Research Article
Magnitude of Preterm Premature Membrane Rupture and Associated Factors Among Pregnant Women Admitted to Bishoftu General Hospital in Oromia of Ethiopia, 2023
- Bezawit Tsegaye
- Wogene Morka Regassa *
Department of Midwifery, College of Health Sciences, Arsi University, Asella, Ethiopia.
*Corresponding Author: Wogene Morka Regassa, Department of Midwifery, College of Health Sciences, Arsi University, Asella, Ethiopia.
Citation: Tsegaye B, Regassa W M. (2024). Magnitude of Preterm Premature Membrane Rupture and Associated Factors Among Pregnant Women Admitted to Bishoftu General Hospital in Oromia of Ethiopia, 2023. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(5):1-8. DOI: 10.59657/2993-0871.brs.24.042
Copyright: © 2024 Wogene Morka Regassa, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: April 23, 2024 | Accepted: May 17, 2024 | Published: May 31, 2024
Abstract
Background: During pregnancy, the bag of water surrounding the baby can break prematurely, which can lead to complications for both the mother and the baby. It is important to understand the burden and causes of this problem so that preventable factors can be ended. However, at Bishoftu General Hospital in Ethiopia, data has been limited.
Objective: The study aimed to assess the magnitude and associated factors of preterm premature membrane rupture among pregnant mothers admitted at Bishoftu General Hospital, Ethiopia in 2023.
Method: An institutional-based cross-sectional study included 303 study participants was carried out from February to May 2023. Participants were selected through a systematic sampling technique from the registration book. Structured pretested interview-administered questionnaires were used to collect data. Epi Data version 3.1 was used to enter the data, and SPSS version 25 was used to analyze logistic regression with a p-value of 5% significance level.
Results: The magnitude of preterm premature rupture of the membrane was 20.9% (95% CI: 16.5-26). Previous [PROM (AOR = 0.27, 95% (CI: 0.73–0.59), preterm delivery (AOR = 7.3, 95% (CI: 1.9-27.2), abortion (AOR = 6.98, 95% (CI: 1.4–35.7), and cesarean section (AOR = 5.3 95% (CI: 1.6– 16.6)] were factors associated with preterm premature rupture of membrane.
Conclusion: The magnitude of preterm premature rupture of the membrane was high. To improve identified factors, it is critical to utilize evidence-based interventions aiming to end preventable factors to enhance positive pregnancy outcomes.
Keywords: premature rupture of membrane; preterm labor; prevalence; pregnant women; Ethiopia
Introduction
Sometimes, the amniotic fluid that protects the baby inside the mom's tummy can break before the baby is ready to be born. This can happen before the baby grows for 37 weeks [1]. The water is important because it keeps the baby safe from getting sick, hurt, or having problems with the cord that gives it food and oxygen [2]. If there isn't enough water or if the water breaks too early, it can squeeze the cord and make it harder for the baby to get enough blood. If the membrane that holds water breaks, it can also stop protecting the baby as it should and affect how the baby grows [3].
Preterm premature rupture of membrane (PPROM) is defined as membrane rupture before the onset of labor in pregnancies between 28 and 37 weeks of gestation [4]. It is notable for its painless liquid flow and other investigations such as the ferning and pooling tests. The lowest gestational age that can be described as Preterm labor in Ethiopia is defined as a pregnancy lasting more than 28 weeks and less than 37 weeks [5]. PPROM is frequently associated with a lot of complications, including infections and inflammations that result in maternal and neonatal deaths. Intact fetal membranes act as a barrier against ascending infection. Both the mother and the fetus are at risk of infection and other complications if the membranes rupture [2,6-8]. To date, various guidelines and standards have been put in place to manage obstetric complications that arise during pregnancy, labor, and delivery to reduce maternal and neonatal mortality. The diagnosis of PROM is adequately made by a history suggestive of spontaneous rupture of membranes. This is followed by a sterile speculum examination demonstrating pooling of fluid in the posterior vaginal fornix [9].
