Research Article
Infertility in Women with Thyroid Pathology: Diagnosis and Tactics, Treatment
Candidate of medical sciences, Obstetrician-gynecologist, Medical Center "Harmony of Health, Ukraine.
*Corresponding Author: Beraia D.Yu, Candidate of medical sciences, Obstetrician-gynecologist, Medical Center
Citation: Beraia D.Yu. (2023). Infertility in women with Thyroid pathology: diagnosis and Tactics, Treatment, Clinical Obstetrics and Gynecology Research, BRS Publishers. 1(1); DOI: 10.59657/2992-9725.brs.23.004
Copyright: © 2023 Beraia D.Yu, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 21, 2023 | Accepted: March 15, 2023 | Published: March 20, 2023
Abstract
Aim: Reduction of the frequency of reproductive function disorders and gestational complications in women with thyroid pathology based on the study of new aspects of the pathogenesis of female infertility, as well as improvement and implementation of the algorithm of diagnostic and therapeutic and preventive measures.
Materials and Methods: We examined 667 women who were divided into the following blocks of research: a screening assessment of the state of the thyroid gland was carried out in 248 women with infertility (the main group) and in 40 fertile women who went to the clinic to choose a contraceptive method (the control group). Questionnaires were conducted in 103 women with infertility; assessment of reproductive function in women with thyroid pathology was carried out retrospectively in 125 patients with a confirmed diagnosis of diffuse toxic goiter and prospectively in 29 women of reproductive age with a confirmed diagnosis, disorders of the menstrual cycle and /or reproductive function; immunological parameters were evaluated in 103 women of reproductive age with tubo-peritoneal factor infertility, including 59 patients with antibodies to thyro peroxidase and/or antibodies to thyroglobulin and 44 patients without thyroid pathology. A dynamic assessment of thyroid function and the course of pregnancy was carried out in 55 pregnant women, divided into 5 groups depending on the initial functional state of the thyroid gland. The assessment of the features of the functioning of the hypothalamic-pituitary-thyroid system during pregnancy after assisted reproductive technologies on the background of ovarian hyperstimulation syndrome, it was carried out in 50 pregnant women without underlying pathology of the thyroid gland, including 30 pregnant women with a severe form of ovarian hyperstimulation syndrome (group 1), 27 pregnant women without signs of ovarian hyperstimulation syndrome (group 2, comparison group) and 14 women with spontaneous pregnancy (group 3).
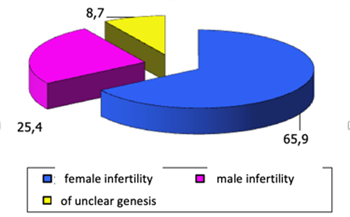
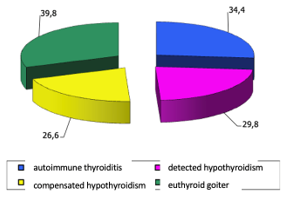
Result: Among women with various forms of thyroid pathology, 49.4% have primary infertility, 50.6% - secondary. Female infertility was diagnosed in 65.9% of patients, male infertility in 25.4%; unclear genesis - in 8.7% of cases. The frequency of thyroid pathology in women with infertility is 47.9%. A comparative evaluation of the results of thyroid screening in women with infertility and in fertile women showed that the prevalence of thyroid pathology in women with infertility was 3.8 times higher compared to fertile women (48% and 12.5%). In the structure of the pathology of the thyroid gland, the presence of antibodies to thyroperoxidase prevails, combined with echo signs of autoimmune thyroiditis 2.8 times more often in infertile women compared to fertile women (24% and 8.7%). The level of hypothyroidism is 9.4%, and thyrotoxicosis is only 0.6%, respectively. A comparative analysis of the causes of reproductive dysfunction in women with thyroid pathology showed that the leading place in the structure of infertility causes in women with autoimmune thyroiditis was external genital endometriosis (34.4%), with detected hypothyroidism - an endocrine factor of infertility (29.8%), with compensated hypothyroidism - external genital endometriosis (26.6%), with euthyroid goiter - tubal-peritoneal factor (39.8%).
