Research Article
Location of Pancreas and Pancreatic Cancer
1Department of Chemistry Sri J.N.M.PG College Lucknow UP India.
2Department of Chemistry Dayanand Girls PG Kanpur UP India.
*Corresponding Author: D.K. Awasthi, Department of Chemistry, Sri J.N.M.PG College, Lucknow UP, India.
Citation: D.K. Awasthi, Dixit A. (2023). Location of Pancreas and Pancreatic cancer. Clinical and Laboratory Research, BRS Publishers. 1(1); DOI: 10.59657/clr.brs.23.004
Copyright: © 2023 D.K. Awasthi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 16, 2023 | Accepted: July 04, 2023 | Published: July 11, 2023
Abstract
Pancreatic cancer occurs when the cancer cells grow in the pancreatic tissues. The types of Pancreatic cancer are classified by the type of cells or the tissues where the cancer cell growth occurs. The following are the types of Pancreatic cancer. Adenocarcinoma cancer is a common type of Pancreatic cancer. In adenocarcinoma, cell development occurs in the gland or inner tissues that line the pancreas. Acinar cell carcinoma is the condition where cancer can develop from the cells that create pancreatic enzymes. Squamous cell carcinoma is a rare type of Pancreatic cancer. Here, cancer growth starts in squamous cells, which regulate the release of hormones.
Keywords: pancreatic; carcinoma; enzymes; hormones; squamous
Introduction
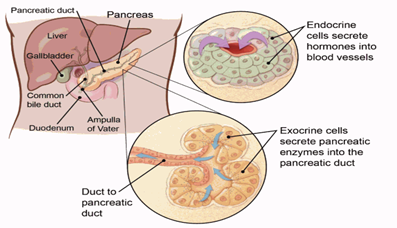
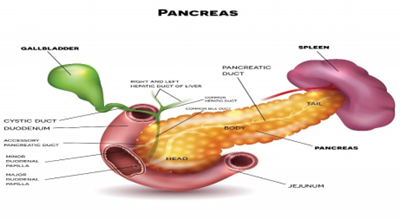
Pancreatic cancer is a type of cancer that starts in the pancreas. (Cancer starts when cells in the body begin to grow out of control). Pancreatic adenocarcinoma is the most common type of pancreatic cancer. Pancreatic neuroendocrine tumors (NETs) are a less common type. The pancreas is an organ that sits behind the stomach. It's shaped a bit like a fish with a wide head, a tapering body, and a narrow, pointed tail. In adults it's about 6 inches (15 centimeters) long but less than 2 inches (5 centimeters) wide. The head of the pancreas is on the right side of the abdomen (belly), behind where the stomach meets the duodenum (the first part of the small intestine). The body of the pancreas is behind the stomach. The tail of the pancreas is on the left side of the abdomen next to the spleen.
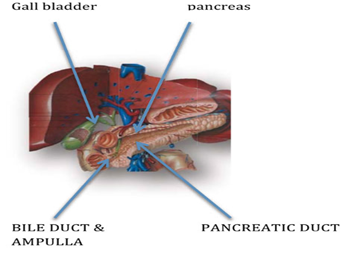
The most common type of pancreatic cancer, adenocarcinoma of the pancreas, starts when exocrine cells in the pancreas start to grow out of control. Most of the pancreas is made up of exocrine cells which form the exocrine glands and ducts. The exocrine glands make pancreatic enzymes that are released into the intestines to help you digest foods (especially fats). The enzymes are released into tiny tubes called ducts which eventually empty into the pancreatic duct. The pancreatic duct merges with the common bile duct (the duct that carries bile from the liver), and empties into the duodenum (the first part of the small intestine) at the ampulla of Voter.
Endocrine cells make up a smaller percentage of the cells in the pancreas. These cells make important hormones like insulin and glucagon (which help control blood sugar levels), and release them directly into the blood. Pancreatic neuroendocrine tumours start in the endocrine cells. The pancreas is a solid gland attached in the back of the abdominal cavity behind the stomach. The pancreas is divided into 5 parts – the head, the uncinate process, the neck, the body and the tail. The head of the gland is closely attached to the duodenum, which is the first part of the small intestine into which the stomach empties liquids and partially digested food The head of the gland is situated just to the right of the midline of the abdomen and below the right ribcage. The uncinate process is an extension of the lower part of the head of the gland, which surrounds important blood vessels. The body and tail of the pancreas lie at an angle so that the tail of the pancreas is situated beneath the extreme edge of the left rib cage. The tail of the gland is closely attached to the central part of the spleen & splenic blood vessels.
