Case Report
Loss of Vision in a Division I Basketball Player
- Rock Vomer 1*
- Rayghan Larick 3
- Emma York 2
- Chris Fungwe 2
- Abigail Bent 2
- Dusty Narducci 1
- Kristin Terry 1
1Department of Family and Community Health and Department of Orthopedics, Division of Sports Medicine, Duke University, Durham, USA.
2Family and Community Medicine (York), Eastern Virginia Medical School, Norfolk, USA.
3Department of Family & Sports Medicine, University of South Florida, Tampa FL, Research Collaborator Department of Family Medicine Mayo Clinic Jacksonville Florida, USA.
*Corresponding Author: Rock Vomer, Department of Family and Community Health and Department of Orthopedics, Division of Sports Medicine, Duke University, Durham, USA.
Citation: Vomer R., Larick R., York E., Fungwe C., Bent A., Narducci K. Terry. et al. (2023). Loss of Vision in A Division I Basketball Player, Clinical Case Reports and Studies, BRS Publishers. 2(4); DOI: 10.59657/2837-2565.brs.23.037
Copyright: © 2023 Rock Vomer, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 05, 2023 | Accepted: May 17, 2023 | Published: May 23, 2023
Abstract
We present a case report of a 20-year-old cis female division 1 collegiate basketball athlete who presented to her team physician with concerns for bilateral temporal, throbbing headache and sudden-onset, non-traumatic, right eye irritation and blurred vision. She was found to have optic neuritis and ultimately diagnosed with multiple sclerosis (MS). Although MS is the most common progressive neurologic disease of young adults there is limited research on athletes with MS. While the pathogenesis of MS remains unknown, current science identifies MS as a multifactorial condition influenced by both environmental and genetic factors. MS has a female predominance and presents most often between the ages of 20 to 45 years old. Since musculoskeletal and/or neurological symptoms are often the first sign of MS it is necessary for healthcare professionals caring for athletes to be familiar with the diagnosis, management and prognosis of MS. This case presents several key themes that aim to assist clinicians caring for athletes with MS. MS can present similar to sports-related injuries (e.g., concussions, overtraining, psychosocial stressors, musculoskeletal injuries) therefore diagnosis in the athletic population is easily missed. Without a healthcare team familiar with the immediate and future needs of the athlete, subpar preliminary and continuous treatment may result in devastating health changes and career ending consequences in athletes. Treatment goals must also align with the patient's athletic goals. Additionally, this case highlights unforeseen ethical and clinical obstacles including the repercussions of the COVID-19 pandemic that must be considered by clinicians involved in the medical care of athletes.
Keywords: vision; basketball; stressors; sclerosis
Introduction
MS, the most common progressive neurologic disease of young adults significantly impacts an individual’s current and future physical and psychological well-being. Symptoms associated with MS present similarly to other musculoskeletal conditions therefore diagnosis in the athletic population can be easily overlooked. Unfortunately, there is limited research assessing the association of physical activity with the risk of incident and prognosis of MS as well as specific recommendations for diagnosing and managing MS in athletes. Individuals with MS who engage in moderate exercise have demonstrated improved muscular performance, sleep quality and cardiovascular health. Clinicians working with athletes should consider MS as a differential diagnosis when appropriate and expect to manage potential ethical and clinical challenges that should arise including prevention of injury, sporting organizations, and worldwide pandemics.
Case Presentation
History
A 20-year-old cis female division 1 collegiate basketball athlete presented with concerns for bilateral temporal, throbbing headache and sudden-onset, non-traumatic, right eye irritation and blurring of vision that had worsened over the past 48 hours. She described the blurry vision as peripherally located and exacerbated by bright lighting. She denied eye pain at rest or with eye movement as well as discharge, visual color changes, fever, double vision, balance or hearing changes, nausea, recent illness, and changes in speech.
She has no known medical problems, past surgeries, or use of medications. Four months prior, during a sport’s pre-participation physical, her visual acuity was reported as 20/20 without corrective lenses. She denies recent changes in her health aside from a now resolved traumatic ankle sprain and piriformis syndrome that developed due to overuse following her ankle injury. She reports no pertinent personal or family history.
