Research Article
Initiation Time of Breastfeeding and Associated Factors among Mothers Delivering at Southwest Region Hospitals, Ethiopia
1Department of Nursing, Collage of Health Science, Institute of Health, Mizan Tepi University, Ethiopia.
2School of Midwifery, Faculty of Health Science, Institute of Health, Jimma University, Ethiopia.
*Corresponding Author: Tsegaw Biyazin ,School of Midwifery, Faculty of Health Science, Institute of Health, Jimma University, Ethiopia.
Citation: Dagnaw Y, Fenta B, Biyazin T, Yetwale A. (2023). Initiation Time of Breastfeeding and Associated Factors among Mothers Delivering at Southwest Region Hospitals, Ethiopia, Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 2(3):1-9, DOI: 10.59657/2993-0871.brs.23.014
Copyright: © 2023 Tsegaw Biyazin, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 19, 2023 | Accepted: September 15, 2023 | Published: September 19, 2023
Abstract
Background: Breastfeeding is a pillar practice during the postnatal period. Recognizing factors associated with the initiation of breastfeeding plays a huge role in improving the habit of breastfeeding. This study aimed to determine and identify factors affecting the timely initiation of breastfeeding among mothers who delivered preterm neonates.
Methods: Institutional based cross-sectional study was conducted among 480 women at Southwest Regional hospitals from March to September 30/2020, in Ethiopia. Study participants were nominated using a systematic random sampling technique. Data were collected using pretested and interviewer-administered questionnaires. The data were entered into Epi data version 3.5 and analyzed using SPSS version 25. Binary and multivariate logistic regression analyses were performed to determine the association between predictors and timely initiation breastfeeding initiation.
Results: Early initiation of breastfeeding was 41% (95% of the confidence interval: 37.1%-45.6%). History of Antenatal care visits (AOR= 6.04, 95%CI 3.14-11.58), 1st minute Apgar <7 scores (AOR=0.57, 95% CI 0.33-0.98), and neonates who received kangaroo mother care (AOR=4.46, 95% CI 2.79-7.13) were positively associated with timely initiation of breastfeeding. Women who gave birth through cesarean section were initiated breastfeeding lately (AOR= 0.37, 95% CI 0.19-0.69) than women who gave birth via spontaneous vagina delivery.
Conclusion: In this study early initiation of breastfeeding was low. Antenatal care follow-up, low 1st minute Apgar score, caesarian section, and received kangaroo mother care had a significant effect on the initiation of breastfeeding. All concerned bodies have to engage to promote the timely initiation of breastfeeding for lactating women.
Keywords: breastfeeding; neonate; early; late; preterm
Introduction
Breastfeeding is the ideal and natural way to nurture infants. Mother’s milk is the most complete food in the first six months of life [1]. Due to nature’s giftedness, it is the most feasible, cost-effective, and affordable irrespective of the country’s wealth. According to the world Health Organization recommendation guidelines, mother's milk must be started immediately after delivery and it must be considered the only food for the baby in the first six months of life and then it should be preserved minimum of two years combined with a child’s diet [2].
Breastfeeding is the only means of obtaining nutrition for neonates until six months and has a variety of roles including; mother-infant bonding, growth, and development, being mentally capable, enhancing the baby’s immunity, disease prevention, and minimizing morbidity and mortality in infants [3, 4] (Layuk, Wardihan, and Asad, 2021). In addition to infants' benefits, the timely practice of breastfeeding has also owned maternal-side benefits regards decreasing the amount of vaginal blood loss and improving uterine involution through stimulation of oxytocin production and facilitating uterine contraction during the postpartum period [6]. By considering those benefits, World Health Organization strongly recommended initiation of breastfeeding within one hour after birth for infants to reach 90%. On the contrary, delayed initiation of breastfeeding has been found to increase early neonatal morbidity, mortality, and impaired mother-infant bonding [7, 8]. Indeed, mothers who delivered preterm neonates made the problems worse.
