case report
Intentional Replantation to Seal Apical and Lateral Canals in A Failed Endodontically Treated Tooth: A Case Report
Iranian Centre for Endodontic Research, Research Institute of Dental Sciences, Shahid Beheshti University of Medical Sciences, Evin, Tehran, Iran.
*Corresponding Author: Saeed Asgary,Iranian Centre for Endodontic Research, Research Institute of Dental Sciences, Shahid Beheshti University of Medical Sciences, Evin, Tehran, Irna.
Citation: Asgary. S. (2023). Intentional Replantation to Seal Apical and Lateral Canals in a Failed Endodontically Treated Tooth: A Case Report. Dentistry and Oral Health Care, Biores Scientia Publishers 2(4):1-3. DOI: 10.59657/2993-0863.brs.23.019
Copyright: © 2023 Saeed Asgary, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: October 16, 2023 | Accepted: October 26, 2023 | Published: November 02, 2023
Abstract
Intentional replantation (IR) is often viewed as a last-resort intervention for failed endodontically treated teeth. This case report presents the successful management of symptomatic apical and lateral lesions through IR, highlighting its potential as an effective solution for challenging endodontic cases. A 45-year-old female patient presented with persistent pain and recurrent labial swelling in the vicinity of her left anterior tooth. Cone-beam computed tomography revealed endodontic lesions at both the apical and mesial aspects of tooth #21, leading to a diagnosis of symptomatic apical periodontitis. The IR procedure involved meticulous preparation and sealing of both apical and lateral canals with calcium-enriched mixture cement. One-year post-treatment, the patient remained asymptomatic, with clinical and radiographic assessments demonstrating a favorable prognosis and evidence of bone healing. This case demonstrates the successful management of symptomatic apical and lateral lesions through IR, offering an effective solution for challenging endodontic cases.
Keywords: intentional replantation; endodontics; apical periodontitis; cem cement
Introduction
The need for endodontic interventions often arises due to the complex nature of dental pathologies. Failed endodontically treated teeth pose a substantial challenge for both patients and dental professionals. When standard endodontic retreatment proves insufficient to address these issues, innovative approaches become essential. In such cases, intentional replantation (IR), despite being a less common procedure, can offer an effective solution [1]. The IR technique defines as extraction of an endodontically involved tooth, doing treatment procedures extra orally, and insertion of the tooth back into its alveolar socket. When endodontic surgery is necessary, but is not possible or practical, IR is a viable treatment option; with careful case selection, it has high success rate [2]. When conventional endodontic treatment proves ineffective, the presence of a significant apical lesion extending into the adjacent bone signals a challenging pathological condition. Moreover, the identification of lateral lesions, commonly linked with lateral canals, underscores the intricate anatomical variations that necessitate meticulous management. In routine endodontic procedures, these lateral and accessory canals are often left instrumented and unfilled [3]. This approach is grounded in the assumption that when the primary canal is thoroughly cleaned and shaped, the body's natural healing processes may overlook and effectively manage the lower pathological intrusion associated with these anatomical complexities. This case highlights the successful management of symptomatic apical and lateral lesions through IR, showcasing the potential of this procedure as an effective solution for challenging endodontic cases. Furthermore, it underscores the significance of comprehensive diagnostic evaluation, novel techniques, and biocompatible materials in achieving positive clinical outcomes.
Case presentation
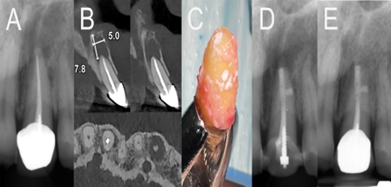
A 45-year-old female patient sought dental care with a chief complaint of persistent pain and recurrent labial swelling around her left anterior tooth. This discomfort and swelling raised significant dental concerns. Upon clinical examination, the patient exhibited tenderness and substantial swelling in the labial region adjacent to the upper left central incisor. Importantly, neighboring teeth displayed normal sensitivity, further isolating the patient's discomfort. The initial periapical radiograph disclosed that the affected tooth had previously undergone endodontic treatment and presented a sizable apical lesion along with bone resorption in the distal aspect of the midfoot (Fig. 1A). Subsequently, we conducted a Cone-beam computed tomography (CBCT) imaging to obtain a comprehensive view of the involved tooth and its surrounding tissues. This radiographic assessment unveiled the presence of endodontic lesions at both the apical and distal aspects of the mid-root of the left anterior tooth (Fig. 1B). The amalgamation of clinical presentation, radiographic evidence, and the patient's reported symptoms led to the diagnosis of symptomatic apical periodontitis affecting tooth #21. This diagnosis underscored the need for a definitive and effective treatment approach to address the intricate endodontic pathology. Given the diagnosis, several treatment options were considered, including non-surgical endodontic retreatment coupled with prosthetic restoration, tooth extraction and implant replacement, periarticular surgery, and IR. The patient opted for IR. Informed consent was duly obtained. The treatment procedure was performed by an experienced endodontist. After a 0.12% chlorhexidine mouth rinse, local anesthesia with 2% lidocaine plus 1:80,000 epinephrine was administered. Subsequently, the tooth was meticulously extracted, and while holding the tooth by the crown, approximately 2 mm of root apices were resected using a diamond bur in a high-speed handpiece. Using Gates Glidden burs #2-3, 3-mm depth root-end cavities were prepared. The procedure also revealed a lateral canal, which was located with high magnification and exploration using an endodontic explorer. A suitable retro tip was employed to create a cavity, into which a mixture of calcium-enriched mixture (CEM) cement powder and liquid, prepared according to the manufacturer’s instructions, was inserted (Fig. 1C). Following saline rinsing and the aspiration of blood clot with suction, the tooth was carefully replanted into the alveolar socket and secured to adjacent teeth using resin composite (Fig. 1D). The total extraoral operation time was 10 minutes. Postoperative instructions, including meticulous oral hygiene, chlorhexidine mouth rinse, and a soft diet, were provided. The patient's progress was closely monitored in the post-treatment phase to assess the effectiveness of the chosen intervention. Following the IR, the patient was observed for a one-year period post-treatment. During this follow-up period, the patient remained asymptomatic, with no signs of swelling or discomfort reported. Radiographic assessments conducted at the one-year follow-up period indicated favorable outcomes, with evidence of bone healing and a positive prognosis for the treated tooth (Fig. 1E).
