Research Article
Magnitude and Predictors of Surgical Site Infection After Caesarean Section in Two Referral Hospitals in Cameroon: A Prospective Study
1Department of obstetrics and Gynaecology, Faculty of Health Sciences, University of Buea, Cameroon.
2Department of obstetrics and Gynaecology, Douala Gynaeco-obstetrics and paediatric Hospital, Cameroon.
3Department of obstetrics and Gynaecology, Douala General Hospital, Cameroon.
4Department of Surgery and Specialities, Faculty of Medicine and Pharmaceutical Sciences, University of Douala, Cameroon.
5Department of obstetrics and Gynaecology, Douala Laquintinie Hospital, Cameroon.
6Faculty of Medicine and Pharmaceutical Sciences, University of Dschang, Cameroon.
*Corresponding Author: Diane Estelle Kamdem, epartment of obstetrics and Gynaecology, Faculty of Health Sciences, University of Buea, Cameroon.
Citation: Tchouzou R, Theophile N Njamen, Fulbert M Nkwele, Essome H, Elise M E Mimesse, et, al. (2024). Magnitude and Predictors of Surgical Site Infection after Caesarean Section in Two Referral Hospitals in Cameroon: A Prospective Study, Journal of Women Health Care and Gynecology, BioRes Scientia Publishers, 3(2):1-9. DOI: 10.59657/2993-0871.brs.23.021
Copyright: ©2024 Robert Tchounzou, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: October 09, 2023 | Accepted: February 26, 2024 | Published: February 17, 2024
Abstract
Background: Caesarean section (CS) is increasingly being preferred to vaginal delivery in Cameroon despite the alert of WHO in 2015. Compared to vaginal delivery, CS is associated to increase rates of maternal complications like surgical site infections (SSI). Incidence and risk factors of surgical site infections after CS have been described in international literature and some peripheral hospitals in Cameroon but little is known on these in the referral hospitals.
Objectives: to determine the incidence and risk factors of SSI in two referral hospitals in Douala, Cameroon.
Methods: A prospective study enrolling a cohort of patients who underwent CS from February, 01 to July 31, 2022 was conducted. Socio-demographic, obstetrical and management information were recorded using a standardized form. Descriptive statistics and multiple logistic regression were used to determine associations between factors and occurrence of SSI. Statistical significance was set at p<0.05.
Results: 444 Women were enrolled in our study and 45 presented SSI, making an incidence of 10.13%. The incidence of SSI was 6.45% in Douala Gynaeco-obstetric and Paediatric Hospital and 11.11% in Laquintinie. After bivariate analysis, obesity, pre-surgical anemia, diabetes and Blood transfusion were associated to SSI. The same factors were confirmed as predictors of SSI after multivariate analysis: Obesity (aOR=5.9, p=0.032), pre-surgical anemia (aOR=4.7, p=0.03), diabetes (aOR=15.7, p=0.013) blood transfusion: aOR=0.05, p=0.013).
Conclusion: SSI is high in in two referral hospitals in Douala. Risk factors include pre-surgical Anaemia, Diabetes, obesity and blood transfusion.
Keywords: surgical site infection; caesarean section; referral hospital; incidence; risk factors
Introduction
Background
Caesarean section is a surgical procedure in which a baby is taken out through an incision done on a woman’s abdomen and uterus. This surgical intervention is usually done when the vaginal delivery may be detrimental to the foetus, the mother or both in situations like prolonged labour, foetal distress or others [1]. Since 1985, WHO and the international scientific community have established that caesarean sections (CS) rates of 10 to 15% at community level are the ideal indicators of good obstetrical practice; and worldwide, CS is increasingly been preferred to vaginal delivery, reaching 54.4% of cases in Turkey, 47.5% in South Korea and 38.97% in Poland despite the WHO’s statement in 2015 that a CS rate of more than 30% at community level may not yield any benefits for the mother and her child [ 2, 3]. Compared to vaginal delivery, CS is associated with more maternal and foetal complications at immediate and long term periods, with reported rates of up to 22.7% in Cameroon [4].