Conclusion: The use of the algorithm improved by us in women with a history of infertility against the background of thyroid pathology allows to reduce the frequency of: reproductive losses from 19.1% to 6.7%; premature births from 20.3% to 6.7%; placental dysfunction from 39.4% to 13.3% of total perinatal pathology from 20.3% to 10.0%, respectively.
Keywords: infertility; thyroid pathology; clinical aspects; treatment tactics
Introduction
According to domestic and foreign researchers, the frequency of infertile marriage ranges from 10 to 20% (O.M. Yuzko et al., 2020). The problem of the relationship between reproductive function disorders and thyroid pathology is actively discussed in the scientific literature (L.M. Semenyuk 2021). On the one hand, this is due to the high prevalence of infertility in marriage (up to 15-17%), which, despite modern achievements in the field of human reproduction, has no tendency to decrease (S.I. Zhuk 2020; V.V. Kaminsky and sang., 2021). On the other hand, thyroid diseases occupy the first place in the structure of endocrine pathology in women of reproductive age (M.D. Tronko et al., 2019).
Today, the role of thyroid dysfunction is widely discussed, which directly negatively affects the quality of the pre-implantation embryo, the implantation process, as well as the differentiation and function of the trophoblast, which leads to infertility, adverse results of assisted reproductive technology (ART) programs, and early reproductive losses (L.V. Suslikova and colleagues, 2020).
The improvement of DRT programs made it possible to increase the frequency of pregnancy from 30 to 80% in cases of infertility of various genesis. The course of the early stages of induced pregnancy (IP) occurs against the background of high non-physiological concentrations of steroid hormones produced by hyperstimulated ovaries and accompanied by an increased frequency of complications (ovarian hyperstimulation syndrome, multiple pregnancies, early reproductive losses). Pronounced hormonal load can adversely affect thyroid function, especially in women with thyroid pathology. However, the literature does not reflect the peculiarities of the functioning of the thyroid gland in the early stages of IP, depending on the initial state of the functional state of the thyroid gland, the degree of ovarian hyperstimulation, and the number of fetuses. There is no developed algorithm for the management of early periods of IP taking into account the functional state of the thyroid gland.
It is relevant to study the frequency and structure of thyroid disorders in women with infertility, the peculiarities of the implementation of reproductive function in patients with verified thyroid pathology, the assessment of the effect of thyroid gland on the receptivity of the endometrium and embryological indicators in the DRT program, the identification of the features of the functional state of the thyroid gland against the background of the induced cycle and induced (in including multiple) pregnancy, taking into account the degree of hyperstimulation of the ovaries, as well as the peculiarities of the course of induced pregnancy in various variants of thyroid pathology.
The aim of the research: reduction of the frequency of reproductive function disorders and gestational complications in women with thyroid pathology based on the study of new aspects of the pathogenesis of female infertility, as well as improvement and implementation of the algorithm of diagnostic and therapeutic and preventive measures.
The following tasks were defined to realize the set goal
- To determine the frequency and structure of reproductive function disorders in women with thyroid pathology.
- To determine the level and leading variants of thyroid pathology in women with infertility.
- To present the results of a comparative analysis of the causes of reproductive function disorders in women with thyroid pathology.
- To find out the state of the ovarian reserve and the level of antibodies to phospholipids, cofactors, antiovarian antibodies and antibodies to human chorionic gonadotropin in women without and with thyroid pathology.
- To assess the functional state of the endometrium and impaired receptivity in women with infertility against the background of thyroid pathology. Show the results of qualitative analysis of follicular fluid in women with infertility against the background of thyroid pathology.
- To study the effect on the functional state of the thyroid gland of stimulation of superovulation in in vitro fertilization programs in women with thyroid pathology.
- To present a comparative analysis of the frequency of complications of the first trimester of pregnancy in women with thyroid pathology.
- To improve and evaluate the effectiveness of the diagnostic and treatment-prophylactic algorithm during pregnancy in women with a history of infertility against the background of thyroid pathology.