Running behind the neck and uncinate process are many important blood vessels which supply the liver, the rest of the gut organs and the kidneys, including the aorta (an artery) which takes all the blood to the lower abdomen and legs, and the inferior vena cava (a vein) which returns blood from these areas. The splenic vein runs immediately under the tail and body of the pancreas and joins with the portal vein that runs immediately under the neck of the pancreas. In short, pancreas is a centrally located and very precariously connected to or is in very close contact with most of the important structures in the abdomen. Hence diseases affecting pancreas can inadvertently involve any one or more of these structures. Hence patients with pancreatic problems may not necessarily have pancreatic complaints, but can present with unrelated complaints. Running along the length of the pancreas within its centre is the main pancreatic duct, which empties pancreatic juice into the duodenum. Also running through the middle of the head of the pancreas is the main bile duct, which also empties into the duodenum. (The main bile duct carries bile from the liver where it is made and also from the gallbladder where it is stored). In most people the pancreatic duct and bile duct join together just before they open into the duodenum through a large fleshy nipple called the ampulla of Voter (after the person who described this). Surrounding the openings of each of these ducts are small muscles that control the release of pancreatic juice and bile and thus act as valves (also called sphincters). There is also a valve that regulates the pancreatic juice and bile together and this sits in the ampulla. This common valve is called the sphincter of Oddi, also named after the man who described this. About one in ten people have two separate pancreatic ducts, one that opens as normal through the ampulla of vaster and the other through a smaller nipple (called as papilla). For this reason, the ampulla of vaster is sometimes called the major papilla and the other smaller opening is called the minor papilla. The pancreatic duct that opens through the minor papilla is called the accessory pancreatic duct (normally this joins the main pancreatic duct rather than opening separately into the duodenum). It makes enzymes, which are necessary to digest food in the intestines: Food consists of carbohydrates (e.g., glucose), proteins (e.g., meat) and fat (e.g., butter). Pancreas secretes different enzymes, which are responsible for breaking down clumps of different types of food into small particles for absorption. (Process of digestion) The main enzymes include amylase for digesting carbohydrates, trypsin for digesting proteins and lipase for digesting fats. These enzymes are collected from the small glands in the pancreas into small ducts and finally into the main pancreatic duct to be released into the duodenum. The enzymes when they are first made in the acini are not active (otherwise they would digest the pancreas as well!). When they pass into the duodenum however, they are made active by the juice of the duodenum. If there are not enough pancreatic enzymes, fat is not digested and the stools (bowel motions) become pale and greasy. These greasy stools may become difficult to flush away from the toilet and may give off a strong offensive smell. Doctors call this steatorrhea (fatty stool). The digestion of fat is very special. Fat needs to be dispersed before the pancreatic enzymes can properly break it down. This dispersion of fats is made by bile acids, which are present in bile produced by the liver and stored in the gall bladder. Bile acids act in exactly the same way as detergents, which are used to wash up greasy dishes. Therefore, both bile acids and pancreatic enzymes are needed for fat digestion. If the main bile duct becomes blocked, then the bile cannot get into the duodenum & fat cannot be properly digested. When this common opening is blocked, the bile made by the liver cannot go into the bowel it goes into the blood and out through the kidneys into the urine. This results in the eyes and skin becoming yellow and is known as jaundice. As the bile is in the urine this now becomes dark in colour. Because the flow of bile is blocked (or obstructed), doctors call this condition obstructive jaundice. As the bile duct goes through the head of the pancreas, jaundice can be caused by disease of the pancreas (such as pancreatitis or cancer). It produces insulin to enable every part of the body to use glucose (sugar). Insulin is a hormone made in special groups of cells called islets of Langerhans, which are dispersed throughout the pancreatic gland. It helps the cells of the body to use glucose as a source of energy in order to maintain their different functions. In absence of insulin, sugar instead of entering the cells of the body, stays in the blood leading to harmfully high concentrations. (Diabetes mellitus) A large proportion of the islets (pronounced ‘eyelets’) are in the tail of the gland. Most of the pancreas can be removed but there are usually enough islets remaining to make insulin sufficient to prevent sugar diabetes from occurring. As you are probably aware, diabetes can be treated by taking regular injections of insulin, which can be taken from the pancreas of animals (e.g. pork insulin) or made by genetic engineering (so called ‘human’ insulin).If pancreatic duct outflow is blocked due to any reason, gradually pancreatic duct enlarges in any size due to backpressure. Eventually the increased pressure within the duct starts taking toll on the pancreatic enzyme secretion, which drops and affects the digestion of food and absorption of nutrients, thereby affecting a person’s weight and overall health. The insulin production is not immediately affected but over a period it will also drop thereby causing sugar diabetes in the patient. Enzyme production and insulin production are independent. Because digestive enzymes and insulin are made by different parts of the pancreas, a problem with enzyme production does not mean necessarily that there will be a problem with insulin production. Similarly, if there is a problem with insulin production, this does not mean necessarily that there will be a problem with enzyme production.
Assuming that the pancreas was normal to begin with, increasing loss of the pancreas gland (by disease or surgery) usually results in more loss of enzyme production before there is obvious loss of insulin production. Another way of saying this is that the insulin ‘reserve’ is much more than the enzyme ‘reserve’ of the pancreas.