Surgical site infection (SSI) is among the commonest post caesarean section complications both in developed and developing countries. European Centre for Disease control (ECDC) defines surgical site infection as any infection of the skin and subcutaneous tissue at the operation site, the deep soft tissue and/or any organ or spaces other than skin that was manipulated and within 30 days of procedure [5].
WHO indicates that SSI are the most reported type of Health care associated infection (HAIs) in low and middle-income countries with an incidence of 11.8 episodes per 100 surgical procedures [6]. The rate of SSI after a caesarean section range from 3% to 15
Materials and Methods
This prospective study was conducted over a period of 6 months from February 01, 2022 to July 31, 2022 at the Laquintinie Hospital and the Douala Gynaeco-obstetric and Paediatric hospital. The two hospitals serve both as teaching hospitals and receive referrals from the Douala metropolis. LQ realises a mean number of 2900 births per year of which nearly one-third (950) is by caesarean section. This hospital receives all categories of patients with various economical capacities and the cost of the treatment is mainly supported by the patients themselves. The obstetrical theatre unit is dedicated to obstetrical surgeries but also to other types of gynaecological surgeries like laparotomy for ectopic pregnancy, myomectomy, hysterectomy. Owing to the trainees from various medical and paramedical schools of the country who are trained here, the important turnover of patients, the aseptic conditions are suboptimal.
The Douala Gynaeco-obstetric and Paediatric hospital on its own is mainly dedicated to mother and child care. It provides quality care and contributes to professional training and staff development. A mean number of 550 to 600 deliveries are conducted here every year with about ¼ through caesarean sections. Management of labour and related complications are done following in-service guidelines which include infection prevention measures. Caesarean sections are done either by obstetricians or senior resident doctors under the supervision of a consultant. The theatre unit has an operating room where cases of obstetrical and gynaecological surgeries are managed apart from cases of abscesses. Infection prevention guidelines measures are implemented on accessing to theatre, wearing the theatre attires and other operating equipment.
All women who underwent CS during the study period were consented and included in the study. Women who failed to answer part or all the questionnaire or those who died immediately or before 30 days after CS without any diagnosis of SSI were excluded. We used a standardized data collection tool to record preoperative, intraoperative and postoperative information of each patient who underwent CS. Preoperative information concerned socio-demographic (age, telephone number, education level, occupation), obstetrical data (parity, gestational age, previous caesarean section, duration of the labor, duration of rupture of membranes). Other information included mode of admission (elective or emergency), patient managed in the site or referred, body mass index (BMI) and Hemoglobin level. The time of insertion of urinary catheter and the shaving of surgical site were also recorded.
Intraoperative data were: the type of anesthesia, the qualification of the surgeon (obstetrician or resident-doctor), the duration of surgery, the use of antibiotic, the quantity of blood loss and any intraoperative complication. Postoperative data were: the use of antibiotics; outcome measures were: occurrence of superficial surgical site infection (SSSI), deep incisional infection (DII) or organ/space infection (OI). Diagnosis of SSI criteria: A diagnosis of surgical site infection was based on the CDC criteria of SSI [5]. Superficial incisional infection: involves the skin and the subcutaneous tissues. We needed to have one of the following criteria; purulent discharge from the wound, isolated organism, at least one symptom of infection and diagnosis by the surgeon. Deep incisional infection: involves deep tissues (muscles and fascial planes). One of the following criteria was necessary: purulent discharge from the wound, dehiscence or deliberate reopening of the deep incision by the surgeon after suspecting an infection, evidence of abscess formation or other deep infection diagnosed by the surgeon.
Organ/space infection: involves any organ apart from the incision site but must be related to the surgical procedure: purulent discharge from the drain placed in the organ, isolated organism from the organ, abscess or infection involving the organ. Participants were reviewed systematically at day 4 when the dressing of surgical site was done according to service guidelines and after every 2 days till day 12 at LQ whereas the patient was asked to come back after 3 days at DGOPH. After this routine period of monitoring, patients with SSI were identified and appropriate treatment started according to hospital protocols whereas those with no infection were discharged home. Before discharge, participants received counseling on presumptive signs of SSI which are; pain, fever, localized swelling, redness, purulent drainage from the incision site, heat of skin and wound dehiscence. This would enable the patient to recognize the infection at home and inform the research team. All participants were systematically reviewed at day 30 for assessment and closure of the study.