The Early initiation of breastfeeding (EIBF) prevalence varies widely among countries and ranging from 17 % to 98% [9]. According to studies conducted in Africa including Northwest Ethiopia [10], Tanzania [11], Burkina Faso [12], Cameroon [13], and Ghana [14] revealed that 75%, 83%, 41%,40%,& 39.4% of neonates practiced late initiation of breastfeeding respectively. Furthermore, a Meta-analysis in Middle Eastern countries [15] indicated that 34.3% ([CI]: 20.2%-51.9%) of newborns received breastfeeding initiated within an hour of birth. The United Nations International Children's Emergency Fund (UNICEF) reported that 56% of neonates practiced early initiation of breastfeeding in East Europe and Central Asia [16].
Numerous factors affecting breastfeeding initiation, such as low birth weight and preterm infants, neonatal illness, mother’s age, mother’s educational level, child’s birth weight, household economic status, and residential area are the predominant factors reported in previous studies [17,18]. Moreover, maternal knowledge and perception play an undeserved role in the timely initiation of breastfeeding.
Despite the current World Health Organization plan and strong recommendations, late initiation and holding breastfeeding at the beginning are commonly practiced in the present study setting, Ethiopia. Generally, to the best of our knowledge, there are limited published studies have been available on breastfeeding; specifically, on the timely initiation of breastfeeding among women who delivered preterm neonates at Southwest region hospitals, in Ethiopia. Therefore, this study aimed to identify the proportion and factors affecting the timely initiation of breastfeeding among preterm delivered mothers in Southwest region hospitals, in Ethiopia.
Methods and Materials
Study setting
The study was conducted at Southwest Region public hospitals, in Ethiopia namely Mizan-Tepi University teaching hospital, Tepi general hospital, and G/tsadik Shawa General Hospital. All hospitals provided delivery services with postpartum care. More than 665 newborns were delivered monthly in three governmental hospitals (Mizan-Tepi University teaching hospital, Tepi General Hospital, and G/tsadik Shawo general hospital) (Source: the previous hospitals' quarter report).
Study design and study participants
A facility based cross-sectional study was conducted among mothers who delivered preterm neonates at Southwest region hospitals from March 2020 to September 30/2020. All mothers who delivered preterm neonates at Southwest region hospitals were considered the source population, while women who delivered preterm neonates at Bench Sheko, Kafa, and Sheka zone hospitals during the data collection period were considered the study population.
Inclusion and exclusion criteria
Mothers who delivered live preterm neonates at Southwest region hospitals were included in this study. Mothers with contraindications to breastfeeding, newborns' congenital anomalies (Cleft lip and cleft palate), and those with newborns presenting emergencies that needed urgent management at birth, such as major digestive malformation, and neurologic problems with feeding disorders were excluded.
Sample size determination and sampling technique
Sample size determination
A single population proportion formula was used to calculate the sample size by considering the following statistical assumptions with proportion (P) = prevalence of timely initiation breastfeeding which took from a previous Ethiopian DHS report [10], which accounts for 75 %, 95% confidence interval at Z α/2 (=1.96) and Margin of error (d) = (4%).


After adding a 10% non-response rate, the total sample size was 495.
Sampling technique
All three hospitals found in Bench Sheko, Kafa, and Sheka zone were included in this study. The sample size was proportionally allocated to each health facility. A systematic sampling technique was used to select individual study participants using patients assigned serial numbers.
Terms definition
Early breastfeeding: initiation of mother's breast milk to infants within one hour of birth[19].
Late breastfeeding: Provision of mother's breast milk to infants one hour after birth.
Preterm: Infants are delivered before 37 weeks, but after 28 weeks of gestational age [20].
Data collection instrument and procedure
Data were collected through face-to-face interviews using a structured and pretested questionnaire adapted from the previous literature(Salasibew, Filteau, and Marchant, 2014). The questionnaire had three sections including socio-demographic characteristics, maternal characteristics, and neonatal characteristics.