On initial exam, her vitals were normal and similar to prior preparticipation physical exams. Snellen chart exam revealed her baseline visual acuity, extraocular motions were normal and painless, and pupils dilated appropriately. Cranial nerve testing as well as upper body neurovascular exam showed no impairments. Balance and proprioception demonstrated no abnormalities.
The athlete declined referral to ophthalmology but agreed to return for reassessment. 72 hours following her initial presentation she continued to have eye symptoms and was evaluated by an ophthalmologist where she was diagnosed with right optic neuritis. The team physician admitted her to the affiliated hospital for further testing and management.
Objective Findings
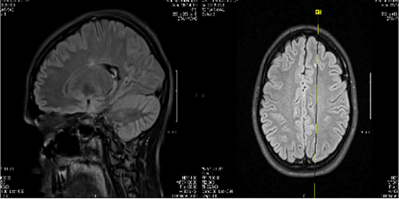
At the time of admission, physical exam revealed new left deep tendon hyperreflexia and mild weakness of bilateral lower extremities with ankle clonus, Babinkski reflex, or spasticity. Laboratory studies including complete blood count, serum vitamin B12, c-reactive protein, Lyme disease titers, rapid plasma regain, antinuclear antibody, complete metabolic profile, Vitamin D, HIV, lead, and drug screening were negative or within normal range. Magnetic resonance imaging (MRI) of the brain and orbits found right optic nerve enhancement and numerous small, non-enhancing periventricular and juxtacortical T2 hyperintensities (Figure 1). There was no evidence of demyelinating disease on MRI of the cervical and thoracic spine. Lumbar puncture was positive for Oligoclonal bands, Anti-Myelin oligodendrocyte Glycoprotein (anti-MOG) Anti-Myelin basic Protein (anti-MBP). Upon further questioning the athlete denied a history of seizures, progressive ataxia, cognitive dysfunction, drug use, and peripheral neuropathy.
Figure 1: MRI demonstrating numerous small, non-enhancing periventricular and juxtacortical T2 hyperintensities.
Differential Diagnosis
The differential diagnosis for this case presentation is broad and included a diagnostic investigation to assess for neurologic, cardiac and ophthalmologic causes of the athlete’s symptoms. At her initial presentation conditions including a headache syndrome, eye infection, and cerebrovascular event were considered. Following her eye exam and diagnoses of optic neuritis the differential diagnosis included central nervous system (CNS) infections (e.g., Lyme, Neurosyphilis, HIV), CNS inflammatory diseases (e.g., systemic lupus erythematosus, Sjogren syndrome, Sarcoidosis), CNS vascular disease (e.eg. diabetes mellitus, vasculitis), CNS anatomic disease (CNS neoplasm, arteriovenous malformation, Arnold Chari malformation, medication or drug use although denied by the athlete, vitamin deficiency or toxicity, psychiatric conditions, and endocrine disorders (e.g., hypothyroidism).
Treatment
The athlete met clinical diagnostic criteria for relapsing-remitting multiple sclerosis based on the McDonald criteria (1,2): 1 attack, 2+ lesions and positive oligoclonal bands on CNS analysis. During hospital admission she was provided a 3-day course of intravenous methylprednisolone, followed by a steroid taper of prednisone 1 mg/kg/day orally for 14 days.
One week following hospital discharge she was reassessed by ophthalmology, established with a neurologist, and continued to see her team physician regularly. Given the acute onset of her condition, young age and desire to continue playing competitive basketball she agreed with beginning a disease-modifying therapy (DMT) for the prevention of future attacks. Due to the presence of JC virus (JCV) antibodies natalizumab was contraindicated, therefore, ocrelizumab which is first-line therapy for primary progressive MS. She was scheduled to receive her first dose of ocrelizumab at 20 mg subcutaneous at week 0, 1 and 2 then 20 mg per month at week 4. Potential adverse effects of ocrelizumab including liver injury, progressive multifocal leukoencephalopathy (PML) and risk of infection were discussed in depth. High dose of Vitamin D and corrective vision lenses were also provided to her.
