Case Report
Intramedullary Tuberculosis of Cervical Spine in An Infant- A Rare Case Report
- Dr Areesha Shakeel
- Dr Areeba Tariq *
- Syed Ahsan Ali Jafri
- Sara Khalil
- Dr Saad Akhtar Khan
Liaquat National Hospital, Karachi, Pakistan.
*Corresponding Author: Areeba Tariq,Liaquat National Hospital, Karachi, Pakistan.
Citation: Shakeel A, Tariq A, S.A.A. Jafri, Khalil S, Saad A. Khan. (2024). Intramedullary Tuberculosis of Cervical Spine in An Infant- A Rare Case Report. International Journal of Medical Case Reports and Reviews, BioRes Scientia Publishers. 3(6):1-4. DOI: 10.59657/2837-8172.brs.24.063
Copyright: © 2024 Areeba Tariq, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 31, 2024 | Accepted: August 24, 2024 | Published: August 17, 2024
Abstract
Tuberculosis is an endemic disease of developing world but intrame Tuberculosis is an endemic disease of developing world but intramedullary tuberculoma manifests rarely. Spinal tuberculoma can be classified on the basis of their location as extradural, intramedullary or intradural extra medullary the symptoms are variable in different patients, but the disease often presents with progressive weakness and numbness in the extremities, quadriparesis, back pain, and bowel or bladder dysfunction. The tumor is typically seen in pediatrics, immunocompromised, alcoholics, malnourished and patient with any cancerous condition at high risk of CNS TB.
Keywords: intramedullary; tuberculosis; cervical spine; infant
Introduction
Tuberculosis is an endemic disease of developing world but intrame Tuberculosis is an endemic disease of developing world but intramedullary tuberculoma manifests rarely [1]. Spinal tuberculoma can be classified on the basis of their location as extradural, intramedullary or intradural extra medullary the symptoms are variable in different patients, but the disease often presents with progressive weakness and numbness in the extremities, quadriparesis, back pain, and bowel or bladder dysfunction [2,3]. The tumor is typically seen in pediatrics, immunocompromised, alcoholics, malnourished and patient with any cancerous condition at high risk of CNS TB [5]. Due to nonspecific clinical presentation, diagnosis of intramedullary tuberculoma is usually diagnosis of exclusion [3]. Diagnosis starts with comprehensive medical history and examination. This enables to recognize the risk factors for expected tuberculosis. Secondly imaging plays a significant role in identifying the site, size and characteristics of the lesion. For this, MRI is the gold standard for diagnosis [6]. However, only biopsy can provide the definitive diagnosis for intramedullary tuberculoma, as it categorizes mycobacterial markers, and is consequently the gold standard [7]. Moreover, patients from endemic region presenting with aforementioned symptoms should be considered highly suspicious of this disease. Treatment is multidisciplinary which involves administration of antituberculosis drugs for 9 to 12 months. In severe cases like a patient is unresponsive to medical therapy, surgical intervention may be required [5]. In this case report, we present a case of intramedullary tuberculoma in one year old boy and how he was managed for this condition. Dullary tuberculoma manifests rarely [1]. Spinal tuberculoma can be classified on the basis of their location as extradural, intramedullary or intradural extra medullary the symptoms are variable in different patients, but the disease often presents with progressive weakness and numbness in the extremities, quadriparesis, back pain, and bowel or bladder dysfunction [2,3]. The tumor is typically seen in pediatrics, immunocompromised, alcoholics, malnourished and patient with any cancerous condition at high risk of CNS TB [5]. Due to nonspecific clinical presentation, diagnosis of intramedullary tuberculoma is usually diagnosis of exclusion [3]. Diagnosis starts with comprehensive medical history and examination. This enables to recognize the risk factors for expected tuberculosis. Secondly imaging plays a significant role in identifying the site, size and characteristics of the lesion. For this, MRI is the gold standard for diagnosis [6]. However, only biopsy can provide the definitive diagnosis for intramedullary tuberculoma, as it categorizes mycobacterial markers, and is consequently the gold standard [7]. Moreover, patients from endemic region presenting with aforementioned symptoms should be considered highly suspicious of this disease. Treatment is multidisciplinary which involves administration of antituberculosis drugs for 9 to 12 months. In severe cases like a patient is unresponsive to medical therapy, surgical intervention may be required [5]. In this case report, we present a case of intramedullary tuberculoma in one year old boy and how he was managed for this condition.