Data was analyzed using EpiInfo 7. Categorical variables (occupation, education level, comorbidity) were summarized using counts and percentages, presented using a tabular form; continuous variables (age, gestational age, BMI) were summarized using mean, standard deviations, medians and interquartile range where necessary. A chi squaretest was performed to test for significant associations between the predictor and outcomes for categorical variables and Student t-test was used for continuous variables. Odds ratio (OR) with 95% confidence interval was calculated to assess the strength of the association between the risk factors and the occurrence of SSI after bivariate analysis followed by multivariate analysis (aOR) of factors found to be significant after bivariate analysis; the level of significance was set at p less than 0.005.
Results
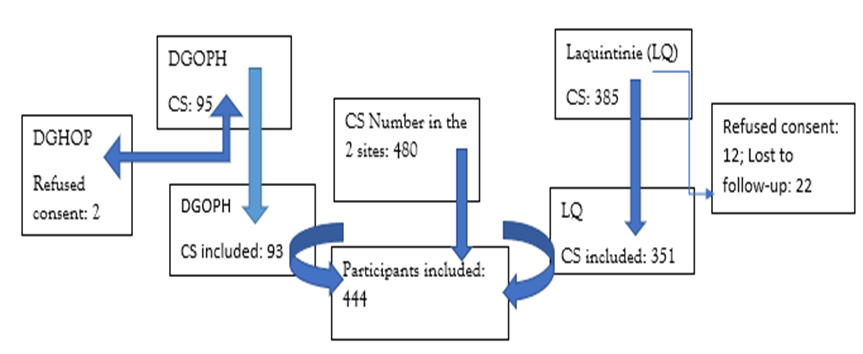
Results chart
Socio-Demographic Characteristics of Participants
The median age of study participants was 29 years and the mean age 29.24±6.46 with extremes of 18 and 42 years. Most of the participants were between the age group 20 to 29 (48.4%). Over fifty-five per cent of participants has no employment (55.85%) and most of them had tertiary level education (49.55%).
Table 1: Sociodemographic characteristics of the study participants.
| Variable | Frequency (n= 444) | Percentages (%) |
| Age group | ||
| <20> | 47 | 10.58 |
| 20-29 | 215 | 48.42 |
| 30-39 | 145 | 32.66 |
| ≥40 | 37 | 8.34 |
| Occupation | ||
| Employed | 196 | 44.15 |
| Unemployed | 248 | 55.85 |
| Level of education | ||
| No formal education | 37 | 8.34 |
| Secondary | 187 | 42.11 |
| Tertiary | 220 | 49.55 |
General characteristics of study population
Three hundred and thirty-two participants (74.78%) had an abnormal body mass index (BMI) with 112 (25.33%) having class II or III obesity. In 34.69% of cases, participants were undergoing repeated CS. Most patients had a normal hemoglobin (Hb) level above 11 g/dl whereas 61(13.73%) were anemic. Caesarean section was done as emergency in the majority of cases (57.88%). The duration of rupture of membranes (ROM) ranged from 0 to 216 hours with a mean of 8.2±32.32 hours and median of 0? (IQRː0-3) hours; in most cases, ROM has lasted less than 12 hours (57.88%). Obstetricians were the main surgeons in (83.11%) and the duration of surgery ranged from 40 minutes to 80 minutes with a mean of 56.09±7.98 minutes and median of 55 (IQRː50-60). Antibiotic use either as prophylaxis or as antibiotherapy was done following the service protocol (appropriate) in 304 (68.47%) cases whereas in 31.53 percentage cases, it was either done with delay or not at all. Over ten per cent of patients had comorbidity with Diabetes mellitus in 4.50% of cases (see table 2).