Acute Pancreatitis
Chronic Pancreatitis
Pseudo cyst of pancreas
Cancer of pancreas
Cystic tumours
Neuroendocrine tumours
Risk factors
Smoking and tobacco
Heavy alcohol consumption
obesity
Diabetes (especially type -2diabetes)
Hereditary
Chronic pancreatitis (inflammation in the pancreas caused by smoking and alcohol)
Unnoticed pancreas infection
For Pancreatic cancer, pay attention to the following symptoms
Abdominal pain
Back Pain
Weight loss
Poor appetite
Inflammation of the pancreas
Fatigue
Nausea and vomiting Fever
Indigestion
Jaundice (yellow skin and eyes)
Change in urine colour (dark or brown colour)
Blood clots
Itchy skin
Gallbladder or liver enlargement
You may be advised to have certain blood tests like complete blood count, blood urea, creatinine, liver function tests (bilirubin, liver enzymes like SGOT, SGPT, Alkaline phosphatase, gamma GT, albumin), amylase, lipase, calcium, and parathormone. In case of acute pancreatic problems, you will be advised to get admitted and all these tests will then be done in-house. Similarly, diagnosis of pancreatic problems requires radiological imaging studies of abdomen like Ultrasonography, CT scan, MRI or further interventions like gastrointestinal endoscopy, ERCP, PTHC or EUS. It quite often so happens that patient is advised these investigations in a sequential manner and not at one go. This does take time but considering the cost of these investigations it is always better to ask for the next investigation only if it is absolutely necessary. Unfortunately, in a small group of patients one cannot reach a diagnosis in spite of all this effort.
The cause of pancreatic cancer is largely not known, although in the case of ductal-type cancer (see below) there is an association with smoking tobacco. There is also an increased risk in patients with chronic pancreatitis and Hereditary Pancreatitis. Pancreatic cancer also occurs in certain familial cancer syndromes such as PeutzJeghers Syndrome, Breast and Ovarian cancer Syndromes, Familial Atypical Mole and Melanoma Syndrome and Familial Adenomatous Polyposis. Rarely there are families with Familial Pancreatic Cancer. Pancreatic tumours can be solid tumours or those containing fluid (cystic). The solid tumours are usually adenocarcinomas even though rarely they can be of other types. There is also a special type of pancreatic tumour called neuroendocrine tumour (PNET). The type of tumour decides the long-term outcome and at times even the treatment. Cystic Tumours may be benign or malignant & may be confused with pancreatic pseudo cysts (pronounced ‘Sue-doe-cyst’) that occur because of inflammation of the pancreas called pancreatitis. Hence it is important to confirm the nature of content of the cyst. The content of the cyst can be rather watery and this type of cystic tumour is called serous cyst adenoma. It is non-malignant and has very little cancer potential.
The fluid of the cyst can be filled with mucin and this type of cystic tumour can be a mucinous cyst adenoma or cyst adenocarcinoma or intraductal papillary mucinous tumour. These are cancerous or have potential to become cancerous. These are the common varieties of cystic tumours. There are some uncommon ones too. The success rate of treatment of cystic tumours is better than the results of treatment of common pancreatic cancer.NET stands for neuroendocrine tumour. Neuroendocrine cells are special types of cells commonly located in the linings of gastrointestinal tract (oesophagus to rectum), bronchus (airway) and pancreas. They are located elsewhere too. Tumour arising from these cells is called a neuroendocrine tumour or NET. The neuroendocrine cells secrete various hormones depending on their location. However not all NETs secrete tumours. Those that secrete hormones present due to the various effects of these hormones. Nets short for pancreatic neuroendocrine tumours. These tumours may arise from the endocrine cells in the islets of Langerhans in the pancreas (islet cell tumours) or so-called neuroendocrine cells either in the pancreas or ampulla of vaster (carcinoid tumours) or the duodenum (gastronomes). The success rate of treatment of these PNETs is much better than the results of treatment of other types of pancreatic cancer. Nets can secrete one of six or more different hormones causing different types of illness (or syndrome) and are called functioning neuroendocrine tumours. Also, neuroendocrine tumours may not secret any hormones and are then called non-functioning neuroendocrine tumours. Endocrine tumours can affect individuals at any age and they can even arise in small babysitters that release excess insulin are called insulinoma. These tumours are nearly always benign, meaning non-malignant and noncancerous. Tumours that release excess gastrin are called gastronome and occur in the pancreas and in the duodenum. These tumours are mostly cancerous. Other types of functioning neuroendocrine tumours are called glucagonomas, VIPoma’s, somatostatin MAs & Pumas and are usually malignant or cancerous. Nets may be inherited and the two main types of hereditary pancreatic neuroendocrine tumours are found in multiple endocrine neoplasia type 1 (MEN-1) & von Hippel-Lindau disease (VHL), but also in the rare disorders of neurofibromatosis type 1 and tuberous sclerosis. Most commonly cancers of the pancreas arise in the head of the gland. This has two effects. First, the cancer blocks the bile duct leading to jaundice, dark urine and pale stools. There is sometimes itching of the skin due to jaundice, which rapidly disappears once the blockage is cleared or bypassed. Second, the cancer blocks the pancreatic duct leading to poor digestion, loose motions and weight loss. This can be relieved by clearing the blockage or by giving pancreatic enzyme tablets. Rarely it causes acute pancreatitis. Diabetes may already be present in a number of patients prior to developing the cancer or become apparent soon after it is diagnosed or following surgery. Similarly, blockage of the pancreatic duct can cause pain. Pain can be due to infiltration of nerves surrounding pancreas too. The commonest type of pancreatic cancer is that arising from the small ducts of the pancreas (ductal-type adenocarcinoma). Most often it arises in the head of the gland and a principal feature is the development of obstructive jaundice. This type of cancer often occurs in individuals aged 60 years or older but it can affect younger people as well. Typical early symptoms are jaundice, dark urine, pale stools, itching, feeling of sickness (nausea), weight loss & unexpected development of diabetes.