Preterm PROM is one of the major factors that have been linked to poor pregnancy outcomes. It is still a critical clinical and public health issue in developing countries [10]. However, research on risk factors of PPROM in developing countries, particularly in the study setting is limited. Besides having had insufficient sample size [11, 12], some previous studies also lacked variables of interest such as lifestyles, accidental falls, lifting heavy objects, and the presence of tuberculosis (TB) supposed to affect pregnant women [11]. Therefore, this study aimed to determine the magnitude and risk factors of PPROM in the study area. Overall, the purpose of the study was to enhance positive pregnancy outcomes.
Methods and Materials
Study setting, period, and design
The study took place from February to March 2023 at Bishoftu General Hospital, located in Bishoftu Town in Oromia Regional State, East Shewa Zone, Ethiopia, and 47 kilometers from Addis Ababa. There are a variety of health services available, including antenatal care, an expanded immunization program, family planning, antiretroviral therapy services, abortion and post-abortion care, delivery services, an outpatient department, a pediatric ward, a medical ward, a surgical ward, a Gynecology ward, a postoperative ward, and a dental clinic. An institutional-based cross-sectional study was employed.
Source and study population
All pregnant mothers admitted to Bishoftu General Hospital were the source population. The study population was all sampled pregnant mothers who were admitted to Bishotu General Hospital during the study period.
Eligibility criteria
All pregnant mothers with gestational age greater than or equal to 28 weeks but less than 37 weeks. A mother who had a serious illness such as preeclampsia, eclampsia, multiple pregnancies, polyhydramnios, and refused to participate were excluded.
Sample size and Sampling technique
The sample size was determined using the single population proportion formula with the following assumptions: [n= (Zα/2) 2 p (1-p)/d 2], where; the given confidence interval 1.96, d=margin of error (0.05), the prevalence of PROM from previous study was 23.5% [13]. Adding a 10% non-response rate, the total sample size required was 303 pregnant women. The total average number of mothers admitted to the hospital in bi-months was 820, as reported by Bishoftu General Hospital. The sampling interval, k, was calculated by dividing the source population by the sample size; K=820/296 =2.8, k ~ 3. Every third of the study participants were selected through systematic random sampling techniques from the logbook.
Data collection tools and procedure
Structured questionnaires were adopted from previous literature [11, 12, 14, 15]. Five Bachelor of Science holders and experienced data collectors conducted the data collection. The contextualized questionnaires were used to collect data on the respondents’ demographics, reproductive health services, history of pregnancies, and current and past medical conditions. Additional information was abstracted from clients' medical records using data extraction tools modified from WHO standard tools. Four independent data collectors were not working at the selected hospital and one supervisor was assigned to the hospital. The data collectors completed each questionnaire, signed it, and had it reviewed by supervisors.
Data processing and analysis
Epi Data version 3.1 was used for data entry and cleaning, and SPSS version 25 was used for analysis. Descriptive analysis was done to determine the magnitude of preterm premature membrane rupture among pregnant women. Bivariate analysis was used to examine the relationship between the dependent and independent variables, and an odds ratio with a 95% confidence interval was analyzed. All variables with a P-value of 0.25 in the bivariate analysis were included in the multivariate logistic regression analysis model to depict factors related to dependent variables. The P-value for statistical significance was set at 5%. The multicollinearity test was assessed to check the correlation between independent variables using variance inflation factor (VIF) and no multicollinearity was detected. The VIF score was less than 5. The model fitness was determined using the Hosmer-Lemeshow goodness-of-fit test (P=0.8).
Data quality control
The accuracy of the data was ascertained while adopting standardized questionnaires, and five data collectors and supervisors received one day of training on the objective, ethics, and tools. The tool was translated into the local language as well as back into English by a language expert to ascertain consistency. The data collection tool was pre-tested before the study period, and necessary corrections were made following the pre-test result to ascertain the quality of the tools. The supervisor monitored the data collection process to ensure the quality of the data. Daily, the supervisors checked the completeness of the collected data. Before data entry, the completeness, accuracy, and consistency of the data were checked. Incomplete questionnaires were excluded from the analysis. The interview was conducted privately. Furthermore, data was entered into Epi Data, exported to SPSS, and checked for outliers.
Study variables
Dependent variable: preterm premature rupture of membrane
Independent variables: Sociodemographic characteristics, Obstetric and reproductive health-related factors.