Table 2: General characteristics (personal, obstetrical and surgical) of study participants.
| Variables | Frequency n = 444 | Percentage (%) | |
| BMI | Underweight | 9 | 2.503 |
| Normal weight | 103 | 23.19 | |
| Overweight | 220 | 49.55 | |
| M. obesity | 112 | 25.23 | |
| Previous CS | No | 290 | 65.31 |
| Yes | 154 | 34.69 | |
| Pre-surgical Hb | < 10> | 61 | 13.73 |
| 10-11 mg/dl | 183 | 41.22 | |
| >11 mg/dl | 200 | 45.05 | |
| Management site | Study site | 271 | 61.03 |
| Referred | 173 | 38.97 | |
| Rupture membranes | < 12> | 257 | 57,88 |
| 12- 18 hours | 150 | 33.78 | |
| >18 hours | 37 | 8,34 | |
| Type of CS | Elective | 187 | 42.12 |
| Emergency | 257 | 57.88 | |
| Grade of surgeon | G. practitioner/ Resident Obgyn | 75 | 16.89 |
| Obstetrician | 369 | 83.11 | |
| Antibiotic use | Appropriate | 304 | 68.47 |
| Inappropriately | 140 | 31.53 | |
| Comorbidity | None | 396 | 89.19 |
| Diabetes | 20 | 4.50 | |
| Others’ | 28 | 6.31 | |
| Blood transfusion | Yes | 23 | 5.18 |
| No | 421 | 94.82 | |
Incidence of SSI
Among the 444 patients included in the study, 45 presented SSI representing an incidence of 10.13%; the incidence was 6 out of 93(6.45%) and 39/351 (11.11%) in DGOPH and LQ respectively. Most SSIs occurred between the 6th and 14th day post-operation with a median time of occurrence of 9 days (IQR 7–12 days). Types of SSI found were superficial SSI 19(42.22%), deep SSI 24 (53.33%) and organ space 2(4.45%). III-5 Bivariate and multivariate analysis of determinants of SSI, After Bivariate analysis, there was no association between socio-demographic characteristics of the participants and the occurrence of SSI.
Table 3: Bivariate analysis of risk factors of SSI
| Variables | SSI (n= 45) | OR (95% CI) | P value | ||
| YES | NO | ||||
| Age(years) | <20> | 4 (8.88) | 43 (10.77) | 1 | |
| 20-29 | 21 (46.66) | 195 (48.87) | 1.1 (0.1-10.6) | 0.94 | |
| 30-39 | 16 (35.55) | 128 (32.08) | 1.33 (0.1-13.53) | 0.81 | |
| ≥40 | 4 (8.88) | 33 (8.27) | 1.2 (0.07-24.38) | 0.87 | |
| Occupation | Not employed | 16 (35.55) | 233 (58.40) | 0.4 (0.1-1.5) | 0.2 |
| Employed | 29 (64.45) | 166(41.60) | 1 | ||
| Education level | No formal | 4(8.88) | 33 (8.27) | ||
| Secondary | 16 (35.56) | 171 (42.86) | 0.83 | ||
| University | 25 (55.56) | 195 (48.87) | 0.98 | ||
| BMI | Underweight | 0 (0.0) | 9 (2.26) | - | |
| Normal weight | 16(35.56) | 87 (21.80) | |||
| Overweight | 9 (20) | 211 (52.88) | 0.48 (0.13-1.81) | 0.2 | |
| Obesity | 20(44.44) | 92 (23.06) | 0.021(0.01-0.93) | 0.03 | |
| Previous CS | YES | 9(20) | 154 (38.60) | 0.56 (0.04-2.93) | 0.54 |
| NO | 36(80) | 245 (61.40) | 1 | - | |
| Pre-surgical Hb level | Anaemia | 16 (35.56) | 228 (57.14) | 4.7 (1.2-19.5) | 0.03 |
| No Anaemia | 29 (64.34) | 171(42.86) | 1 | ||
| Type of CS | Emergency | 37 (8.22) | 220 (55.14) | ||
| Elective | 8 (17.78) | 179 (45.86) | |||
| Antibiotic use | Appropriate | 8 (17.78) | 132 (34.34) | 1.5 (0.3-7.5) | 0.62 |
| inappropriate | 37 (82.22) | 262 (65.56) | 1 | ||
| Rupture of membranes | 0-12 hours | 29(64.44) | 228(57.14) | 1 | |
| 12-18 hours | 12(26.67) | 138(34.58) | 0.7 (0.17-2.9) | ||
| >18 hours | 4(8.89) | 33(8.27) | 0.9 (0.1-9.2) | ||
| Grade of surgeon | Obstetrician | 37(82.22) | 332 (83.21) | 1 | |