Tumours in the body and tail of pancreas are more difficult to pick up early because they do not cause obstructive jaundice earlier on. Therefore, they remain undiagnosed for long time & spread by the time are diagnosed.
Typical symptoms for body and tail of pancreas tumours are vague abdominal pain, dyspepsia, stomach ulcer-like pain, intermittent diarrhoea, feeling of sickness (nausea), weight loss, unexpected development of diabetes, back pain that does not go away & unexplained blood clots (venous thrombosis). Tumours of the Ampulla of vaster, Intrapancreatic Bile Duct Cancer (bile duct as it travels through the pancreas) & Duodenal Cancer can also cause similar complaints as the cancer of head of pancreas. Tumours from the ampulla & duodenum may cause bleeding& present as bloody vomiting or blood in stools (black stools) or only anaemia. It is important to know that these cancers have better long-term outcome than pancreatic cancer.
Cystic tumours are relatively uncommon and are more frequent in females. They present with abdominal pain, back pain, vomiting, nausea, weight loss, an attack of acute pancreatitis & rarely gastrointestinal bleeding. If the cyst presses on the bile duct, then this will cause obstructive jaundice. However, it is often picked up while investigating the abdomen for relatively minor or unrelated complaints or during a routine health check-up. A patient with symptoms & signs of a pancreatic tumour may be 1st seen by family physician, internist, and general surgeon or directly by gastroenterologist. Specialist pancreatic surgeon is usually the last ring in the chain unfortunately and hence patients quite often come with a stent in the biliary system, which could be avoided.
Apart from a routine complete blood count investigations like liver function tests & abdominal USG are asked for as a rule. Once USG confirms suspicion then rest of the investigations like CT scan or MRI scan of abdomen and often a EUS are asked.
Remember that an abdominal US scan is likely to miss an early pancreas cancer. Therefore, if clinical picture & LFTs are in favour of pancreatic cancer (e.g., obstructive jaundice) patient will be sent for a pancreas specific CT scan which is fast & accurate. An MRI of abdomen is also equally useful & can be done. Sometimes both are necessary when the tumour is cystic & nature of tumour (? cancer) is uncertain. A EUS is most useful in doubtful cases and a EUS guided biopsy or aspiration of cyst fluid for analysis will be done whenever possible.
There are not many blood tests to diagnose any form of pancreatic cancer. Levels of a tumour marker CA 19.9 in the blood are measured and if they are significantly high, it raises a strong suspicion of biliary or pancreatic cancer. However, it can rise even with noncancerous obstruction of bile duct. In case of cystic tumour, estimation of levels of Carcinoembryonic Antigen or CEA & mucin in the cyst fluid aspirated during an EUS is useful to diagnose mucinous tumours. Whenever a PNET is suspected on clinical picture & imaging studies, certain special tests will be asked. These include serum levels of gastrin, insulin, proinsulin, c-peptide levels and sometimes tests for uncommon tumours; nuclear scan called octreoscan or SRS (somatostatin receptor scintigraphy) scan, EUS guided aspiration cytology or biopsy. Rarely invasive tests are required to reach a diagnosis. Patients with pancreatic neuroendocrine tumours need to undergo some special tests that may be extra to those already describe above.
Hormone Profile
In order to find out whether your tumour is secreting hormones and which hormones are involved you will need to give several blood samples. You may also need to give a sample of urine or urine collected for a complete 24-hour period. If doctors are worried that you have an insulinoma you may need to be fasted for up to 72 hours. The endocrine team will help to advice and co-ordinate the collection of samples. The samples are sent to special labs (or laboratories). Because the tests are difficult to perform, the results may take several weeks to be completed. And unfortunately, sometimes they have to be repeated.
Octreotide Scan
Most pancreatic neuroendocrine tumours have what are called type-2 receptors (doctors say somatostatin type-2 receptors) on the outer surface of each cell of the tumour. By attaching a radioactive chemical to a particle that attaches to the receptor it is possible to see where the tumour is. This test is performed in the Nuclear Medicine Department and you are asked to lie on a special couch under a special camera called a gamma camera. It involves giving a small harmless intravenous injection of the radioactive chemical. Where and how many tumours there are can now be seen by the gamma camera.
MIBG Scan
Because not all pancreatic neuroendocrine tumours (NET) can be seen by the octreotide scan we use another type of scan. MIBG is a special chemical that is taken up by the pancreatic NET cells and is concentrated inside the tumour cells. By attaching a radioactive chemical to the MIBG it is possible to see where the tumour is. This test is also performed in the Nuclear Medicine Department. Again, you are asked to lie on a special couch under a special camera called a gamma camera. It involves giving a small harmless intravenous injection of the radioactive MIBG. Where and how many tumours there are can now be seen by the gamma camera.
Selective Arteriography
Despite all the many tests already performed to locate where a pancreatic neuroendocrine tumor is, further tests may still be required. It might be possible to find the tumor because it has a special blood supply. Selective arteriography is performed in the X-ray department. You will be placed on an X-ray table, the skin cleansed with antiseptic and covered with sterile gowns. Under local anesthetic a tube will be inserted into the artery in either the left or right groin (called an arterial catheter). ‘Dye’ (or contrast) is then injected into the catheter to see where it goes using an X-ray television screen. The catheter can be guided to the different small arteries that supply the pancreas. More ‘dye’ (or contrast) is then injected into each artery and using X-rays the tumor blood supply can be seen on a television screen and pictures are then taken.