Quality Control
First the questionnaires were prepared in the English language then translated into the local language spoken in the study area (Amharic language) and back-translated into English. A pretest of the study was conducted in another setting with a small sample (5%) before the actual data collection period to ascertain questionnaire consistency. Six BSc nurses and three MSc personnel were recruited as the data collectors and supervisors respectively. Data collectors were trained in the data collection process for one day. The principal investigator checked the data for completeness and consistency at the end of every day.
Data Analysis
Data entry and coding were performed using Epi-data version 3.5 and data analysis was performed using SPSS version 25. Binary and multivariate analyses were used to determine the factors associated with the timely initiation of breastfeeding. Odds ratios and -95% confidence intervals were used to measure the strength of the association between the timely initiation of breastfeeding and independent variables. In binary logistic regression variables with P-value of less than 0.25 were considered candidate variables for multivariate regression, while in multivariate logistic regression variables with a p-value less than 0.05 were considered statistically significant. Descriptive analysis frequencies, percentages, means, and standard deviations were computed to explore the socio-demographic characteristics of the study participants. The results were presented using text, tables, figures, and graphs.
Ethical consideration
Ethical approval letters were obtained from the institutional review board (IRB) of Mizan Tepi University. Permission letters were written to the administrators of each hospital. The participants were informed of the study’s objectives and their right to terminate their participation at any time and they were informed that their information was kept confidential and that verbal informed consent was obtained from all participants.
Results
Socio-demographic and obstetric Characteristics
A total of 480 participants were rolled in an interview with a response rate of 97%. The majority of -416(86.7%) respondents were found in the age range between 20-34 years (Mean age with SD; 25.26±4.37). More than two-thirds 324(67.9%) of the participants were living in rural and approximately half 236 (49.2%) of respondents were prim-gravidas. The majority of 388(80.8%) participants had antenatal care visits, of which only 119(24.8%) fulfilled the minimum requirement or recommendation for ANC follow-up (Table 1).
Table 1: Maternal and neonatal characteristics at Southwest region hospitals, Southwest Ethiopia, 2021.
| Variables | Category | Frequency (N) | Percent (%) |
| Age of mother | <20> | 45 | 9.4 |
| 20-34 | 416 | 86.7 | |
| >=35 | 19 | 4 | |
| Mean & SD | 25.26±4.37 | ||
| Maternal residency | Urban | 154 | 32.1 |
| Rural | 326 | 67.9 | |
| Parity | Prime-gravida | 236 | 49.2 |
| Multigravida | 244 | 50.8 | |
| Type of pregnancy | Single | 370 | 77.1 |
| Multiple | 110 | 22.9 | |
| Had Antenatal care visit | Yes | 388 | 80.8 |
| No | 92 | 19.2 | |
| Number of ANC Visit | 1-3 | 269 | 55 |
| 4 | 119 | 24.8 | |
| Place of delivery | Home | 23 | 4.8 |
| Health institution | 457 | 95.2 | |
| Type of Presentation | Cephalic | 410 | 85.4 |
| Non-cephalic | 70 | 14.6 | |
| Mode of delivery | SVD | 386 | 80.4 |
| Caesarian section | 94 | 19.6 | |
| Any obstetrics complication during delivery | No | 433 | 90.2 |
| Yes | 47 | 9.8 | |
| Had the neonate been diagnosed with asphyxia | No | 395 | 82.3 |
| Yes | 85 | 17.7 | |
| 1st minute APGAR score | 7-10 | 342 | 71.3 |
| <7> | 138 | 28.8 | |
| Had neonate received KMC | No | 217 | 45.2 |
| Yes | 263 | 54.8 |
More than half 291(60.6%) of neonates’ sexes were male and the majority 287 (59.8%) of neonates’ gestational age was lies under 32-37weeks at birth (Table 2).