Operational definitions
Preterm premature rupture of membrane - rupture of membrane before 37 weeks of gestational age. Premature rupture of membrane- rupture of membrane at least for one hour before onset of labor. Preterm labor – onset of labor before 37 weeks of gestational age [15].
Ethical consideration
Arsi University College of Health Science Ethical Review Committee provided ethical clearance with protocol number: A/U/mw-983/15 dated 25/01/2023. The administration of Bishoftu General Hospital granted permission. Permission was also obtained from the head of the obstetrics and gynecology ward. Following an explanation of the study's purpose, duration, potential risks, and benefits, study participants provided verbal informed consent.
Results
Socio-demographic characteristics
Out of 303 study participants, 296 pregnant women participated in the study, yielding a 97.7% response rate. In this study, most of the participants were residents of urban 204(69%). The majority of the participants (93%) were Oromo in ethnicity and 156(53%) respondents were 18-29 years old. The majority 148(50%), of the participants, attended secondary school. Two hundred eighty (94%) of the study participants were married, and more than half of the study subjects, 158 (53%) were housewives, with few earning more than 6000 (6%) average monthly income Ethiopian birr (Table 1).
Table 1: Socio-demographic characteristics of pregnant women admitted at Bishoftu General Hospital Oromia, Ethiopia, 2023.
| Variables | Categories | Frequency | Percent (%) |
| Age (in years) | 18-29 | 156 | 53 |
| 30-39 | 138 | 46 | |
| >40 | 2 | 1 | |
| Residence | Rural | 92 | 31 |
| urban | 204 | 69 | |
| Educational status | No education | 6 | 2 |
| Primary | 92 | 31 | |
| Secondary | 148 | 50 | |
| More than secondary | 60 | 17 | |
| Religion | Protestant | 78 | 26 |
| Orthodox Christian | 172 | 58 | |
| Catholic | 4 | 2 | |
| Muslim | 42 | 14 | |
| Ethnicity | Oromo | 276 | 93 |
| Amhara | 12 | 4 | |
| Other | 8 | 3 | |
| Monthly income | 1000-2000 | 110 | 38 |
| 2000-4000 | 114 | 38 | |
| 4000-6000 | 54 | 18 | |
| >6000 | 18 | 6 | |
| Occupation | Government employee | 54 | 19 |
| Private employee | 32 | 10 | |
| Merchant | 36 | 12 | |
| Housewife | 158 | 53 | |
| Student | 14 | 5 | |
| Other | 2 | 1 | |
| Marital status | Single | 12 | 5 |
| Married | 280 | 94 | |
| Divorced | 2 | 0.5 | |
| Widowed | 2 | 0.5 |
The obstetric and reproductive health characteristics
The majority of the participants (51%) were multigravida, 234 (79%) had gestational age greater than or equal to 37 weeks, and nearly all of the respondents 272 (92%) had ANC follow-up, 54 (18%) had a history of PROM, and 32 (11%) had a history of preterm delivery (Table 2).
Table 2: Obstetric and RH characteristics of the pregnant women admitted at Bishoftu General Hospital Oromia, Ethiopia, 2023.
| Variable | Categories | Frequency | Percent (%) |
| Gravidity | Primigravida | 134 | 45 |
| Multigravida | 150 | 50 | |
| Grand multigravida | 12 | 5 | |
| ANC follow-up | Yes | 272 | 92 |
| No | 24 | 8 | |
| History of preterm birth | Yes | 32 | 11 |
| No | 264 | 89 | |
| History of abortion | Yes | 34 | 12 |
| No | 262 | 88 | |
| PPROM | Yes | 62 | 21 |
| No | 234 | 79 | |
| Preeclampsia | Yes | 168 | 57 |
| No | 128 | 43 | |
| History of CS | Yes | 54 | 18 |
| No | 242 | 82 |
Magnitude of preterm premature rupture of membrane
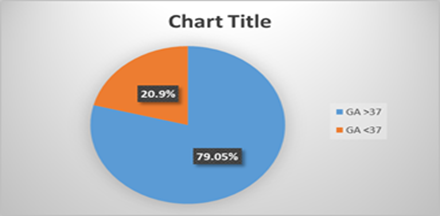
The prevalence of preterm premature rupture of the membrane was 20.9% (95% CI: 16.5-26).
