. Bull Soc Chir, 7:1856-1857.
Publisher | Google Scholor - Branski LK. Hundeshagen G, Zapata-Sirvent R, Goverman J.(2017). Tissue Rearrangements: The Power of the Z-Plasty. Clinics in plastic surgery. 2017 of the Z-Plasty. Clinics in plastic surgery, 44(4):805-812.
Publisher | Google Scholor - Chaubal, Tanay V. Dixit M Ankyloglossia and its management, J Indian Soc Periodontol, 15(3): 270-272.
Publisher | Google Scholor - Lalakea, M.; Messner, A.H. (2003). Ankyloglossia: Does it matter? Pediatr. Clin. N. Am. 50: 381-397.
Publisher | Google Scholor - Yoon, A. Zaghi, S. Weitzman, R. Ha, S. Law, C.S. Guilleminault, C. Liu, S.Y. (2017). Toward a functional definition of ankyloglossia: Validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 21:767-775.
Publisher | Google Scholor - Mazzoni A, Navarro RS, Fernandes KPS, Mesquita-Ferrari RA. (2022). Horliana ACRT.Comparison of the Effects of High-Power Diode Laser and Electrocautery for Lingual Frenectomy in Infants: A Blinded Randomized Controlled Clinical Trial. J Clin Med, 11(13):3783.
Publisher | Google Scholor