Table 2: Neonatal characteristics at southwest region hospitals, southwest Ethiopia, 2021.
| Sex of neonate | Female | 189 | 39.4 |
| Male | 291 | 60.6 | |
| Gestational age at birth | 28-32Wk | 193 | 40.2 |
| 32.1-37Wk | 287 | 59.8 | |
| Birth Weight | <1000> | 26 | 5.4 |
| 1000-1499 | 186 | 38.8 | |
| 1500-2499 | 259 | 54.0 | |
| 2500-3999 | 9 | 1.9 |
Initiation of breastfeeding
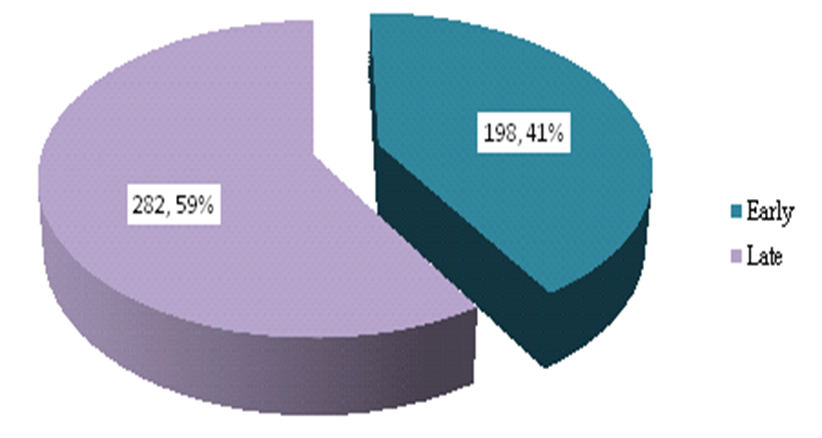
Figure 1: The status of initiation of breastfeeding at Southwest region hospitals, Southwest Ethiopia, 2021.
More than half 198(41%) of the respondents have practiced late initiation of breastfeeding; the remaining respondents had commenced breastfeeding within one hour (Figure 1).
Bivariate and Multivariate logistic regression
In binary logistic regression, predictors including residence, parity, women who had ANC visits, place of delivery, mode of delivery, neonates who developed Asphyxia, first minute Apgar score, and neonates who received KMC service were a candidate for multivariate logistic regression. However, multivariate analysis showed that only four variables were statistically associated with the initiation of breastfeeding. These predictors included ANC visits (AOR= 6.04, 95%CI 3.14-11.58), mode of delivery (AOR= 0.37, 95% CI 0.19-0.69), 1st minute Apgar <7 AOR=0.57, AOR=4.46,>
Respondents who had ANC visits during their pregnancy were six times more likely to practice early breastfeeding initiation than those who didn’t have any ANC follow-up during pregnancy (AOR= 6.04, 95%CI 3.14-11.58). In part, the mode of delivery was also a significant predictor for the time of breastfeeding initiation; neonates who were born via cesarean section were 63% times less likely to initiate early breastfeeding than those born through spontaneous vaginal delivery (AOR= 0.37, 95% CI 0.19-0.69). Furthermore, neonates with Apgar scores < 7 AOR=0.57, AOR=4.46,>
Table 3: Bivariate and multivariate logistic regression results of Factors affecting initiation of breastfeeding among mothers gave preterm neonates in Southwest region’s hospitals, Southwest Ethiopia, 2021.