Figure 1: Prevalence of preterm premature rupture of membrane among pregnant women admitted at Bishoftu General Hospital Oromia, Ethiopia, 2023.
Risky lifestyle, and medical history
Pregnant women engaged in a variety of lifestyles during their current pregnancy, including accidental falling 24(8%), lifting heavy objects 26(9%), and daily transportation 242(82%). Even though anemia 14 (5%) and tuberculosis (TB) 8(3%) were less common, hypertensive disorders 168 (57%) were more common among study participants (Table 3).
Table 3: Life style, and medical history of pregnant women admitted at Bishoftu General Hospital Oromia, Ethiopia, 2023.
| Variable | Categories | Frequency | Percent (%) |
| History of alcohol intake | Yes | 12 | 4 |
| No | 284 | 96 | |
| Abnormal vaginal discharge | Yes | 16 | 5 |
| No | 280 | 95 | |
| Falling accident | Yes | 24 | 8 |
| No | 272 | 92 | |
| Lifting heavy objects | Yes | 26 | 9 |
| No | 270 | 91 | |
| Daily transportation | Yes | 242 | 82 |
| No | 54 | 18 | |
| Anemia | Yes | 14 | 5 |
| No | 282 | 95 | |
| TB | Yes | 8 | 3 |
| No | 288 | 97 | |
| History of hypertensive disorders | Yes | 168 | 57 |
| No | 128 | 43 |
Factors associated with PPROM
After controlling for confounders, previous preterm premature rupture of membrane, preterm delivery, abortion, and cesarean section were all significantly associated with preterm premature rupture of membrane. Participants with a history of PROM had a significantly lower risk of developing PPROM than those who did not have a history of PROM (AOR = 0.27, 95% (CI: 0.7–0.6). Having a history of previous preterm delivery makes pregnant women nearly seven times more likely to have PPROM than just not having a history of preterm delivery (AOR = 7.3, 95% (CI: 1.97 - 27.19). Furthermore, women who had a previous history of abortion were six times more likely to develop PPROM than those who did not (AOR = 6.98, 95% (CI: 1.36–35.74) and those who had a previous history of CS were five times more likely to develop PPROM than those who did not (AOR = 5.26 (95% (CI: 1.65– 16.7) (Table 4).
Table 4: Factors associated with preterm premature rupture of membrane among pregnant women admitted at Bishoftu General Hospital Oromia, Ethiopia, 2023.
| Variable with categories | Preterm PROM | COR (95%CI) | AOR (95%CI) | P value | ||
| Yes (%) | No (%) | |||||
| Monthly income | 1000-2000 | 20(18.2%) | 90(81.8%) | 3.6(1.3-10.3) | 5.1(0.8-31.6) | 0.08 |
| 2000-4000 | 24(21.1%) | 90(78.9%) | 3.0(1.068-8.428) | 1.8(0.3-11.4) | 0.51 | |
| 4000-6000 | 10(18.5%) | 44(81.5%) | 3.5(1.11-11.2) | 3.3(0.41-26.7) | 0.26 | |
| >6000 | 8(44.4%) | 10(55.6%) | 1 | 1 | ||
| History of previous PROM | Yes | 30(55.6%) | 24(44.4%) | 0.16(0.1-0.3) | 0.21(0.7-0.6) * | 0.003 |
| No | 18(16.7%) | 90(83.3%) | 1 | 1 | ||
| History of preterm delivery | Yes | 4(12.5%) | 28(87.5%) | 3.6(1.2-10.9) | 7.3(1.9-27.2) * | 0.003 |
| No | 44(33.8%) | 86(66.2%) | 1 | 1 | ||
| History of abortion | Yes | 2(5.9%) | 32(94.1%) | 8.9(2.1-39.2) | 6.98(1.4-35.7) * | 0.02 |
| No | 46(35.9%) | 82(64.1%) | 1 | 1 | ||
| History of CS | Yes | 8(14.8%) | 46(85.2%) | 3.4(1.45-7.9) | 5.26(1.65-16.7) * | 0.005 |
| No | 40(37.0%) | 68(63.0%) | 1 | 1 | ||
| Preeclampsia | Yes | 22(13.1%) | 146(86.9%) | 3.02(1.7-5.41) | 0.9(0.34-2.6) | 0.9 |