Table 1: McDonald Criteria for Diagnosis of Multiple Sclerosis.
| McDonald Criteria for Diagnosing Multiple Sclerosis | ||
| Number of Attacks | Number of lesions | Additional data needed for diagnosis |
| ≥ 2 attacks | ≥ 2 | None |
| ≥ 2 attacks | 1 AND clear historical evidence of previous attack involving a lesion in a distinct anatomical location | None |
| ≥ 2 attacks | 1 | Dissemination in space demonstrated by additional clinical attack implicating a different CNS site or by MRI |
| 1 attack | ≥ 2 | Dissemination in time demonstrated by additional clinical attack or by MRI OR demonstration of CSF-specific oligoclonal bands |
| 1 attack | 1 | Dissemination in space demonstrated by an additional clinical attack implicating a different CNS site or by MRI AND Dissemination in time demonstrated by an additional clinical attack or by MRI OR demonstration of CSF-specific oligoclonal bands |
Adapted directly from Thompson AJ, Banwell BL, Barkhof F, et al.: Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17:162-173. 10.1016/S1474-4422(17)30470-2.
Outcome
She returned to basketball 2 weeks after being discharged from the hospital, but participation in sport and academics, as well as her initial ocrelizumab dose was suspended due to the beginning of the COVID-19 pandemic. Six weeks from her initial diagnoses during a telehealth visit with her team physician she reported continued right eye irritation. Additionally, she reported living with her mother and two teammates in a small apartment, not practicing the recommended hygiene and social distancing sanctions provided by the Center for Disease Control (CDC). She expressed interest in returning home to her foreign country given the undetermined future of academics, medical care and sports during the pandemic.
With guidance from the neurologist, the team physician proposed treatment options to assist the athlete during this personal and universally challenging time. Suggested treatment alternatives included, delaying DMT with or without oral steroids, beginning DMT with ocrelizumab followed by strict social isolation to avoid risk of infection and return to her home country one month following treatment initiation, or returning to her home country where she would begin DMT. Ultimately, she decided to begin DMT in the United States and return home after one month. She was advised to remain in isolation given her immunocompromised state to prevent infection from COVID-19 and other diseases. The athlete and her teammates were educated on how to create a safer living environment according to CDC standards and provided necessary equipment (e.g., sanitization products, masks, etc.). Her team physician contacted the athletes’ home primary care physician to create a travel and treatment plan as she prepared to return home following her initial dose of ocrelizumab.
Although the above treatment plan was selected, her parents lost their jobs due to COVID-19 and she was unable to return to her home country initially due to financial restraints. She returned to full basketball participation once COVID-19 restrictions for athletic competitions were lifted. At the end of the basketball season, she decided to leave the university to pursue a professional basketball career in her home country. Although counseled on the risk of disease progression without DMT she decided to discontinue ocrelizumab after 7 treatments. Two years from diagnosis she is playing basketball for her home country’s national team, but the status of her MS is unknown.
Discussion
MS is the most common progressive neurologic disease of young adults worldwide affecting nearly 1 million people in the United States [1,2]. The cause of this heterogenous condition is unknown but its associated clinic manifestations are attributable to inflammation, demyelination, and axon degeneration [3,4]. Multiple sclerosis has a female predominance with women often being diagnosed earlier than men [3,5,6]. There is a paucity of literature addressing elite and collegiate athletes affected by the disorder. Since the typical patient presents as a young adult with one or more clinically distinct musculoskeletal and/or neurological symptoms, clinicians caring for athletes should be familiar with the diagnosis, management and prognosis of MS as it pertains to this specific population.