| Variables | Category | Initiation of breast feeding | COR [ 95%CI] | AOR [95%CI] | P-Value | |
| Early | Late | |||||
| Age of mother | <20> | 19 | 26 | ** | ||
| 20-34 | 168 | 248 | 0.93(0.49-1.73) | .74(.36-1.50) | .403 | |
| >=35 | 11 | 8 | 1.88(0.63-5.57) | 1.10(.31-3.93) | .878 | |
| Maternal residence | Urban | 74 | 80 | 1.51(1.02-2.22) | 1.55(0.97-2.48) | 0.066 |
| Rural | 124 | 202 | ** | |||
| Parity | <=1 | 86 | 150 | ** | ||
| >=2 | 112 | 132 | 1.48(1.03-2.13) | 1.18(0.76-1.84) | 0.451 | |
| Type of pregnancy | Single | 155 | 215 | ** | ||
| Multiple | 43 | 67 | 0.9(0.57-1.37) | .79(.48-1.31) | .368 | |
| Antenatal care visit | Yes | 173 | 215 | 2.15(1.31-3.56) | 6.04(3.14-11.58) | 0.000* |
| No | 25 | 67 | ** | |||
| Presentation at delivery | Cephalic | 170 | 240 | ** | ||
| Non-cephalic | 28 | 42 | 0.94(0.56-1.57) | 2.64-1.31-5.30) | .006 | |
place of delivery
| Health institution | 185 | 272 | ** | ||
| Home | 13 | 10 | 2.09(0.84-5.44) | 1.05(0.39-2.93) | 0.888 | |
| Mode of delivery | SVD | 174 | 212 | ** | ||
| Caesarian section | 24 | 70 | 0.42(0.25-0.69) | 0.37(0.19-.69) | 0.002* | |
| Sex of the newborn | Female | 74 | 115 | ** | ||
| Male | 124 | 167 | 1.15(0.79-1.67) | 1.17(.754-1.82) | .482 | |
| Neonate diagnosed with sepsis | No | 42 | 68 | ** | ||
| Yes | 156 | 214 | 1.18(0.76-1.86) | 1.08(.65-1.80) | .751 | |
| Neonate diagnosed with asphyxia | No | 157 | 238 | ** | ||
| Yes | 41 | 44 | 1.41(0.88-2.26) | 1.03(1.57-1.85) | 0.913 | |
| 1st minute APGAR score | 7-10 | 160 | 182 | ** | ||
| <7> | 38 | 100 | 0.43(0.28-0.66) | 0.57(0.34-0.98) | 0.042* | |
| Had neonate received KMC | Yes | 122 | 95 | 3.16(2.16-4.61) | 4.46(2.79-7.13) | 0.001* |
| No | 76 | 187 | ** | |||
Key: AOR: Adjusted odd ratio, COR: Crude odd ratio, **reference category, * statistically significant variables
Discussion
This study aimed to assess the factors affecting the timely initiation of breastfeeding among mothers. The present study showed that 41% (95% CI: 37.1%-45.6%) of respondents had practiced early initiation of breastfeeding. This study is consistent with studies conducted in Burkina Faso[12], Cameroon [13], and Ghana [14], which revealed 41%,40%,& 39.4%, respectively, commenced breastfeeding within a one-hour duration. However, this finding was lower than the WHO recommendation of 90% and previous studies conducted in Ethiopia [21], Tanzania [11], and Iraq [22]; which revealed that 75%, 83%, 70% of respondents had commenced early initiation of breastfeeding respectively. This discrepancy is due to variations in the provision of healthcare services, participants’ health literacy, study area, and period. However, the present findings are higher than those of studies conducted in Rwanda [23], and Saudi Arabia [24], which reported that only 20.5% & 11.4% of mothers of neonates initiated breastfeeding within one hour respectively. The possible reason for this discrepancy might be due to the variation in health care service provision and participants' health literacy.
According to this study; Antenatal care was significantly associated with timely initiation of breastfeeding. Respondents who had ANC visits during their pregnancy were six times more likely to practice early breastfeeding initiation than those who haven't ANC follow-up during pregnancy. This finding is consistent with studies of Ethiopian DHS reports [25], A Meta-analysis of observational studies [26], Nepal [27],and Turkey [28]. A possible reason might be that women with a history of ANC follow-up during their pregnancy; might have a better chance of being aware of breastfeeding counseling provided by healthcare providers. The present study’s findings showed that the mode of delivery was also significantly associated with the timely initiation of breastfeeding. Women who gave birth through cesarean section were initiate breast feeding lately (AOR= 0.37, 95% CI 0.19-0.69) than women gave birth via spontaneous vagina delivery. This finding is similar to those of the, 2016 Ethiopian Demographic and Health Survey [10], Ohio-US [29], George Mason University, USA[30], Pakistan [31], A systematic literature review conducted in Brazil [32], and A meta-analysis of Demographic Health Surveys across 31 countries [24]. The possible reason may be due to the nature of the procedures which may take a long time; mothers who had undergone caesarian sections usually feel discomfort and interfere to apply timely initiation of breastfeeding.