| No | 40(31.3%) | 88(68.8%) | 1 | 1 | ||
| Variable with categories | Preterm PROM | COR (95%CI) | AOR (95%CI) | P value | ||
| Yes (%) | No (%) | |||||
| Monthly income | 1000-2000 | 20(18.2%) | 90(81.8%) | 3.6(1.3-10.3) | 5.1(0.8-31.6) | 0.08 |
| 2000-4000 | 24(21.1%) | 90(78.9%) | 3.0(1.068-8.428) | 1.8(0.3-11.4) | 0.51 | |
| 4000-6000 | 10(18.5%) | 44(81.5%) | 3.5(1.11-11.2) | 3.3(0.41-26.7) | 0.26 | |
| >6000 | 8(44.4%) | 10(55.6%) | 1 | 1 | ||
| History of previous PROM | Yes | 30(55.6%) | 24(44.4%) | 0.16(0.1-0.3) | 0.21(0.7-0.6) * | 0.003 |
| No | 18(16.7%) | 90(83.3%) | 1 | 1 | ||
| History of preterm delivery | Yes | 4(12.5%) | 28(87.5%) | 3.6(1.2-10.9) | 7.3(1.9-27.2) * | 0.003 |
| No | 44(33.8%) | 86(66.2%) | 1 | 1 | ||
| History of abortion | Yes | 2(5.9%) | 32(94.1%) | 8.9(2.1-39.2) | 6.98(1.4-35.7) * | 0.02 |
| No | 46(35.9%) | 82(64.1%) | 1 | 1 | ||
| History of CS | Yes | 8(14.8%) | 46(85.2%) | 3.4(1.45-7.9) | 5.26(1.65-16.7) * | 0.005 |
| No | 40(37.0%) | 68(63.0%) | 1 | 1 | ||
| Preeclampsia | Yes | 22(13.1%) | 146(86.9%) | 3.02(1.7-5.41) | 0.9(0.34-2.6) | 0.9 |
| No | 40(31.3%) | 88(68.8%) | 1 | 1 | ||
*P-value less than 0.05
Discussion
This research intended to determine the magnitude and risk factors for preterm premature membrane rupture. The magnitude of preterm premature membrane rupture was 20.9% (95% CI: 16.5-26). This finding was higher than the studies conducted in India 2.01% [16], Brazil 3.1% [17], China 19.2% [18], Kampala International University teaching hospital in Uganda 7.5% [4] and Debre Tabor of Ethiopia 13.67% [15]. The disparity could be attributed to lower standards of health care, low economic status, and social life in developing countries. The study participants were also from high-risk populations/admitted pregnant women rather than those living in the community, which increased the magnitude of PPROM. In addition, this study was done in areas where poor nutritional status was high.
The previous history of PROM was found to be significantly associated with PPROM in this study. Pregnant women with a history of PROM were nearly 0.3 times less likely than those who did not have a history of PROM to develop PPROM (AOR = 0.27, 95% (CI: 0.7–0.6). The rate of PPROM was decreased by 70% among women who have experienced PPROM during the past pregnancy. This result is consistent with the findings in Mekele, and Debre Tabor General Hospital in Ethiopia [15,19]. This could be because a woman with a history of certain complications was labeled as high-risk. This enables the woman to have more frequent ANC follow-ups, which may aid in early detection and treatment.
Women who had a history of previous preterm birth were seven times more likely to develop PPROM than those who had no history of preterm birth (AOR = 7.3, 95% (CI: 1.97 - 27.19). This finding is comparable with studies done in Indonesia [7], Ethiopia [11, 15], India [16] and China [20]. The association between PROM and preterm birth can be explained biologically by intrapartum infection triggering pro-inflammatory cytokines and interleukin, stimulating the fetal membrane and maternal decidua to release prostaglandins and metalloproteinase matrix enzymes or proteases, and then thinning of the cervix leading to stimulation of uterine contractions together cause preterm birth.