Case presentation
A one-year-old boy presented though ER with complaints of bilateral upper limb weakness for two weeks. His right hand was affected first and then gradually, weakness developed in left hand as well. There was no weakness of lower limbs. There was no history of fever, or trauma. TB contact history was also negative. On examination, there was an awake and active child with decreased tone in both upper limbs and power grossly 0/5 with exaggerated reflexes. Lower limbs tone and power was normal. No tenderness or gibbus deformity was noted on local examination of back and neck. Rest of neurological as well as systemic examination was unremarkable. His MRI cervical spine was performed which showed a lobulated intramedullary area of heterogeneous signal intensity with post contrast enhancement seen extending from the level C2 to upper endplate of C5 vertebra causing significant swelling of cord. It measured approximately 1.0 x 0.8 x 3.5cm. On right side its extended from the level of C2 to D7 and on left side from C2 to C4 vertebra. There was significant intradural enhancement around nerve roots of cauda L2 to S1 vertebra, on surface of entire spinal cord with few adhesions extending laterally. Edema and significant enhancement around nerve roots of cauda equina was also present.
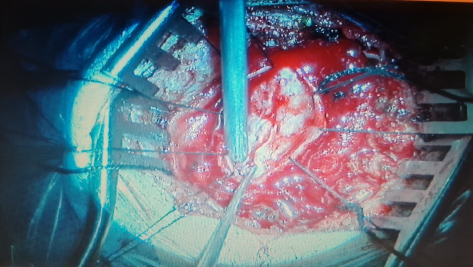
Figure 1: Patient underwent cervical laminoplasty and excision of intramedullary abscess. Intra-operative findings included: fish meat like granulation tissue was present with cystic components.
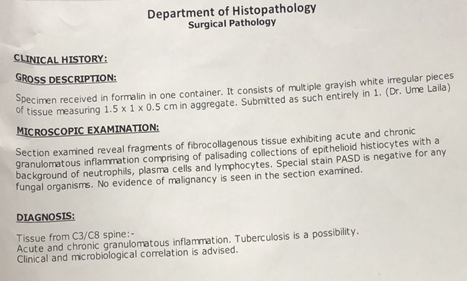
Figure 2: The child was discharged on second post op day. He had an uneventful recovery and regained his upper limb powers. On OPD follow up 20 days after surgery, patient had fully regained his powers and had no remaining deficits. Histopathology showed acute and cgronic inflammation with tuberculosis as a possibility.
Figure 3: Anti-tuberculous therapy was continued till 9 months as advised by infectious diseases specialist.
