Case Report
IVC Injury at Its Origin
Surgical Health Collective, Phoenix Boulevard Suite, Atlanta, Georgia.
*Corresponding Author: Mark L. Walker, Surgical Health Collective, Phoenix Boulevard Suite, Atlanta, Georgia.
Citation: Mark L Walker. (2022). IVC Injury at Its Origin. Journal of Surgical Case Reports and Reviews, BRS Publishers. 1(1); DOI: 10.59657/2993-1126.brs.22.001
Copyright: © 2022 Mark L. Walker, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: October 14, 2022 | Accepted: November 04, 2022 | Published: November 12, 2022
Abstract
A case report of infra-renal inferior vena caval injury at its origin is presented. The operative approach is outlined and the principles of trauma resuscitation reviewed. The patient had a good outcome because of adherence to Advanced Trauma Life Support principles in conjunction with team input and care.
Keywords: IVC Injury; origin; trauma; wound; hematoma
Introduction
Case Report
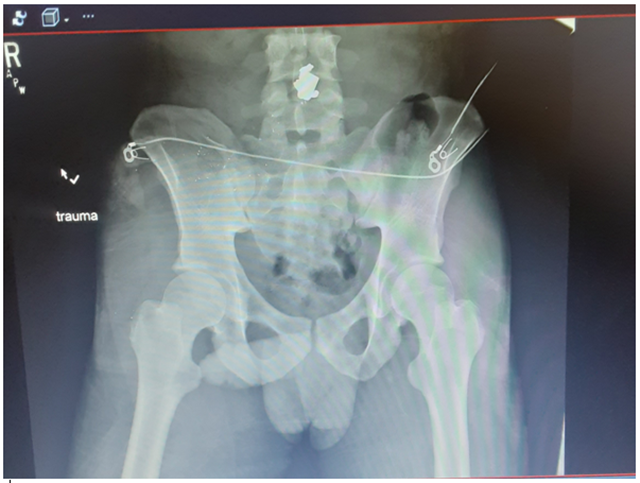
A 22-year-old man presented to a Level 1 trauma center after sustaining an isolated gunshot wound to the right flank above the iliac crest without an exit wound. On admission he was alert and oriented.His blood pressure was 80/63, pulse 80, respiratory rate 17 and temperature 97.9 degrees. The Glasgow Coma Scale was 15.The initial FAST was negative.His abdomen was soft, non-distended and somewhat tender in the right lower quadrant. A plain film of the chest was within normal limits and a pelvic film revealed a bullet at the level of the L4 vertebrae (Figure 1). 2 units of PRBC’s were administered in the trauma bay.The initial serum lactate was 4.4 and the base deficit on the arterial blood gas was 6. The initial hemoglobin was 13 gms/dl.The patient was taken to the operating room where abdominal exploration ensued. A large right retroperitoneal hematoma was evident.Proximal control of the infra-renal aorta with a vessel loop was performed. The right colon was mobilized by taking down the peritoneal reflection and the retroperitoneal hematoma was evacuated.The infra-renal IVC was controlled with a vessel loop. The bullet was located at the origin of the inferior vena cava at the junction of the right and left common iliac veins and was visible after the exposure. Sponge sticks were used to control the right and left common iliac veins. The bullet was removed and the cava was repaired with a running 3-0 prolene suture. Once this was done blood loss slowed but there was still some bleeding from the right side of the cava. Several interrupted sutures of 3-0 prolene were used to control the bleeding from the right lateral wall of the cava above the bifurcation. There was no evidence of bowel injury on exploration. The estimated blood loss was 3600 ccs. The patient received 10 units of packed cells, 8 units of FFP, 2 cryoprecipitate packs and 2 platelets during the procedure.The procedure was concluded.The patient was monitored in the ICU for 72 hours and then transferred to floor. Enoxaparin was used for deep vein thrombosis prophylaxis. Sequential compression devices to both lower extremities were also utilized. A CT scan was performed in the post-operative period because of ileus. It suggested right common iliac vein occlusion (Figure2).This was confirmed on a post-op venogram.The patient continued to progress well and was discharged to home on his 9th hospital day. He was seen in the office one week after discharge with decreased swelling of his right lower extremity and a benign abdominal exam. The midline incision was healing well.
Figure 1
Figure 2
This patient’s care reflects many of the basic principles of the Advanced Trauma Life Support [1]. He sustained an isolated gunshot wound without an exit and was hypotensive on arrival. The airway was assessed and the patient was talking without evidence of stridor. The chest was clear on exam and clearly the cause for hypotension was likely intra-abdominal hemorrhage. The focused abdominal ultrasound for trauma was negative but there was no need for CT in this setting because in the face of hypotension he was not a candidate for non-operative care [2,3,4,5]. The FAST exam excluded cardiac tamponade and the normal CXR excluded on-going bleeding in the thoracic cavity. The bullet was lodged at the origin of the inferior vena cava with on-going hemorrhage. Proximal and distal control utilizing sponge sticks is an effective technique in stemming on-going hemorrhage from the cava. Looping the cava and the common iliacs is another approach to achieve proximal and distal control. We utilized a hybrid approach looping the infra-renal cava and then using sponge sticks to control the common iliacs. Proximal control of the infra-renal aorta was obtained just in case aortic occlusion was needed. Once the bleeding is controlled venous repair is preferred [6]. The inferior vena cava below the renal veins can be ligated but this may be associated with bilateral lower extremity swelling [7]. In general, the suprarenal cava should be repaired. Retro-hepatic caval and or hepatic venous injuries in the setting of blunt trauma can be packed and this approach has been successful on occasion [8]. Endovascular venous stenting with appropriate side holes for hepatic venous drainage is a new approach being explored as well [9].