Selective Venous Sampling
If selective arteriography has not been successful then this sampling technique can be used either in the same or separate sitting. Blood samples are taken from different positions in the veins that drain away from the pancreas. The procedure is also performed in the X-ray department. You will be placed on an X-ray table, the skin cleansed with antiseptic and covered with sterile gowns. Usually using local anesthetic, a wire is pushed through the skin and into one of the branches of the hepatic portal vein within the liver. A tube (or catheter) is pushed over the guidewire and the guidewire is removed. The tube is then advanced into the different veins that drain the pancreas and small samples of blood are then taken. The blood samples are then sent for special tests to see if there are any hormones and what the concentration is. Usually there is one area with a very high concentration. This tells the surgeon where about in the pancreas the tumor will be at operation.
The best treatment for pancreatic cancers of above-mentioned types and peripancreatic cancers (ampulla, lower bile duct & duodenum) is surgery to remove the cancer (resection) by a specialist pancreatic surgeon. However, this is possible only when the cancer is not spread to other tissues like liver, lungs, and bone etcetera. Similarly, the tumor should be free from surrounding important blood vessels. If this local involvement of vessels is limited to portal vein, a portion of this vein can be removed and reconstructed with a graft. The patient can have a good life after this. But it is not true if the artery supplying the intestines is involved. The process involving assessment of surrounding & distant organ involvement is called staging of tumor. Not all patients are lucky enough to undergo a surgery for various reasons and these patients undergo various palliative therapies. (Treatments that palliate or reduce complaints but don’t cure the patient).
In all patients it is important to determine whether an operation is feasible (‘staging’). This requires the use of a special CT scan. The specialist may request this investigation even if this has already been performed by the referring hospital. Another ‘staging’ procedure is to perform laparoscopy and/or laparoscopic ultrasound. This is a short operation under general anesthetic. Using ‘key hole’ surgery a telescope is inserted into the abdomen to examine the organs. A special ultrasound ‘probe’ may be used to look at deeper tissues. Some centers may also use a PET scan.
Operations On Pancreatic Neuroendocrine Tumors
The operations performed on PNETs are very similar to those performed on pancreatic cancers in general the choice of operation depends on the number and position of the tumors. In the case of insulinoma, usually only a very small procedure needs to be done on the pancreas. This simply involves removing the tumor only but not removing any of the pancreas. This operation is called enucleation. This is still classed, as a major operation however as a big abdominal incision is still needed and major surgery is needed to find the pancreas. Also, you will still need to be monitored closely after surgery to check on the blood sugar levels.
Debulking Of Tumor
This implies partial removal of the tumor to whatever extent possible with safety. This is never done for the common ductal type of pancreatic cancer. It is done in selected cases of cystic tumors and on many occasions for PNET. Patient should discuss the possibility in an individual case with his treating physician. Debulking reduces tumor volume allowing resolution of some complaints and also allows other form of therapies like chemotherapy or TACE or DOTATATE & DOTATOC work more effectively.
Biliary Bypass
This operation is performed for obstructive jaundice. Obstruction of the bile duct in pancreatic cancer is common. This happens because the cancer in the head of the pancreas can press on the bile duct and cause it to become partly blocked. This causes obstructive jaundice (see above). The narrowing (or stricture) is ‘bypassed’ using a special small bowel channel. This operation is called hepato-jejunostomy or choledochal-jejunostomy. Choledochal’ is two words (from Greek and Latin) meaning bile (chole) and duct (dacha), whilst ‘hepatic’ refers to the bile duct as it leaves the liver. This operation will be done either as a planned operation (rare with availability of stent) or sometimes as a last-minute decision when patient has been taken up for surgery and found inoperable on opening the abdomen (common).
Gastric Bypass
This procedure is undertaken if there is vomiting due to obstruction of the stomach or duodenum by a tumor. Obstruction of the duodenum is quite common. This happens because a cancer in the head of the pancreas can press or invade the duodenum and cause it to become partly blocked. This causes a feeling of sickness (nausea) and vomiting after food. This will obviously contribute to weight loss. The narrowing (or stricture) is ‘bypassed’ connecting the small bowel to the stomach. This operation is called a gastro-jejunostomy or gastric-bypass. In fact, this may be done during the same time as biliary bypass to avoid the problems of duodenal obstruction at a later date.
Biliary Stenting
Older patients may not be suitable for surgery. The jaundice can still be relieved by inserting a tube (stent) through the tumor during ERCP. If it is not possible to do this by ERCP, then an alternative is by PTHC or a combination of ERCP and PTHC and is called a combined procedure or rendezvous procedure. A metallic stent, which is a permanent fixture, is inserted. It is better than a plastic stent as it doesn’t get blocked easily. But it is expensive. Stenting should be done only if patient is having symptoms due to jaundice like severe itching. Stenting is not without complications because stent can get blocked and can cause infection and severe sepsis. At times a repeat stenting will be required.