Discussion
Tuberculosis (TB) is a bacterial infection caused by Mycobacterium tuberculosis (M. tuberculosis), presenting a global health concern. Among its various forms, central nervous system TB is particularly severe, often leading to complications with high morbidity and mortality rates [8]. This type of TB triggers a robust granulomatous inflammatory response, typically detectable through MRI imaging. However, diagnosing CNS TB is challenging due to the diverse spectrum of MRI appearances and clinical features, which vary depending on the affected region and complications. Intramedullary tuberculomas are exceptionally rare, occurring in only 2 out of every 1000 cases of CNS TB. Involving the spine in roughly 50% of CNS TB cases, tuberculosis manifests most commonly as tuberculous spondylitis, followed by arachnoiditis, meningitis, and intramedullary lesions. Intramedullary involvement typically presents as radiculomyelitis, transverse myelitis, intraspinal space-occupying lesions, or anterior spinal artery thrombosis [9]. While spinal intramedullary tuberculomas are infrequent, they generally respond well to conventional anti tuberculous medications, necessitating surgical intervention only in rare cases. MRI serves as the optimal diagnostic tool for spinal intramedullary tuberculosis, offering precise localization, sizing, and lesion enumeration, as well as detection of associated degeneration and necrosis. The radiological presentation varies depending on the tuberculoma's stage, with early phases characterized by severe infective reactions, poor gel capsule formation, and significant edema around the lesion. As the tuberculoma progresses, MRI signals evolve, with T1-weighted and T2-weighted sequences initially showing equal signal intensity, followed by rim enhancement and the characteristic "target sign" indicative of caseation. Treatment outcomes are generally favorable with combined surgical and medical approaches. However, medical treatment is typically prioritized, particularly in endemic regions like India or when radiological findings strongly suggest intramedullary tuberculoma. Surgery is reserved for cases with neurological deficits, presence of paravertebral abscess, resistance to antituberculous treatment, or risk of spinal instability. Our patient presented to us with neurological detoriation and due to young age and vague MRI findings,our provisional diagnosis was some intramedullary neoplastic lesion . it was only after histopathology that tuberculosis was identified. Although, a similar case in adult has been reported in thoracic spine in literature, no study was found for such a presentation in pediatrics and cervical spine [10]. Hence, tuberculosis should always be considered a differential diagnosis in endemic region in unusual case presentations.
Conclusion
Tuberculosis is a disease of developing countries and still a lot of research is lacking on its unusual presentations. Tuberculosis should be considered in all cases of diagnostic dilemma.
References
- Du Plessis J, Andronikou S, Theron S, Wieselthaler N, Hayes M. (2008). Unusual forms of spinal tuberculosis. Child's Nervous System. 24(4):453-457.
Publisher | Google Scholor - Biakto KT, Arifin J, Wonggokusuma G, Micelli C. (2020). Tuberculoma of spine mimicking intramedullary tumour: A case report. Int J Surg Case Rep, 76:231-236.
Publisher | Google Scholor - Qu LM, Wu D, Guo L, Yu JL. (2020). Paraplegia from spinal intramedullary tuberculosis: A case report. World J Clin Cases, 8(24):6353-6357.
Publisher | Google Scholor - Kobayashi K, Imagama S, Ito Z, Ando K, Yagi H, Shinjo R, et al. (2015). Tuberculous meningitis with dementia as the presenting symptom after intramedullary spinal cord tumor resection. Nagoya J Med Sci, 77(4):653-657.
Publisher | Google Scholor - Meegada S, Gyamfi R, Muppidi V, Dandu V, Challa T. (2020). Multiple Intracranial Tuberculomas with an Intra-medullary Spinal Cord Tuberculoma in a Pediatric Patient. Cureus, 12(3): e7248.
Publisher | Google Scholor - Lu M. (2010). Imaging diagnosis of spinal intramedullary tuberculoma: case reports and literature review. J Spinal Cord Med, 33(2):159-162.
Publisher | Google Scholor - Rajasekaran S, Soundararajan DCR, Shetty AP, Kanna RM. Spinal Tuberculosis: Current Concepts. Global Spine J. 2018;8(4 Suppl):96s-108s.
Publisher | Google Scholor - Ramdurg SR, Gupta DK, Suri A, Sharma BS, Mahapatra AK. (2009). Spinal intramedullary tuberculosis: a series of 15 cases. Clinical neurology and neurosurgery. 111(2):115-118.
Publisher | Google Scholor - Sardana V, shringi P. Intramedullary tuberculoma of the Spinal Cord, Clinical features & imaging: Possibility of early diagnosis with imaging? Indian Journal of Tuberculosis,
Publisher | Google Scholor - Abdu AM, Alshoabi SA, Arafah MA, Hamid RA, Hamid AM, Kocak M. (2023). Intramedullary tuberculoma of the thoracic spine presented as paraparesis: A rare case report. Radiol Case Rep, 19(1):310-31s4.
Publisher | Google Scholor