Resuscitative balloon occlusion of the aorta has been used in patients with caval gunshot wounds to reverse hypotension and there are emerging case reports suggesting that balloon occlusion of the inferior vena cava can be used in concert with Reboa to facilitate caval repair [10]. Massive transfusion protocols (MTP) are necessary in most of these cases as blood loss can be rapid. Assessment of Blood Consumption score (consisting of 4 parameters; penetrating trauma, systolic pressure of 90 or below, pulse greater than120 and a positive FAST) can provide an important prompt to order MTP [11]. In the case above, the presence of hypotension and the presence of a penetrating injury yielded a score of 2 meeting the MTP threshold. Approximating whole blood administration is the goal. This has been termed hemostatic resuscitation or damage control resuscitation. A packed red cell, fresh frozen plasma, platelet ratio of 1:1:1 is recommended. Minimizing crystalloid administration is essential. Civilian trauma centers are beginning to use more whole blood in resuscitation. The civilian results mirror the military experience with whole blood [12,13]. Damage control resuscitation is associated with more normal physiology when the patient arrives in the intensive care unit after the surgical intervention [14,15]. Deep vein thrombosis prophylaxis is essential and both mechanical and chemical prophylaxis is recommended. Although these are difficult cases, adherence to a well-organized plan of care associated with critical support from anesthesia and the operating room staff can achieve good outcomes.
References
- Stewart RM, Rotondo MF, Henry SM, et. al. (2018). ATLS - 10th Edition -Advanced Trauma Life Support Course Manual – Library of Congress Control.
Publisher | Google Scholor - Inaba K, Branco BC, Moe D, Barmparas G et.al (2012). Prospective evaluation of selective nonoperative management of torso gunshot wounds: When is it safe to discharge? Journal of Trauma, 72(4):884-891.
Publisher | Google Scholor - Peponis T, Kasotakis G, Yu J, Alouidor R et. al. (2017). Selective Nonoperative Management of Abdominal Gunshot Wounds from Heresy to Adoption: A Multicenter Study of the Research Consortium of New England Centers for Trauma JACS, 224(6):1036-1045.
Publisher | Google Scholor - Schellenberg M, Benjamin E, Piccinini A, Inaba K, Demetriades D. Gunshot wounds to the liver: No longer a mandatory operation. Journal of Trauma Acute Care Surgery, 87(2):350-355.
Publisher | Google Scholor - Fikry K, Velmahos GC, Bramos A et.al (2011). Successful Selective Nonoperative Management of Abdominal Gunshot Wounds Despite Low Penetrating Trauma Volumes Archives Surgery, 146(5):528-533
Publisher | Google Scholor - Matsumoto S, JungK, Smith A, Coimbra R. (2019). Management of IVC Injury: Repair or Ligation? A Propensity Score Matching Analysis Using the National Trauma Data Bank. J Am Coll Surg, 226(5): 752-759.
Publisher | Google Scholor - Timberlake GA, O’Connell RC, Keirstein MD. (1986). Venous Injury to Repair or Ligate, the dilemma. Journal Vascular Surgery, 4(6):553-558.
Publisher | Google Scholor - Zargaran D, Argara A, Khan M. (2020). Systematic Review of the Management of Retro-Hepatic Inferior Vena Cava Injuries Open Access Emergency Medicine, 12:163.
Publisher | Google Scholor - Giannakoupouls TG, Avgerinos ED (2017). Management of Peripheral and Truncal Venous Injuries Frontiers in Surgery, 4:46.
Publisher | Google Scholor - Howell EC, Kulkarni S, Walker PF, et.al. Endovascular Balloon Occlusion of the Inferior Vena Cava in Trauma: A Single-Center Case Series. Journal of the Americal College of Surgeons.
Publisher | Google Scholor - Cotton BA, Dossett LA, Haut ER, et.al (2010). Multicenter validation of a simplified score to predict massive transfusion in trauma. J Trauma and Critical Care, 69(1):S22-S29.
Publisher | Google Scholor - Hann K, Bible L, Chehab M et.al (2020). Nationwide Analysis of Whole Blood in Civilian Trauma Journal of Trauma and Acute Care Surgery, 89(2):329-334.
Publisher | Google Scholor - Spinella PC (2008). Warm Fresh Whole Blood Transfusion for Severe Hemorrhage. U.S. Military and potential civilian application. Critical Care Medicine, S340-S345.
Publisher | Google Scholor - Cotton BA, Reddy N, Hatch QM et.al (2011). Damage Control Resuscitation is Associated with a reduction in Resuscitation volumes and improvement in Survival in 390 Damage Control Laparotomy Patients Annals of Surgery, 254(4):598-605.
Publisher | Google Scholor - Duschesne JC, Kimonis K, Marr AB, Rennie KV et.al (2010). Damage Control Resuscitation in Combination with Damage Control Laparotomy: A Survival Advantage J Traum, 669(1):46-52.
Publisher | Google Scholor