The previous history of abortion was another factor depicted that has an association with PPROM. Pregnant women with a history of abortion in pregnancy were almost seven times more likely to get PPROM than those who did not (AOR = 6.98, 95% (CI: 1.36–35.74). The studies conducted in Korea [16,21], Uganda [4], and Ethiopia [10, 11, 22, 23] reported similar findings. This may be explained by the fact that women who have previously had an abortion—especially an unsafe one—are more likely to experience intra-amniotic and intrapartum infections, which can lead to PROM. Additionally, women who have had multiple abortions are more likely to have a shorter cervix, which is linked to an increased risk of PROM. Additionally, dilatation and curettage disrupt cervical and uterine elasticity leading to uterine scaring and cervical incompetence. As a result, health professionals should give mothers who have previously had abortions extra consideration by providing health promotion during ANC.In this study, women with a history of previous cesarean section were five times more likely to develop PPROM than those who do not have the history (AOR = 5.26 (95% (CI: 1.65– 16.7). Previous cesarean delivery was documented in research conducted in Korea [21], China [18], and Ethiopia [6, 15, 22, 23], and was linked to PPROM. The possible reasons could be the scar formed due to cesarean section leading to PROM as the consequence of pregnancy.
Limitations
Due to logistics, the study was conducted only in the hospital, though several women were delivering at health centers in the town. Hence, the finding of the study is only generalizable to hospitals throughout the region.
Conclusion
The magnitude of preterm premature rupture of the membrane was high in the study area. History of previous preterm delivery (AOR=7.3, 95% (CI: 1.97, 27.19), previous history of abortion (AOR = 6.98, 95% (CI: 1.36–35.74), and history of previous CS (AOR = 5.26 (95% (CI: 1.65–16.7) were factors significantly linked to PPROM. Early identification of high-risk pregnancies leading to preterm premature membrane rupture should be promptly managed. A longitudinal study depicting the causes of PPROM needs to be conducted.
Declarations
Data
Data is available upon request from the corresponding author at reasonable request.
Conflict of interest
Authors declare there is no conflict of interest
Consent to publish
Not applicable
Fund
No fund was received for this research
Author’s contribution
BZ made the conception. WM involved in designing the study, data acquisition, availing resources, data management, and wrote the manuscript. All authors read and approved the manuscript.
References
- (2016). ACOG. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice Bulletin No. 172: Premature Rupture of Membranes. Obstet Gynecol, 128(4):e165-177.
Publisher | Google Scholor - Movahedi M, Rezaie M, Taefnia AM. (2013). Maternal and fetal outcomes of preterm premature rupture of membrane. J Isfahan Med Sch, 30(216):2134-2139.
Publisher | Google Scholor - Park JH, Bae JG, Chang YS. Neonatal Outcomes According to the Latent Period from Membrane Rupture to Delivery Among Extremely Preterm Infants Exposed to Preterm Premature Rupture of Membrane: A Nationwide Cohort Study. J Korean Med Sci, 36(14):1-2.
Publisher | Google Scholor - Byonanuwe S, Nzabandora E, Nyongozi B, Pius T, Ayebare DS, Atuheire C, et al. (2020). Predictors of Premature Rupture of Membranes among Pregnant Women in Rural Uganda: A Cross-Sectional Study at a Tertiary Teaching Hospital. Int J Reprod Med, 1-6.
Publisher | Google Scholor - Dagnew N, Tazebew A, Ayinalem A, Muche A. (2020). Measuring newborn foot length to estimate gestational age in a high-risk Northwest Ethiopian population. 1-12.
Publisher | Google Scholor - Telayneh AT, Ketema DB, Mengist B, Yismaw L, Bazezew Y, Birhanu MY, et al. (2023). Pre-labor rupture of membranes and associated factors among pregnant women admitted to the maternity ward, Northwest Ethiopia. PLOS Glob Public Heal, 3(3):e0001702.
Publisher | Google Scholor - Sari IM, Adisasmita AC, Prasetyo S, Amelia D, Purnamasari R. (2020). Effect of premature rupture of membranes on preterm labor: a case-control study in Cilegon, Indonesia. Epidemiol Health, 42:1-6.
Publisher | Google Scholor - Sahoo S, Rath K, Behera A, Nayak N. (2023). Prevalence Of Preterm Premature Rupture of Membrane and Its Associated Factors Among the Pregnant Women in The Selected Tertiary Carehospital, Bhubaneswar, Odisha. 14(03):3290-3300.