| MD/Resident | 8(17.78) | 67(16.79) | 1.1 (0.2-5.7) | 0.9 | |
| Comorbidity | None | 37(82.22) | 359 (89.98) | 1 | |
| Diabetes | 8(17.78) | 12 (3.00) | 8.4 (1.06-28.0) | 0.04 | |
| Others | 0(0) | 28 (7.01) | |||
| Blood transfusion | Yes | 12(26.67) | 11(2.76) | 1 | 1 |
| No | 33(73.33) | 388(97,24) | 0.06 (0.01-0.4) | 0.06 | |
Table 4: Multivariate analysis
| Variable | SSI | aOR (95% CI) | P value | ||
| Yes | No | ||||
| BMI (Obesity) | 20 (44.44) | 92(23.06) | 5.9 (1.17-30.0) | 0.032 | |
| Anaemia | Yes | 16 (35.56) | 228 (57.14) | 1 | |
| No | 29 (64.34) | 171(42.86) | 5.9 (1.17-30.0) | 0.031 | |
| Comorbidities | None | None | 37(82.22) | - | - |
| Diabetes | Diabetes | 8(17.78) | 15.7 (1.7-24.4) | 0.013 | |
| Others | Others | 0(0) | - | ||
| Blood transfusion | No | No | 33(73.33) | 0.05 (0.008-0.39) | 0.004 |
| Yes | Yes | 12(26.67) | 1 | - | |
Discussion
This study aimed at determining the incidence and risk factors of SSI in two referral hospitals of Cameroon where the standard of care is presumably among the highest in the Country. Our study appears to be among the very few in Cameroon with the active surveillance of study participants during 30 days post-surgery to meet the international criteria for SSI [5] compared to others which limited the observation to the duration of postoperative hospital stay; thus, we believe that the incidence found is closer to the real one.
Rates of SSI
We found a cumulative incidence of 10.13% of SSI in this study; the incidence was 6 out of 93(6.45%) and 39/351 (11.11%) in DGOPH and LQ respectively. The odds of having an SSI in Laquintinie hospital was 1.5 times higher than in DGOPH but the difference was not statistically significant Although there is a good level of hygiene and cleanliness in the 2 hospitals the availability of written guidelines on infection prevention measures both in maternity and theatre units in DGOPH could explain the difference.
There is a great variation of SSI rates reported in developing countries with relatively low rates: 1.81% by Fouedjio et al. in Cameroon[14], 3.5% by Sawadogo et al. in 2019 in Burkina Faso [8], 5% by Ghuman [11], and 5.3% by Khaled Gomaa et al. in Egypt [16]. The relative low rates reported in these studies may not reflect the true incidence, given that must of these studies were either retrospective and cross sectional or observation of patients was limited to the period of postoperative hospital stay which is reduced to 4 to 7 days. Authors have clearly demonstrated that when the surveillance is limited to duration of hospital stay, the incidence of SSI is underestimated [17]. Many authors have found incidences of SSI similar to ours [12,18,19] and [9] in settings with similar standards of care. Other authors in Asia and sub-Saharan Africa reported higher incidences of SSI ranging from 18.8% by Jasim et al. in Malaysia [7] to 20.7% by Ngowe Ngowe et al. in Cameroon [20]. Compared to developed countries, the magnitude of SSI is still important due probably to less standard infection prevention measures applied in our settings. In these countries, the incidence ranges between 1 and 3.9% [17,21,22] obtained after a 30-day post caesarean section follow-up of patients.