Furthermore, neonates with Apgar scores -Less than 7 were 42% less likely to practice early breastfeeding initiation than neonates with an Apgar score of 7 to 10. This finding is consistent with a study conducted in Ghana(14), which revealed that a low Apgar score was associated with the time to initiation of breastfeeding. This might be because neonates who required additional breathing support or additional support faced difficulty in timely breastfeeding initiation [33]. The current study findings revealed that utilization of kangaroo mother care was statistically associated with timely initiation of breastfeeding; neonates who received kangaroo mother care were four times more likely to have early breastfeeding initiation than their counterparts. This finding is consistent with studies including; a meta-analysis of published studies from January 2000 to June 30, 2018 [34], longitudinal studies in Sweden [35], Bangladesh [36], India [37], and China [38]. One possible reason for this is that kangaroo mother care practices enhance skin-to-skin contact and promote breastfeeding.
Strength and limitation of the study
As a strength this study involved all public hospitals found in the Southwest region and had a high participant response rate. As a limitation, this study didn’t address health care provider's perspectives on the early initiation of breastfeeding. In addition, due to its cross-sectional study design nature, this study also didn’t show the cause and effect of early initiation of breastfeeding.
Conclusion
Timely initiation of breastfeeding in the current study was lower than the World Health Organization recommendations. Histories of ANC visits, low 1st minute Apgar score, provision of KMC, and delivery via cesarean section were significantly associated with timely initiation of breastfeeding. Hence, health professionals working in the delivery ward should be aware of those factors to improve the proportion of early initiation of breastfeeding. Additionally, all concerned bodies should pay attention to enhancing and promoting the early initiation of breastfeeding.
Abbreviation
EIBF: Early initiation of breastfeeding,
EDHS: Ethiopian Demographic Health Survey;
COR: Crude Odd ratio;
AOR: Adjusted Odd ratio;
ANC: Antenatal care;
WHO: World Health Organization;
KMC: Kangaroo mother care
Declarations
Consent to Participate
Both verbal and written informed consent was provided for study participants with information regarding the purpose, objective, procedures, potential risks and benefits of the study, and the right to withdraw from the study. They were also assured of strict confidentiality concerning any information obtained from them.
Data Availability
The data is available at the corresponding author upon reasonable request.
Author contributions
YD: Prepared the manuscript, reviewed, and edited a manuscript, statistical analysis, and interpretation. BF: writing the original draft, designing the study, preparing the manuscript, reviewing, and editing the manuscript. TB: designed the study, prepared the manuscript, reviewed, edited a manuscript, and critically reviewed the article. AY: designed the study, prepared the manuscript, reviewed, and edited the manuscript. All authors’ contributions to conception and design, acquisition of data, analysis, and interpretation of data, drafting of the article, and revising it critically.
Consent for publication
Not applicable.
Funding
There is no funding organization for this study.
References
- Hanson LÅ, Korotkova M. (2002). The role of breastfeeding in prevention of neonatal infection. Semin Neonatol Elsevier, 7(4):275-281.
Publisher | Google Scholor - WHO and U. (2018). Early initiation of breastfeeding: The best start for every newborn. New York.
Publisher | Google Scholor - Esteves TMB, Daumas RP, de Oliveira MIC, de Andrade CA de F, Leite IC. (2014). Factors associated to breastfeeding in the first hour of life: Systematic review. Rev Saude Publica, 48(4):697-708.
Publisher | Google Scholor - E Lawn, S. Cousens JZ. (2005). MDGs and newborn babies. Lancet, 65:891-900.
Publisher | Google Scholor - Layuk N, Wardihan A, Asad S. (2021). Early initiation of breastfeeding and gut microbiota of neonates. A literature review ଝ. Med Clínica Práctica, 4:100222.