Endoscopic Duodenal Stenting
Obstruction to the duodenum usually needs surgery. An alternative in older or unfit patients is to insert a tube through the duodenum. In the X-ray department a flexible telescope or endoscope is passed into the mouth. This is then eased down the gullet and into the stomach and then into the duodenum. A small guidewire is then pushed through the tiniest gap left by the tumor. The special tube or stent is then pushed over the guidewire. This stent is metallic and expands on its own in next 48 hours. You lie on an X-ray table to enable pictures of the procedure to be taken as it is being performed. It is essential that you do not eat or drink anything for at least 8 hours before the procedure is performed. Usually, a plastic tube is put into a vein of the right forearm or the back of the hand before you go to the X-ray department. You may need a drip of intravenous fluids. You will be asked to sign a consent form agreeing to this procedure because it is complicated.
Normally you are taken on a trolley to the X-ray department and, after being checked by a nurse, asked to move onto the X-ray table. You will be asked to lie on your left side with your left arm behind your back and be given a throat spray of local anesthetic. These tastes awful but the feeling quickly goes and it will stop any coughing during the procedure. A strong sedative is now given by injection. This is enough to make most patients very sleepy but not fully unconscious. It is very important that you are as relaxed as possible before and during the procedure. The telescope is easily passed into the mouth and stomach. There is then a strange sensation as air is introduced into the stomach. Belching should be avoided as the air helps the endoscopist to pass the tip of the telescope into the duodenum. Most patients usually do not remember anything of the procedure. The special tube or stent is permanent and is a metal mesh. This gradually expands over a few days after it has been inserted, so the relief from nausea may not be immediate.
Chemotherapy
This is also advised for patients with a cancer that cannot be removed as this makes you feel better (doctors say ‘improves symptoms’) as well as increasing the length of time that you have to live. Because doctors have still to work out the best type of chemotherapy there are many clinical trials that compare the best available treatment with a new treatment. We have a trial because we do not know if the new treatment is actually better. Patients usually benefit by being in a trial so patients are recommended to consider joining an approved trial. Else one opts for a reasonably proven & efficacious protocol.
All mucin containing tumors (because of their cancerous potential), tumors with evidence of cancer, all rapidly enlarging cystic (serous or otherwise) tumors, all tumors causing complaints, all cystic PNETS and tumors whose nature cannot be confirmed; all of them should ideally be subjected to surgical treatment and excision. However small sized serous cystic tumors do not need surgery if confirmed beyond doubt and are only observed by routine imaging like CT scan. If they grow in size or cause complaints only then a surgery is performed. However, some patients are not fit for surgery because of age, spread or medical illnesses and they are treated only for their prominent symptoms like pain (medicines), jaundice (stent), vomiting (medicines or stent or surgery if there is obstruction of stomach or intestine).
The symptoms of some patients with certain types of pancreatic neuroendocrine tumor are because their tumors are secreting a hormone or it’s a functioning tumor. An insulin secreting tumor reduces blood sugar and can cause repeated giddiness or fainting episodes, gastrin secreting tumor causes hyperacidity leading to gastric ulcers, others can cause watery diarrhea weakness, so on and so forth. These complaints can be greatly relieved by special drugs (such as octreotide) by blocking the secretion of the hormone from the tumor. However, this does not stop the growth or spread of the tumor. Similarly, the effect is limited if tumor load is very high. The exception is insulinoma, which should always be treated by surgical removal.
Some patients will also benefit from chemotherapy and also from a special drug called interferon–alpha (mainly for patients with carcinoid tumors). Special radiotherapy treatment may be given using chemicals that are tagged with radioactive agents (DOTATOC & DOTATATE). These selectively go to the tumor, and destroy it. This is conditional on the tumor being positive for the octreotide scan. There are other treatments also available if the tumor has spread to the liver such as chemoembolization (TACE) or radiofrequency ablation (RFA). These are quite new treatments and your doctor will give you more specific information about these if they apply to you.
It is important to know that PNETS have a better outcome compared to other pancreatic cancers because they are slow growing, spread is late & multiple treatment options are there even when tumor has spread. There may be severe pain from pancreatic cancer if the cancer cannot be removed. You will be seen by a specialist pain team, which will help to find the best combination of medication for you. This frequently involves the use of morphine tablets of one kind or another. These kinds of tablet cause two particular problems. One is a feeling of sickness (called nausea), so you will need to take anti-sickness tablets. The other problem is constipation so you will need to take some form of stool loosening medicine or laxatives. Sometimes medicated skin patches are given which deliver the drug through skin avoiding certain side effects. Most patients manage very well on this type of medication but sometimes it is necessary to resort to special pain killing measures. This involves paralyzing or cutting the pain nerves that go between the brain (where the pain is felt) and the pancreas.
Coeliac Plexus Nerve Block
The nerves from the pancreas collect just behind the pancreas in a thick bundle called the coeliac plexus (coeliac is pronounced ‘see-lee-ack’). These nerves can be injected using a long needle and local anesthetic in the X-ray department or using a needle with the endoscope during EUS. If a local anesthetic is used this may reduce the pain, but usually this only lasts for a few weeks. It is also possible to block the nerves permanently using special chemicals (called sclerosants) such as concentrated alcohol.