Risk factors of SSI
After bivariate analysis, the following factors were identified as predictors of SSI: obesity (OR=0.021; CI (0.01– 0.93); p=0.03), pre-surgical anemia (OR=4.7; CI (1.2–19.5); p=0.03) Diabetes (OR=8.4; CI (1.06–28); p=0.04), and blood transfusion (OR=0.01; CI (0.01–0.4); p=0.06). Inappropriate use of antibiotics with an OR = 1.5, p=0.62CI (0.3–7.50) appeared like like a predictor of SSI but not significant and was not retained for the multivariate analysis,
After multivariate logistic regression model, we obtained the following results:
Obesity (aOR=5.9; CI (1.17 – 30); p=0.032), pre-surgical anaemia (aOR=4.7, CI (1.2–19.5); p=0.03) diabetes (aOR=15.7; CI (1.7–24.4); p=0.013), blood transfusion (aOR=0.05; CI (1.7–24.4); p=0.013).
In previous studies conducted both by Tebeu et al. [23] and Fouedjio et al. [14] in Cameroon, risk factors of SSI were prolonged premature of membranes, patients operated by junior resident physicians and midline incision. These factors were not identified as predictors in our study. In fact, the midline incision was exceptional in the study site and the resident doctors performed CS under strict supervision of senior consultant according to in-service protocols and these reasons could account for the difference. In accordance with many other authors, anemia and blood transfusion were independent risk factors of SSI [1, 24–26] of SSI in our study. Anemia is a common finding in our settings with financial constraints and absence of health coverage scheme; anaemia has been proven to delay surgical healing process and the blood transfusion administered to correct this could induce immunomodulation and expose the patient to risk of post-surgery infection [27].
Obesity and Diabetes mellitus were also found to have strong association with the occurrence of SSI. Obesity is a known risk factor of Diabetes mellitus and the later can induce changes and modifications in the vascular and immunologic systems [28,29]; The association between increasing body weight and the safety of surgical procedures has been thoroughly documented in the scientific literature [30, 31]. Although not identified like a significant risk factor, inappropriate antibiotic use was observed in LQ (late administration of prophylactic antibiotics in cases of emergency, irregular or absence of prescribed antibiotics in the post-operative period) and has 1.5 odds of predicting SSI. In fact, an important proportion(69.63%) of patients pay health care services fees from out-of-their pockets and it is not unusual that referred patients with indications of emergency CS present as destitute, unable to comply with treatment [32]. The role of antibiotic prophylaxis in elective surgery or antibiotherapy in contaminated surgery has been abundantly highlighted in the literature and guidelines on their use clearly edited [29, 6,33,34]. Other risk factors reported in the literature have not been evidenced in our study. These include number of vaginal examinations, prolong labor, prolonged rupture of membranes.
Conclusion
The magnitude of SSI remains high in our settings and multiple modifiable factors have been identified during this study including obesity, diabetes mellitus, and severe anaemia. Targeted strategies to reduce the burden of this include the old paradigm of development and strict implementation of infection prevention protocols and fight against obesity.
Declarations
Funding
No funding was received.
Authors’ contributions
RT, TNN, FGMN, and EMEM designed the study and recruited study participants. DK participated in in participants ‘recruitment and reviewed the manuscript. RT in addition wrote the manuscript. HE and TNN revised and scrutinized the study for important intellectual content. All the authors read and approved the final version of the manuscript.
Competing interests
Authors declare no competing interest.
References
- Gelaw KA, Aweke AM, Astawesegn FH, Demissie BW, Zeleke LB. (2017). Surgical site infection and its associated factors following cesarean section: a cross sectional study from a public hospital in Ethiopia. Patient Saf Surg, 11:18.
Publisher | Google Scholor - C-Section Rates by Country 2023. World population review.
Publisher | Google Scholor - WHO statement on caesarean section rates.
Publisher | Google Scholor - Henri E, Valere MK, Paul EJ, Merlin B, Felix E, Grâce TT, et al. (2019). Caesarean Section in African Setting: Current Situation, Problematic and Qualitative Approaches at Laquintinie Hospital (Douala, Cameroon). Open J Obstet Gynecol, 9(10):1392-1406.
Publisher | Google Scholor - Zejnullahu VA, Isjanovska R, Sejfija Z, Zejnullahu VA. (2019). Surgical site infections after cesarean sections at the University Clinical Center of Kosovo: rates, microbiological profile and risk factors. BMC Infect Dis, 9(1):752.