Publisher | Google Scholor - Al Sabati SY, Mousa O. (2019). Effect of Early Initiation of Breastfeeding on the Uterine Consistency and the Amount of Vaginal Blood Loss during Early Postpartum Period. Nurs Prim Care, 3(3):2-7.
Publisher | Google Scholor - Berkat S, Sutan R. (2014). The Effect of Early Initiation of Breastfeeding on Neonatal Mortality among Low Birth Weight in Aceh Province, Indonesia: An Unmatched Case Control Study. Adv Epidemiol, 1-7.
Publisher | Google Scholor - Oot L, Sethuraman K, Ross J, Sommerfelt AE. (2018). of Late Breastfeeding Initiation on Neonatal Mortality: A Model in PROFILES for Country-Level Advocacy.
Publisher | Google Scholor - Takahashi K, Ganchimeg T, Ota E, Vogel JP, Souza JP, Laopaiboon M, et al. (2017). Prevalence of early initiation of breastfeeding and determinants of delayed initiation of breastfeeding: Secondary analysis of the WHO Global Survey. Sci Rep, 1-10.
Publisher | Google Scholor - Gedefaw G, Goedert MH, Abebe E, Demis A. (2020). Effect of cesarean section on initiation of breast feeding: Findings from 2016 Ethiopian Demographic and Health Survey. PLoS One, 15(12):1-13.
Publisher | Google Scholor - Lyellu HY, Hussein TH, Wandel M, Stray-Pedersen B, Mgongo M, Msuya SE. (2020). Prevalence and factors associated with early initiation of breastfeeding among women in Moshi municipal, northern Tanzania. BMC Pregnancy Childbirth, 20(1):1-10.
Publisher | Google Scholor - Savadogo LGB, Ilboudo B, Meda C, Kinda M. (2018). Early Initiation of Breastfeeding and Its Association in Rural Areas of Burkina Faso. Open J Epidemiol, 8(2):5466.
Publisher | Google Scholor - Nguefack F, Ngwanou DH, Moyo GPK, Ejake L, Mah EM, Wafeu G, et al. (2020). Reasons for Delayed Breastfeeding Initiation among Newly Delivered Women in Two First-Category Hospitals in Yaoundé Cameroon. Open J Pediatr, 10(03):474-85.
Publisher | Google Scholor - Boakye-Yiadom AP, Nguah SB, Ameyaw E, Enimil A, Wobil PNL, Plange-Rhule G. (2021). Timing of initiation of breastfeeding and its determinants at a tertiary hospital in Ghana: a cross-sectional study. BMC Pregnancy Childbirth, 21(1):1-9.
Publisher | Google Scholor - Alzaheb RA. (2017). A Review of the Factors Associated with the Timely Initiation of Breastfeeding and Exclusive Breastfeeding in the Middle East. Clin Med Insights Pediatr.
Publisher | Google Scholor - Moment CTHE, Initiation E, Breastfeeding OF. CAPTURE.
Publisher | Google Scholor - Alzaheb RA. (2016). Factors associated with the initiation of breastfeeding within the first 48 hours of life in Tabuk, Saudi Arabia. Int Breastfeed J, 11(1):1-6.
Publisher | Google Scholor - Paramashanti BA, Hadi H, Alit Gunawan IM. (2016). Timely initiation of breastfeeding is associated with the practice of exclusive breastfeeding in Indonesia. Asia Pac J Clin Nutr, 52-56.
Publisher | Google Scholor - WHO and, UNICEF. (2018). Capture the Moment-Early initiation of breastfeeding: The best start for every newborn. New York.
Publisher | Google Scholor - World Health Organization (WHO). (2012). The global action report on preterm birth.
Publisher | Google Scholor - Salasibew MM, Filteau S, Marchant T. (2014). Measurement of breastfeeding initiation: Ethiopian mothers’ perception about survey questions assessing early initiation of breastfeeding. Int Breastfeed J, 9(1):1-8.
Publisher | Google Scholor - Mayasah A. S, Alaa A. S. (2020). Factors Affecting Initiation of Breast Feeding: A Cross Section Study. J Fam Med Dis Prev, 6(4):6-11.