Early recognition is essential to prevent injury, relapse, and future disabilities. While prompt diagnosis is often difficult due to clinical findings that mimic many other conditions. McDonald criteria aids to establish an MS diagnosis by incorporating clinical, diagnostic imaging, and laboratory evaluations but various other studies should be considered to exclude other diagnoses. How some sports related injuries (e.g., concussions, overtraining, psychosocial stressors, musculoskeletal injuries) present similarly to MS must be taken into consideration especially in the athletic population. Characteristically, MS begins with a distinct episode affecting the central nervous system. Episodes can be a result of a single lesion or more than one lesion both of which often develop acutely than steadily resolve at least partially over weeks to months. Features suggestive of MS include altered proprioception, optic neuritis, focal weakness, paraesthesia, diplopia, incoordination, vertigo, urinary incontinence, Lhermitte sign (electrical sensation down the cervical spine), cognitive changes, and Uhthoff phenomenon (heat sensitivity) [7, 8]. Optic neuritis can present with an afferent pupillary defect, nystagmus, and visual changes which may considered related to an acute sport-related concussion [9,10]. Motor neuron signs such as spasticity, hyperreflexia, sensory changes of the extremities and gait disturbances can also be assumed concussion symptomatology or other common injuries of athletes such as herniated discs, stingers/burners or functional gait changes due to acute or remote injury. Physical exhaustion from sport training, sleep impairments related to travel, nutrient deficiency due to low energy availability, and urinary incontinence are common in athletes. Outdoor sports, particularly those in hot climates can lead to intolerability to heat which is often presumed to be correlated to poor acclimation, deconditioning or dehydration.
Athletes with MS should be inspired to notify their medical team of new or worsening symptoms to prevent injury, their treatment plan, and participation in competitive sport. Athlete-centered communication, focusing on the whole person not just their diagnosis and encouraging athletes to make an informed decision about their medical care is essential. Although DMT presents a risk of adverse effects and financial burden athletes treated with DMT have the potential to reduce or stop further neurological and/or musculoskeletal impairments. Some medications for the management of MS may be prohibited by sports organizations (e.g., NCAA, WADA) therefore certain measures may be needed to allow competitive sport participation. Since athletes often receive medical care and medications through their athletic institution or governing body the medical team must consider treatment resources if their status should change. Respecting social and cultural differences is essential as athletes commonly travel to other countries to participate in competitive sports. Athletes often share living spaces which can be challenging for multiple reasons, particularly during the COVID pandemic as seen in this case. Superlative physical and mental health is required for an athlete to be successful in their sport. A condition such as MS can cause devastating career ending consequences for athletes. Although the severity in debility caused by relapse-remitting MS varies from person to person, even a slight temporary or permanent alteration in an athletes neurological or musculoskeletal system can inhibit sport performance. Injuries in athletes without a diagnosis of MS have been correlated to poor outcomes and enhanced psychosocial stress [11].
As seen in this case, a young athlete recently diagnose with MS was also faced with the challenge of a worldwide pandemic. Although there is limited evidence to suggest the use of steroids and immunosuppressants for treating and preventing progression of MS, there was even less evidence regarding COVID-19 and its effects on such treatments. Based on prior studies most medical societies suggest early administration of steroids during the replicative phase of the virus’s lifecycle may increase viral shedding [12]. Most recommendations stated that during the COVID-19 pandemic patients with independent indications for steroid use such as asthma or COPD exacerbation or vasopressor-refractory shock should not change their treatment management. Steroids are the mainstay treatment for acute MS attacks [13]. Based on our limited knowledge the benefits of steroid use in acute MS episodes seems to outweigh potential dangers associated with COVID-19. Regarding DMT, no universal consensus on use, dose or alternative treatments were available for guiding management during the pandemic. The National MS society recommends DMTs should be continued during the COVID-19 pandemic as stopping treatment may lead to worsening of disease course [14]. Additionally, those recently diagnosed with MS yet to receive DMT were advised to receive treatment as planned. There are different types of DMTs including immunomodulators and immunosuppressants which generally suppress the immune system and place individuals at greater risk for infections including COVID-19. Ocrelizumab and rituximab, two DMTs, are noted to increase the risk of having a severe COVID-19 disease course [14]. Although the risk of infection may be higher while taking a DMT, the probability of MS relapse may be of more concern. The decision to discontinue, postpone or change DMT should be based on specific risks such as disease severity, age, comorbid health conditions and environment. Given the young age and low likelihood of comorbid health conditions of collegiate athletes, the risk of infection is lower than the general MS population. Therefore, preventing further neurological/musculoskeletal impairments with the use of DMT should be strongly considered.