Bilateral Thoracoscopic Sympathectomy (Bits)
The BITS procedure involves cutting the pain nerves from the pancreas as they travel through the chest towards the spinal cord in the spinal canal. The operation is done using fine instruments and telescopes using general anesthetic and is surprisingly simple and safe to perform. This is so called ‘keyhole’ surgery. Inherited pancreas cancer happens because there is an altered gene that predisposes to cancer and is passed on from one generation to the other. Each person has exactly the same number of genes as every other person. The total number of genes is 30,000. Genes are in the nucleus of each cell of the body. Genes are like the blueprints in a factory. These blueprints (or genes) enable the cell to make proteins which then organize the two other types of basic molecule (carbohydrates and fats) to create particular types of cells and hence the different organs (such as liver, arms and legs and so on).
In the cells of different organs only some of the 30,000 genes in the nucleus are selected for use. This number varies from 6,000 to 10,000 genes in any particular cell. The different combination of genes used as blueprints for making proteins is how the human body can be organized in such a complicated way (compared to a simple worm that has only 900genes). Genes are always in pairs, so that one set comes from the mother and one set comes from the father. There are tiny variations in each gene. These tiny variations are essential to make every person an individual. Occasionally a tiny variation in a gene can give rise to a disease condition. An alteration in a gene that gives rise to a disease is often referred to as a mutation (this is a Latin word that simply means ‘changed’). Patients and their families with inherited pancreatitis require the care of a specialist surgeon, pediatrician or gastroenterologist and genetic counselling.
The main genes involved in all of the major familial cancer syndromes are known. The names of the genes sound quite strange so we only tend to use the short version name of each gene. The gene for Peutz-Jeghers Syndrome is the STK11 gene, the genes for Breast and Ovarian Cancer Syndromes are BRCA1 and BRCA2, the gene for Familial Atypical Mole and Melanoma Syndrome is the p16 gene and the gene for Familial Adenomatous Polyposis is the APC gene. The main gene for Hereditary Pancreatitis is the PRSS1 gene. The main gene for Familial Pancreatic Cancer is not known, although 10- 20% of families have a BRCA2 gene mutation. The gene for multiple endocrine neoplasia type 1 is the MEN-1 gene. The gene for von Houppelande disease is the VHL gene. The gene for neurofibromatosis type 1 is NF-1. The genes for tuberous sclerosis are the TSC-1 and TSC-2 genes.
Multiple Endocrine Neoplasia Type1 (Men-1)
This is an autosomal dominant familial cancer syndrome (passed on by the mother or the father) with tumors in small glands in the neck (called parathyroid), a small gland attached to the brain (called the anterior pituitary) as well as the pancreas. The neuroendocrine tumors in the pancreas are usually multiple.
Von Hippel-Lindau (VHL)
Von Hippel-Lindau disease is another type of rare autosomal dominant familial cancer syndrome (passed on by the mother or the father). This condition causes a multiplication of small blood vessels in the brain, spinal cord and back of the eyes and also cancers of the kidney and the small gland next to the kidney called the adrenal gland. About two thirds of patients with VHL also have a problem with the pancreas, but this is usually in the form of simple harmless cysts. About one in ten people with VHL however will also have one or more pancreatic neuroendocrine tumors (these are usually non-functioning). These families should undergo general screening for cancer as above. A proportion of families with Familial Pancreatic Cancer will have a mutation of the BRAC2 gene. Individuals from these families must be referred for genetic counselling and BRCA2 gene testing.
Screening In Patients with Men-1
Surveillance of carriers of the MEN-1 gene should begin in early childhood with blood tests every year and imaging every 3 years. Consensus guidelines have recommended screening from the age of 5 years for anterior pituitary tumors with blood tests (called prolactin and Insulin like growth factor-1) and MRI and for insulinoma also MRI along with blood tests (called fasting glucose and insulin). Screening for parathyroid tumors should begin from the age of 8 years with blood tests (Called calcium and parathyroid hormone) and for chest and abdominal tumors from the age of 20 years by CT. Other neuroendocrine tumors should also be screened from the age of 20 years using other blood tests (called chromogranin A, glucagon and proinsulin) and MRI, CT or octreotide scan. There should also be endoscopy for gastric tumors (carcinoids) and EUS for duodenal and pancreatic tumors.
Screening In Patients With VHL
Surveillance of carriers of the VHL gene should begin at the age of 10yrs initially with abdominal ultrasound repeated annually looking to find tumors in the kidneys, adrenal glands and pancreas gland as well as the pelvis. From the age of 20yrs there should be 1-2 yearly abdominal CT or MRI scans. For the pancreas again EUS examinations are to be preferred. Pancreatic cancer does not leave any symptoms in the early stages. The symptoms follow when it develops into further stages. However, body changes and other symptoms can indicate the concern for medical treatment. Pancreatic cancer stages involve four stages; the stages are characterized to help in diagnosis and treatment and to indicate the growth of cancer cells or how far it has spread.
Stage 1: The cells get located in the pancreas and start their growth.
Stage 2: The cancer cells either spread or affect the nearby organs and tissues, causing health complications.
Stage 3: The cancer cells affect the surrounding blood cells and lymph nodes.
Stage 4: Cancer spreads to other organs like the liver or abdominal cavity.
Treatments for Pancreatic cancer
Age, current health condition, severity and health complication are the factors that determine the treatment.