Publisher | Google Scholor - Mukashyaka J, Mukarubayiza R, Mukarubayiza R, Habumugisha E, Sunday F-X, Muganwa K, et al. (2020). Early Initiation of Breastfeeding Among Postpartum Mothers at Two Rwandan Hospitals. Rwanda J Med Heal Sci, 3(2):181-192.
Publisher | Google Scholor - Analysis CAT, Mallick L, Wang W, Farid S. (2020). Initiation of Breastfeeding in Low- and Middle-Income. Glob Heal Sci Pract, 9(2):308-317.
Publisher | Google Scholor - Ahmed KY, Page A, Arora A, Ogbo FA. (2019). Trends and determinants of early initiation of breastfeeding and exclusive breastfeeding in Ethiopia from 2000 to 2016. Int Breastfeed J, 9:1-14.
Publisher | Google Scholor - Habtewold TD, Sharew NT, Alemu SM. (2019). Evidence on the effect of gender of newborn, antenatal care and postnatal care on breastfeeding practices in Ethiopia: A meta-Analysis andmeta-regression analysis of observational studies. BMJ Open, 9(5).
Publisher | Google Scholor - Ghimire U. (2019). The effect of maternal health service utilization in early initiation of breastfeeding among Nepalese mothers. Int Breastfeed J,14(1):1-8.
Publisher | Google Scholor - Göl İ. (2018). Antenatal Care and Breastfeeding. Turkish J Fam Med Prim Care,12(2):102-108.
Publisher | Google Scholor - Study AP, Regan J, Thompson A, Defranco E. (2013). The Influence of Mode of Delivery on Breastfeeding Initiation in Women with a Prior Cesarean Delivery. Breastfeed Med, 8(2):26-31.
Publisher | Google Scholor - Birth C. (2017). Mode of delivery and breastfeeding practices. Int J Pregnancy Child Birth, 2(6):167-172.
Publisher | Google Scholor - Saeed G, Fakhar S. (2011). The Effect of Modes of Delivery on Infants’ Feeding Practices. Iran J Med Sci, 36(2):128-132.
Publisher | Google Scholor - Maria T, Esteves B, Daumas RP, Leite IC. (2014). Factors associated to breastfeeding in the first hour of life: systematic review Fatores associados à amamentação na primeira hora de vida: revisão sistemática. Rev Saúde Pública, 48(4):697-708.
Publisher | Google Scholor - KC A, KC A, Lawn JE, Zhou H, Ewald U, Gurung R, et al. (2020). Not crying after birth as a predictor of not breathing. Pediatrics,145(6).
Publisher | Google Scholor - Mekonnen AG, Yehualashet SS, Bayleyegn AD. (2019). The effects of kangaroo mother care on the time to breastfeeding initiation among preterm and LBW infants: a meta-analysis of published studies. Int Breastfeed J, 14(12):12-17.
Publisher | Google Scholor - Ewald U, Wallin L. (2011). Positive Effect of Kangaroo Mother Care on Long-Term Breastfeeding in. JOGNN, 40(2):190-197.
Publisher | Google Scholor - Hoque MM. (2017). Effectiveness of KMC on Success of Breast feeding in Preterm Low Birth Weight Neonate. Acad J Pediatr Neonatol, 3(4):70-73.
Publisher | Google Scholor - Heidarzadeh M, Hosseini MB, Ershadmanesh M, Gholamitabar Tabari M, Khazaee S. (2013). The Effect of Kangaroo mother care (KMC) on breast feeding at the time of NICU discharge. Iran Red Crescent Med J, 15(4):302-306.
Publisher | Google Scholor - Zhang B, Duan Z, Zhao Y, Williams S, Wall S, Huang L, et al. (2020). Intermittent kangaroo mother care and the practice of breastfeeding late preterm infants: results from four hospitals in different provinces of China. Int Breastfeed J, 5:1-9.
Publisher | Google Scholor