Social determinants of health among collegiate athletes with MS and individuals in their life propose a challenge to the athletic medical team, particularly during a global pandemic. An athlete’s environment often includes close living quarters and lively social interactions which enhance the spread of all infections including COVID-19. Athletes receiving DMT would need regular monitoring from healthcare providers but avoiding facilities with potential infected patrons would need to be a priority. As seen in this case report, the use of virtual visits allowed for continued and safe medical care and education for not only this athlete but also teammates, coaching staff, and other supporting individuals. As in all individuals, financial insecurity in collegiate athletes can limit treatment options. Although athletes receiving DMT will continue to be at risk of infections regardless of a pandemic scenario, there is limited knowledge about COVID-19 and its risks for athletes living with MS.
Learning Points
1. Early diagnosis of MS in athletes can be challenging given the similarities of presenting symptoms to common musculoskeletal conditions.
2. Treatment goals must be set that align with athletic needs, goals and protocols.
3. Handling unexpected barriers in a global pandemic.
4. Patient autonomy using patient-centered communication is essential for rapport building and quality medical care.
Conclusion
This case presents several themes that assist clinicians caring for athletes with MS. MS presents similar to other conditions therefore diagnosis in the athletic population is easily missed. Without a healthcare team familiar with the immediate and future needs of the athlete, subpar preliminary and continuous treatment may result in devastating health changes and career ending consequences in athletes. Additionally, this case presents unforeseen ethical and clinical obstacles, including the impact of COVID-19 pandemic.
Declarations
Competing interests: None.
Contributor ship: All Authors contributed equally to this case report.
Acknowledgements: None.
Funding info: None.
Ethical approval information, institution(s) and number(s): None.
Data sharing statement: None.
Patient involvement: None.
References
- (2020). Anon DMT Guidelines for Coronavirus (COVID-19) and : National Multiple Sclerosis Society .
Publisher | Google Scholor - Anon Updated McDonald Criteria Expected to Speed the Diagnosis of MS and Reduce Misdiagnosis.
Publisher | Google Scholor - Arentz, M., Yim, E., Klaff, L., et al. (2020). Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. The Journal of the American Medical Association.
Publisher | Google Scholor - Wallin, M.T., Culpepper, W.J., Campbell, J.D., et al. (2019). The prevalence of MS in the United States: A population-based estimate using health claims data. Neurology 92(10):1029-e1040.
Publisher | Google Scholor - Ramagopalan, S.V. and Sadovnick, A.D. (2011). Epidemiology of multiple sclerosis. Neurologic clinics 29(2):207-217.
Publisher | Google Scholor - Goodin, D.S. (2014). The epidemiology of multiple sclerosis: insights to disease pathogenesis. Handbook of Clinical Neurology 122:231-266.
Publisher | Google Scholor - (2020). Helen Ford. Clinical Medicine, 20(4):380-383.
Publisher | Google Scholor - Panginikkod S, Rayi A, Rocha Cabrero F, et al. (2022). Uhthoff Phenomenon. StatPearls Publishing.
Publisher | Google Scholor - National Clinical Guideline Centre (UK). (2014). Multiple Sclerosis: Management of Multiple Sclerosis in Primary and Secondary Care. London: National Institute for Health and Care Excellence (UK); 2014 Oct. (NICE Clinical Guidelines, No. 186.) 5, Diagnosing MS.
Publisher | Google Scholor - Wallace B, Lifshitz J. (2016). Traumatic brain injury and vestibulo-ocular function: current challenges and future prospects. Eye Brain,6(8):153-164.
Publisher | Google Scholor - Ivarsson, A., Johnson, U., Andersen, M.B., Tranaeus, U., Stenling, A. et al. (2017). Psychosocial Factors and Sport Injuries: Meta-analyses for Prediction and Prevention. Sports medicine (Auckland, N.Z.) 47(2):353-365.
Publisher | Google Scholor - Ontaneda D, Rae-Grant AD. (2009). Management of acute exacerbations in multiple sclerosis. Ann Indian Acad Neurol., 12(4):264-272.
Publisher | Google Scholor - National Multiple Sclerosis Society. Coronavirus Covid-19 information MS treatment-guidelines during coronavirus
Publisher | Google Scholor