Case Report
Isolated Umbilical Endometriosis (Villar's Nodule): about Two Cases, and Literature Revision
- Moad Belouad *
- Abdelhamid Benlghazi
- Hamza Massoudi
- Saad Benali
- Mly Mehdi Elhassani
- Kouach Jaouad
Departments of Gynecology and Obstetrics, Military Hospital of Instruction Mohamed V, Rabat, Morocco.
*Corresponding Author: Moad Belouad, Departments of Gynecology and Obstetrics, Military Hospital of Instruction Mohamed V, Rabat, Morocco.
Citation: Belouad M, Benlghazi A, Massoudi H, Benali S, Mly M Elhassani, et, al. (2024). Isolated Umbilical Endometriosis (Villar's Nodule): about Two Cases, and Literature Revision. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(3):1-8. DOI: 10.59657/2993-0871.brs.24.034
Copyright: © 2024 Moad Belouad, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 24, 2024 | Accepted: February 17, 2024 | Published: February 27, 2024
Abstract
Without anterior or continuing pelvic endometriosis, villar's nodule is an example of umbilical endometriosis. This nodule's primordial position at the umbilical level is uncommon. Its exact etiopathogenesis is yet unknown. It would occur 1% of the time in all other areas. We report two observations of primary umbilical endometriosis explored by ultrasound and describe the clinical, pathophysiological aspects and the role of imaging in the positive diagnosis of this extremely rare condition, with a review of the literature.
Keywords: endometriosis; villar’s nodule; omphalectomy
Introduction
Primary and secondary umbilical endometriosis is a rare clinical condition representing 0.5 to 1% of all extragenital endometrioses. was first described by Villar in1886 [1]. It is defined as the ectopic localisation of functional endometrium in the umbilical fossa. Its preoperative clinical and ultrasonographic diagnosis is difficult, and its pathophysiology remains a challenge. We report two observations of primary umbilical endometriosis explored by ultrasound and describe the clinical and pathophysiological aspects and the role of imaging in the positive diagnosis of this rare condition, with a review of the literature [2].
Observation
Observation 1: A 30-year-old female, with no previous surgical history and in good health, consulted for the appearance of a nodule over the umbilicus, which had initially been of low symptomatic but had become increasingly uncomfortable and even painful. Clinical examination revealed a nodule directly under the umbilicus, about 2cm in diameter, hard, mobile and tender, with discrete brownish skin discoloration. No spontaneous or provoked umbilical discharge. Abdominal ultrasound revealed a nodule 2 cm in diameter reaching the linea alba, with slight peri-lesional inflammation suggestive of umbilical endometriosis. Wide surgical excision was performed in one piece removing the skin and nodule in their entirety The post-operative phase is simple. Histological analysis confirms the diagnosis of endometriosis, revealing dilated glands filled with macrophagic debris, lined by a cylindrocellular epithelium, strongly associated with a cetogenic stroma.
Figure 1: Post-Operative Image After Nodule Resection.
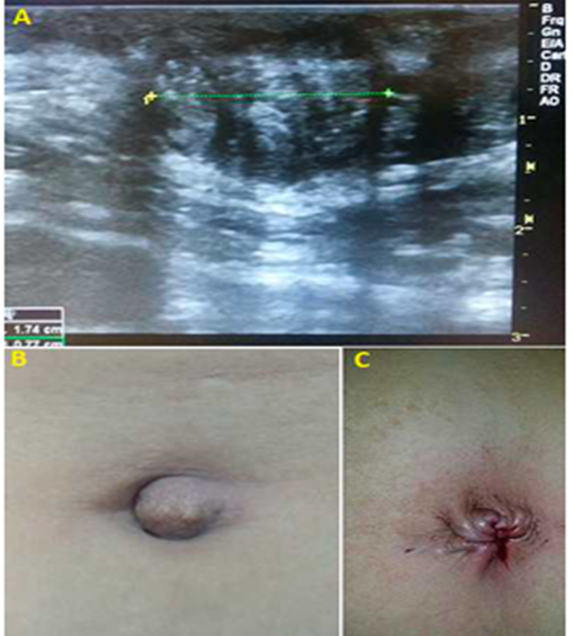
Observation 2: 50-year-old female, 3rd gesture, 3rd pare, postmenopausal for three years, presenting with a painful umbilical tumefaction, sometimes hemorrhagic, progressively increasing in volume, evolving for two months. She had no notable pathological antecedents. An omphalectomy was then performed, with verification of the absence of pelvic endometriosis during laparoscopic exploration. Histological examination of the operative section showed a focus of endometriosis in the dermis and hypodermis, with clean margins of resection. Histopathological examination of the operative specimen showed endometrial glands in an ectopic position, with glandular tubes, cytogenic chorion and muscle fibres.
Figure 2:A) Ultrasound image showing the echo appearance of a Villar nodule. B) pre-operative image of the umbilical region. C) post-operative image after nodule resection.
Discussion
Endometriosis is a chronic gynecological condition that affects millions of women worldwide. It is characterized by the abnormal presence of endometrial tissue, typically found inside the uterus, outside of the uterine cavity. While endometriosis is commonly associated with implants in the pelvic regions, there exists a rare yet significant form called umbilical endometriosis[3]. In this article, we will explore the features, symptoms, causes, and treatment options for umbilical endometriosis. Umbilical endometriosis is an uncommon form of the disease where endometrial implants develop in the umbilical region, or belly button. The lesions can vary in size and depth, ranging from small spots to larger nodules. Symptoms of umbilical endometriosis may resemble those of pelvic endometriosis, but some distinctive signs may include pain, abnormal bleeding, or nodules in the umbilical area [4].