The treatment option includes the following:
- Surgical treatment involves the removal of the cancerous portion of the pancreas. During the removal, the surrounding affected lymph nodes are also removed to avoid recurring cancer.
- Distal pancreatectomy is the surgery process where the cancer-affected part of the pancreas is removed. In a total pancreatectomy, the whole pancreas is removed. Surgery to remove the pancreas is rare.
- Without the pancreas, the body finds it difficult to maintain blood sugar levels; in such cases, medication can help to regulate it.
- Whipple procedure where the surgeon removes the head of the pancreas along with the affected lymph nodes, duodenum and other tissues if the cancer cells are developed in the head of the pancreas.
- Radiation therapy destroys cancer cells through radiation like x-rays. Radiation therapy helps to kill, reduce and remove cancer Chemotherapy method uses anti-cancer drugs to kill cancer cells. The processes involve the intake of anti-cancer drugs to kill cancer cells or to stop them from spreading.
Conclusion
You may be advised to have certain blood tests like complete blood count, blood urea, creatinine, liver function tests (bilirubin, liver enzymes like SGOT, SGPT, Alkaline phosphatase, gamma GT, albumin), amylase, lipase, calcium, and parathormone. In case of acute pancreatic problems, you will be advised to get admitted and all these tests will then be done in-house.
References
- Rockville, MD. (2001). U.S. Preventive Services Task Force. Final Recommendation Statement: Pancreatic Cancer: Screening.
Publisher | Google Scholor - American Cancer Society. (2016). What is pancreatic cancer? American Cancer Society.
Publisher | Google Scholor - National Cancer Institute. (2018) Common Cancer Types. National Cancer Institute.
Publisher | Google Scholor - American Cancer Society. (2018). Cancer Facts & Figures 2018. Atlanta, GA: American Cancer Society.
Publisher | Google Scholor - Zhou J, Enewold L, Stojadinovic A, et al. (2010). Incidence rates of exocrine and endocrine pancreatic cancers in the United States. Cancer Causes Control, 21(6):853-861.
Publisher | Google Scholor - Howlader N, Noone A, Krapcho M, et al. (2017). SEER Cancer Statistics Review, 1975–2014. Bethesda, MD: National Cancer Institute.
Publisher | Google Scholor - National Cancer Institute. (2018). SEER Stat Fact Sheets: Pancreas Cancer. National Institutes of Health.
Publisher | Google Scholor - Rahib L, Smith BD, Aizenberg R, et al. (2014). Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res., 74(11):2913-2921.
Publisher | Google Scholor - Al Qadhi H, Al Wahibi K. (2015). Intraductal Papillary Mucinous Neoplasm of Pancreas. N Am J Med Sci. 7(5):160-175.
Publisher | Google Scholor - Nakamura M, Miyasaka Y, Sadakari Y, et al. (2017). Comparison of guidelines for intraductal papillary mucinous neoplasm: What is the next step beyond the current guidelines? Annals of Gastroenterological Surgery, 1(2):90-98.
Publisher | Google Scholor - Vege SS, Ziring B, Jain R, et al. (2015). American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology, 148(4):819-822; quize12-23.
Publisher | Google Scholor - Pergolini I, Sahora K, Ferrone CR, et al. (2017) Long-term Risk of Pancreatic Malignancy in Patients with Branch Duct Intraductal Papillary Mucinous Neoplasm in a Referral Centre. Gastroenterology, 21:21.
Publisher | Google Scholor - Sohn TA, Yeo CJ, Cameron JL, et al. (2004). Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg., 239(6):788-797.
Publisher | Google Scholor - Girometti R, Pravisani R, Intini SG, et al. (2016). Evolution of incidental branch-duct intraductal papillary mucinous neoplasms of the pancreas: A study with magnetic resonance imaging cholangiopancreatography. World J Gastroenterol, 22(43):9562-9570.
Publisher | Google Scholor - Olson SH, Xu Y, Herzog K, et al. (2016). Weight Loss, Diabetes, Fatigue, and Depression Preceding Pancreatic Cancer. Pancreas. 45(7):986-891.
Publisher | Google Scholor - Keane MG, Horsfall L, Rait G, et al. (2014). A case-control study comparing the incidence of early symptoms in pancreatic and biliary tract cancer. BMJ Open, 4(11):e005720.
Publisher | Google Scholor - Ansary-Moghaddam A, Huxley R, Barzi F, et al. (2006). The effect of modifiable risk factors on pancreatic cancer mortality in populations of the Asia-Pacific region. Cancer Epidemiol Biomarkers Prev.,15(12):2435-2440.
Publisher | Google Scholor - Ducreux M, Cuhna AS, Caramella C, et al. (2015). Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol., 26(5):56-68.
Publisher | Google Scholor - Cancer Research UK. (2016). Pancreatic cancer screening. Cancer Research UK.
Publisher | Google Scholor - Yamaguchi K, Okusaka T, Shimizu K, et al. (201). EBM-based Clinical Guidelines for Pancreatic Cancer issued by the Japan Pancreas Society: a synopsis. Jpn J Clin Oncol. 44(10):883-888.
Publisher | Google Scholor - (2018). American Joint Committee on Cancer. Pancreas Cancer Staging, 7th edition. American Joint Committee on Cancer.
Publisher | Google Scholor