Publisher | Google Scholor - Pathak A, Mahadik K, Swami MB, Roy PK, Sharma M, Mahadik VK, et al. (2017). Incidence and risk factors for surgical site infections in obstetric and gynecological surgeries from a teaching hospital in rural India. Antimicrob Resist Infect Control, 6(1):66.
Publisher | Google Scholor - Jasim HH, Sulaiman SAS, Khan AH, Dawood OT, Abdulameer AH, Usha R. (2017). Incidence and Risk Factors of Surgical Site Infection Among Patients Undergoing Cesarean Section. Clin Med Insights Ther,9:117.
Publisher | Google Scholor - Sawadogo YA, Komboigo E, Kiemtore S, Zamane H, Ouedraogo I, Kain DP, et al. (2019). Parietal suppurations after cesarean section at the Yalgado Ouédraogo University Hospital, Burkina Faso: epidemiological clinical, therapeutic and prognostic aspects. Pan Afr Med J, 32.
Publisher | Google Scholor - Wodajo S, Belayneh M, Gebremedhin S. (2017). Magnitude and factors associated with post-cesarean surgical site infection at Hawassa University Teaching and referral hospital, southern Ethiopia: a cross-sectional study. Ethiop J Health Sci, 27(3):283-290.
Publisher | Google Scholor - Bizuayew H, Abebe H, Mullu G, Bewuket L, Tsega D, Alemye T. (2021). Post-cesarean section surgical site infection and associated factors in East Gojjam zone primary hospitals, Amhara region, North West Ethiopia, 2020. PLoS ONE, 16(12):0261951.
Publisher | Google Scholor - Ghuman M, Rohlandt D, Joshy G, Lawrenson R. (2011). Post-caesarean section surgical site infection: rate and risk factors. N Z Med J, 124(1339):32-36.
Publisher | Google Scholor - Opøien HK, Valbø A, Grinde-Andersen A, Walberg M. (2007). Post-cesarean surgical site infections according to CDC standards: rates and risk factors. A prospective cohort study. Acta Obstet Gynecol Scand, 86(9):1097-1102.
Publisher | Google Scholor - Mbakwa MR, Tendongfor N, Ngunyi YL, Ngek ESN, Alemkia F, Egbe TO. (2021). Indications and outcomes of emergency obstetric hysterectomy; a 5-year review at the Bafoussam Regional Hospital, Cameroon. BMC Pregnancy Childbirth, 21(1):323.
Publisher | Google Scholor - Fouedjio JH, Mbongo JA, Kamdem TA, Meka EJ, Fouelifack YF, Nkwabong E, et al. Facteurs Associés aux Infections du Site Opératoire après Césarienne à Yaoundé.: Infections du site opératoire après césarienne. Health Sci Dis, 22(10).
Publisher | Google Scholor - SCHLESSELMAN JJ. (1974). Sample size requirements in cohort and case-control studies of disease. Am J Epidemiol, 99(6):381-384.
Publisher | Google Scholor - Gomaa K, Abdelraheim AR, El Gelany S, Khalifa EM, Yousef AM, Hassan H. (2021). Incidence, risk factors and management of post cesarean section surgical site infection (SSI) in a tertiary hospital in Egypt: a five-year retrospective study. BMC Pregnancy Childbirth, 21(1):634.
Publisher | Google Scholor - Ferraro F, Piselli P, Pittalis S, Ruscitti LE, Cimaglia C, Ippolito G, et al. (2016). Surgical site infection after caesarean section: space for post-discharge surveillance improvements and reliable comparisons. New Microbiol, 39(2):134-138
Publisher | Google Scholor - Mpogoro FJ, Mshana SE, Mirambo MM, Kidenya BR, Gumodoka B, Imirzalioglu C. (2014). Incidence and predictors of surgical site infections following caesarean sections at Bugando Medical Centre, Mwanza, Tanzania. Antimicrob Resist Infect Control, 3(1):25.