Symptoms of umbilical endometriosis can vary from woman to woman. Some may experience pain in the umbilical area, increased sensitivity of the region, abnormal umbilical bleeding, or the presence of palpable nodules. These symptoms can be mistaken for other conditions, making the diagnosis of umbilical endometriosis more challenging. A thorough medical evaluation, including physical examination, detailed medical history, and possibly imaging tests, can help confirm the diagnosis [5]. Endometriosis and infertility are still linked, although this relationship is still debatable. The American Society of Reproductive Medicine asserts that endometriosis is linked to infertility whether it is severe or moderate [6].
The exact causes of umbilical endometriosis are not fully understood. However, several theories have been proposed to explain its development. The most plausible could be the implantation theory, which assumes that umbilical endometriosis develops as a result of ectopic implantation of endometrial cells from menstrual reflux. This theory could also explain the appearance of pelvic peritoneal implants in laparoscopic patients. The umbilical location could also be explained by the venous or lymphatic metastatic theory, when endometriotic cells migrate to the umbilicus, using the periumbilical venous system. Finally, according to a third theory, that of metaplasia, cells derived from the coelomic epithelium undergo metaplasia towards endometrial cells, under the effect of various infectious, toxic or hormonal factors [7]. MRI can also be a valuable diagnostic aid, revealing a cystic lesion with a homogeneous hyperintense signal in T1 sequence [8]. It can also confirm the existence of other locations, notably pelvic, which could be treated during the same operation, but cannot eliminate the existence of sub-centimetric peritoneal implants.
Ultrasound of the abdominal wall with a high-frequency probe is the initial, easily accessible examination that points to the diagnosis of umbilical endometriosis, but it is not pathognomonic. The treatment of umbilical endometriosis will depend on the severity of symptoms and the patient's future fertility desires. Treatment options may include medications to relieve pain, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or hormonal contraceptives. In more severe cases, surgical intervention may be necessary to remove the endometrial implants from the umbilical region. A multidisciplinary approach involving gynecology specialists, surgeons, and pain management experts may be required to ensure optimal care.
Surgical treatment appears to be the most appropriate [9]. Nodule excision must be sufficiently large to allow excision with healthy margins and avoid recurrence. Early surgical management would enable histologically complete excision and esthetically acceptable repair. Excision may involve the entire thickness of the abdominal wall, in which case laparoscopic exploration of the pelvis is rapid and without additional risk. The wall is closed in anatomical planes, and the umbilical depression is obtained using an absorbable suture that attaches the dermis to the fascia of the rectus muscles. The role of medical treatment in the prevention of umbilical recurrence has not been defined, and it is unlikely that therapeutic trials with a good level of evidence will ever be carried out, given the low prevalence of this location [10].
Conclusion
Umbilical endometriosis is an uncommon condition. It should always be considered in the presence of an umbilical mass associated with cyclical symptoms, and appropriate management should be initiated.
Declarations
Conflict of interest
No conflict of interest.
Funding
No funding
Consent
Informed written consent obtained from the patients.
References
- Michowitz M, Baratz M, Stavorovsky M. (1983). Endometriosis of the umbilicus. Dermatology, 167(6):326-330.
Publisher | Google Scholor - Victory R, Diamond MP, Johns DA. (2007). Villar’s nodule: a case report and systematic literature review of endometriosis externa of the umbilicus. Journal of Minimally Invasive Gynecology, 14(1):23-32.
Publisher | Google Scholor - Benardete-Harari DN, Muñoz-de Cote Frade JM, Hidalgo-Carrera JA, Felgueres-Hermida A, Meraz-Ávila D. Primary umbilical endometriosis (Villar’s nodule): case report. Revista Médica del Instituto Mexicano del Seguro Social, 56(2):203-206.
Publisher | Google Scholor - Pariza G, Mavrodin C. (2014). Primary umbilical endometriosis (Villar's nodule)-case study, literature revision. Chirurgia (Bucur), 109(4):546-549.
Publisher | Google Scholor - Moustaghfir I, Adamski H, Le Gall F, Chevrant-Breton J, editors. (2010). Case for diagnostic: umbilical pigmented lesion. Annales de Pathologie.
Publisher | Google Scholor - Canis M, Donnez JG, Guzick DS, Halme JK, Rock JA, Schenken RS, et al. (1997). Revised american society for reproductive medicine classification of endometriosis: 1996. Fertility and sterility, 67(5):817-821.
Publisher | Google Scholor - Teh W-T, Vollenhoven B, Harris PI. (2006). Umbilical endometriosis, a pathology that a gynecologist may encounter when inserting the Veres needle. Fertility and sterility, 86(6):1-2.
Publisher | Google Scholor - Hartigan C, Holloway B. (2005). MR imaging features of endometriosis at the umbilicus. The British Journal of Radiology.78(932):755-757.
Publisher | Google Scholor - Purvis RS, Tyring SK. (1994). Cutaneous and subcutaneous endometriosis: surgical and hormonal therapy. The Journal of dermatologic surgery and oncology, 20(10):693-695.
Publisher | Google Scholor - Ploteau S, Malvaux V, Draguet A-P. (2007). Primary umbilical adenomyotic lesion presenting as cyclical periumbilical swelling. Fertility and sterility, 88(6):1674-1675.
Publisher | Google Scholor