Figure 1: Radiographic assessment of the failed endodontically treated tooth (#21) and the IR procedure. A: Initial periapical radiograph revealing a failed endodontically treated tooth with a big apical lesion and bone resorption in the distal aspect of the midfoot. B: CBCT image showing endodontic lesions at both the apical and distal aspects of the mid-root. C: Intraoperative image illustrating the preparation and sealing of apical and lateral canals with calcium-enriched mixture (CEM) cement during the intentional replantation procedure. D: Radiographic image post-IR, showcasing the repositioned tooth and the use of resin composite to secure it to adjacent teeth. E: Radiographic image at the one-year follow-up, indicating favorable outcomes with evidence of bone healing and a positive prognosis for the treated tooth.
Discussion
Endodontically treated teeth that present with complex and persistent pathologies pose significant challenges for dental professionals. The failure of conventional endodontic treatment can lead to substantial apical lesions, and in some instances, the involvement of lateral canals, representing intricate anatomical variations demanding meticulous management. Often, in routine endodontic procedures, these lateral and accessory canals are left untreated, with the assumption that a well-prepared main root canal(s) will allow the body's natural healing processes to manage any lower pathological invasion associated with these anatomical complexities. The successful treatment of a failed endodontically treated tooth in this case through IR, sealing both apical and lateral canals with CEM cement, offers valuable insights into managing complex endodontic pathologies. The clinical and radiographic outcomes at the one-year follow-up underscore the effectiveness and reliability of IR, even in cases involving substantial apical and lateral lesions. The choice of IR was made, considering the specific case details, and informed consent was obtained. The procedure was performed by an experienced endodontist and involved the meticulous extraction of the tooth, resection of approximately 2 mm of root apices, and preparation of 3-mm depth root-end cavities. Importantly, during the procedure, a lateral canal was identified and thoroughly treated. The prepared cavities were filled and sealed with CEM cement; a bioactive material known for its favorable properties in endodontics [1]. The postoperative phase of the patient's treatment involved close monitoring for one year. During this time, the patient remained asymptomatic, with no signs of swelling or discomfort. Radiographic assessments at the one-year follow-up indicated favorable outcomes, including evidence of bone healing and a positive prognosis for the treated tooth. This case demonstrates that IR can be a successful approach for the management of complex endodontic cases, even when apical and lateral lesions are present. Moreover, it emphasizes the importance of thorough diagnostic evaluation, the utilization of innovative techniques, and biocompatible materials such as CEM cement in achieving positive clinical outcomes. The successful management of symptomatic apical and lateral lesions through IR highlights the potential of this procedure as an effective solution for challenging endodontic cases.
Conclusion
This case serves as a testament to the importance of considering innovative treatment approaches when conventional endodontic procedures prove insufficient. The utilization of meticulous diagnostic evaluation, advanced techniques, and biocompatible materials can lead to positive clinical outcomes, ultimately benefiting both patients and dental professionals.
References
- Asgary S, Alim Marvasti L, Kolahdouzan A. (2014). Indications and case series of intentional replantation of teeth. Iran Endod J, 9(1):71-78.
Publisher | Google Scholor - Javed F, Zafar K, Khan FR. (2023). Outcome of intentional replantation of endodontically treated teeth with periapical pathosis: A systematic review and meta-analysis. Aust Endod J, 49(1):494-507.
Publisher | Google Scholor - Kishen A. (2010). Advanced therapeutic options for endodontic biofilms. Endodontic Topics, 22(1):99-123.
Publisher | Google Scholor