Publisher | Google Scholor - Shrestha S, Shrestha R, Shrestha B, Dongol A. (2014). Incidence and risk factors of surgical site infection following cesarean section at Dhulikhel Hospital. Kathmandu Univ Med J KUMJ, 12(46):113-116.
Publisher | Google Scholor - M. Ngowe Ngowe. FF, Mouafo Tambo and M A Sosso. (2014). Prevalence and Risk Factors Associated with Post Operative Infections in the Limbe Regional Hospital of Cameroon. Open Surg J, 8(1):1-8.
Publisher | Google Scholor - Barbut F, Carbonne B, Truchot F, Spielvogel C, Jannet D, Goderel I, et al. (2004). Surgical site infections after cesarean section: results of a five-year prospective surveillance]. J Gynecol Obstet Biol Reprod (Paris), 33(6 Pt 1):487-496.
Publisher | Google Scholor - Douville SE, Callaway LK, Amoako A, Roberts JA, Eley VA. (2020). Reducing post-caesarean delivery surgical site infections: a narrative review. Int J Obstet Anesth, 42:76-86.
Publisher | Google Scholor - Tebeu PM, Kamdem A, Ngou-Mve-Ngou JP, Meka E, Antaon JSS, Loic MT, et al. (2021). Risk factors for surgical site infections after caesarean section at Yaounde, Cameroon. Int J Reprod Contracept Obstet Gynecol, 10(11):4048-4052.
Publisher | Google Scholor - Yerba K, Failoc-Rojas V, Zeña-Ñañez S, Valladares-Garrido M. (2020). Factors Associated with Surgical Site Infection in Post-Cesarean Section: A Case-Control Study in a Peruvian Hospital. Ethiop J Health Sci, 30(1):95-100.
Publisher | Google Scholor - Jido T, Garba I. (2012). Surgical-site Infection Following Cesarean Section in Kano, Nigeria. Ann Med Health Sci Res, 2(1):33-36.
Publisher | Google Scholor - Mukagendaneza MJ, Munyaneza E, Muhawenayo E, Nyirasebura D, Abahuje E, Nyirigira J, et al. (2019). Incidence, root causes, and outcomes of surgical site infections in a tertiary care hospital in Rwanda: a prospective observational cohort study. Patient Saf Surg, 13:10.
Publisher | Google Scholor - Youssef LA, Spitalnik SL. (2017). Transfusion-related immunomodulation: A reappraisal. Curr Opin Hematol, 24(6):551-557.
Publisher | Google Scholor - Kawakita T, Landy HJ. Surgical site infections after cesarean delivery: epidemiology, prevention and treatment. Matern Health Neonatol Perinatol, 3:12.
Publisher | Google Scholor - Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R, et al. (2016). Diabetes and Risk of Surgical Site Infection: A Systematic Review and Meta-analysis. Infect Control Hosp Epidemiol, 37(1):88-99.
Publisher | Google Scholor - Vermillion ST, Lamoutte C, Soper DE, Verdeja A. (2000). Wound infection after cesarean: effect of subcutaneous tissue thickness. Obstet Gynecol, 95(6 Pt 1):923-926.
Publisher | Google Scholor - Myles TD, Gooch J, Santolaya J. (2002). Obesity as an independent risk factor for infectious morbidity in patients who undergo cesarean delivery. Obstet Gynecol, 100(5 Pt 1):959-964.
Publisher | Google Scholor - Ntembe A, Tawah R, Faux E. (2021). Redistributive effects of health care out-of-pocket payments in Cameroon. Int J Equity Health, 20(1):227.
Publisher | Google Scholor - Misganaw D, Linger B, Abesha A. (2020). Surgical Antibiotic Prophylaxis Use and Surgical Site Infection Pattern in Dessie Referral Hospital, Dessie, Northeast of Ethiopia. BioMed Res Int.
Publisher | Google Scholor - Alsaeed OM, Bukhari AA, Alshehri AA, Alsumairi FA, Alnami AM, Elsheikh HA, et al. (2022). The Use of Antibiotics for the Prevention of Surgical Site Infections in Two Government Hospitals in Taif, Saudi Arabia: A Retrospective Study. Cureus, 14(7).
Publisher | Google Scholor