Publisher | Google Scholor - (2021). Obstetrics management protocol FOR HOSPITALS. Ethiopian Federal Ministry of Health.
Publisher | Google Scholor - Getnet A, Oljira L, Assefa N, Tiruye G, Figa Z. (2023). Determinants of premature rupture of membrane among pregnant women in Harar town, Eastern Ethiopia: A case-control study. Heliyon, 9(4):e15445.
Publisher | Google Scholor - Argaw M, Mesfin Y, Geze S, Nuriye K, Tefera B, Embiale A, et al. (2021). Preterm Premature Ruptures of Membrane and Factors Associated among Pregnant Women Admitted in Wolkite Comprehensive Specialized Hospital, Gurage Zone, Southern Ethiopia. Infect Dis Obstet Gynecol.
Publisher | Google Scholor - Assefa NE, Berhe H, Girma F, Berhe K, Berhe YZ, Gebreheat G, et al. (2018). Correction to: Risk factors of premature rupture of membranes in public hospitals at Mekele city, Tigray, a case control study. BMC Pregnancy Childbirth, 18(1):1-7.
Publisher | Google Scholor - Tesfaye AY, Gudina E, Berhanu S DM. (2020). Khat chewing in pregnant women associated with prelabor rupture of membranes, evidence from eastern Ethiopia. Pan Afr Med J, 8688:1-9.
Publisher | Google Scholor - Getnet A, Oljira L, Assefa N, Tiruye G, Figa Z. (2023). Determinants of premature rupture of membrane among pregnant women in Harar town, Eastern Ethiopia: A case-control study. Heliyon, 9(4):455-466.
Publisher | Google Scholor - Addisu D, Melkie A, Biru S. (2020). Prevalence of Preterm Premature Rupture of Membrane and Its Associated Factors among Pregnant Women Admitted in Debre Tabor General Hospital, North West Ethiopia: Institutional-Based Cross-Sectional Study. Obstet Gynecol Int, 1-7.
Publisher | Google Scholor - Mohan SS, Thippeveeranna C, Singh NN, Singh LR. (2017). Analysis of risk factors, maternal and fetal outcome of spontaneous preterm premature rupture of membranes: a cross sectional study. Int J Reprod Contraception, Obstet Gynecol, 6(9):3781.
Publisher | Google Scholor - Hackenhaar AA, Albernaz EP, Fonseca TMVD. (2014). Preterm premature rupture of the fetal membranes: Association with sociodemographic factors and maternal genitourinary infections. J Pediatr (Rio J), 90(2):197-202
Publisher | Google Scholor - Chandra I, Sun L. (2017). Third trimester preterm and term premature rupture of membranes: Is there any difference in maternal characteristics and pregnancy outcomes? J Chinese Med Assoc, 80(10):657-661.
Publisher | Google Scholor - Assefa NE, Berhe H, Girma F, Berhe K, Berhe YZ, Gebreheat G, et al. (2020). Correction to: Risk factors of premature rupture of membranes in public hospitals at Mekele city, Tigray, a case control study. BMC Pregnancy Childbirth, 20(1):1-7.
Publisher | Google Scholor - Zhang LX, Sun Y, Zhao H, Zhu N, Sun X De, Jin X, et al. (2017). A bayesian stepwise discriminant model for predicting risk factors of preterm premature rupture of membranes: A case-control study. Chin Med J (Engl), 130(20):2416-2422.
Publisher | Google Scholor - Choi EK, Kim SY, Heo JM, Park KH, Kim HY, Choi BM, et al. (2021). Perinatal outcomes associated with latency in late preterm premature rupture of membranes. Int J Environ Res Public Health, 18(2):1-9.
Publisher | Google Scholor - Tiruye G, Shiferaw K, Tura AK, Debella A, Musa A. (2021). Prevalence of premature rupture of membrane and its associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis. SAGE Open Med, 9.
Publisher | Google Scholor - Habte A, Dessu S, Lukas K. (2021). Determinants of premature rupture of membranes among pregnant women admitted to public hospitals in Southern Ethiopia, 2020: A hospital-based case–control study. Int J Womens Health, 13:613-626.
Publisher | Google Scholor