Materials and methods
We examined 667 women, who were divided into the following blocks of research: a screening assessment of the state of the thyroid gland was carried out in 248 women with infertility (the main group) and in 40 fertile women who went to the clinic to choose a method of contraception (the control group). The selection of patients was carried out by an open cohort method as the patients with infertility applied to the Department of Preservation and Restoration of Reproductive Function. The survey was conducted in 103 women with infertility; assessment of reproductive function in women with thyroid pathology was carried out retrospectively in 125 patients with a confirmed diagnosis of diffuse toxic goiter and prospectively in 29 women of reproductive age with a confirmed diagnosis, disorders of the menstrual cycle and/or reproductive function; immunological parameters were evaluated in 103 women of reproductive age with tubo-peritoneal factor infertility, including 59 patients with antibodies to thyroperoxidase and/or antibodies to thyroglobulin and 44 patients without thyroid pathology.
Dynamic assessment of thyroid function and the course of pregnancy was carried out in 55 pregnant women (including 35 women with pregnancy after assisted reproductive technologies and 20 patients with spontaneous pregnancy), divided into 5 groups depending on the initial functional state of the thyroid gland: 13 pregnant women after assisted reproductive technologies without thyroid gland pathology (group I), 10 pregnant women after assisted reproductive technologies carriers of thyroperoxidase antibodies (group II), 13 pregnant women after assisted reproductive technologies with compensated hypothyroidism (group III), 10 women with spontaneous pregnancy without thyroid gland pathology (group IV ), 9 women with spontaneous pregnancy and compensated hypothyroidism (group V).
The assessment of the features of the functioning of the hypothalamic-pituitary-thyroid system during pregnancy after assisted reproductive technologies against the background of ovarian hyperstimulation syndrome was carried out in 50 pregnant women without primary thyroid pathology, including 30 pregnant women with a severe form of ovarian hyperstimulation syndrome (group 1), 27 pregnant women without signs of ovarian hyperstimulation syndrome (group 2, comparison group) and 14 women with spontaneous pregnancy (group 3).
Results
The results of the research show that 49.4% of women with various forms of thyroid pathology have primary infertility, 50.6% have secondary infertility. Female infertility was diagnosed in 65.9% of patients, male infertility in 25.4%; unclear genesis - in 8.7% of cases. In the structure of the causes of female infertility, the tube-peritoneal factor prevails (37%); external genital endometriosis - 36.4% and endocrine factor - in 23.2%.
A combination of various infertility factors was noted in 23.8% of women.
Figure 1: “Causes of infertility”
The frequency of thyroid pathology in women with infertility is 47.9%. A comparative evaluation of the results of thyroid screening in women with infertility and in fertile women showed that the prevalence of thyroid pathology in women with infertility was 3.8 times higher compared to fertile women (48% and 12.5%).
In the structure of the pathology of the thyroid gland, the carrier of antibodies to thyroperoxidase prevails, combined with echo symptoms of autoimmune thyroiditis (diffuse heterogeneity and reduced echogenicity of the tissue), which is 2.8 times more common in infertile women compared to fertile women (24% and 8.7%). The level of hypothyroidism is 9.4%, and thyrotoxicosis is only 0.6%, respectively. (slide 16) A comparative analysis of the causes of reproductive dysfunction in women with thyroid pathology showed that the leading place in the structure of infertility causes in women with autoimmune thyroiditis was external genital endometriosis (34.4%), with detected hypothyroidism - an endocrine factor of infertility (29, 8%), with compensated hypothyroidism - external genital endometriosis (26.6%), with euthyroid goiter - tubal-peritoneal factor (39.8%).
Figure 2: “Structure of infertility causes in women with autoimmune thyroiditis”
In women with infertility on the background of thyroid pathology, there is a violation of the ovarian reserve in the form of a significant decrease in the average concentrations of anti-Mullerian hormone and an increase in the average levels of follicle-stimulating hormone, as well as a significantly increased level of antibodies to phospholipids and cofactors (cardiolipin, 2-glycoprotein-1, phosphatidylserine ), antiovarian antibodies and antibodies to human chorionic gonadotropin compared to women without thyroid pathology and healthy fertile women.
When assessing the functional state of the endometrium in women with infertility against the background of thyroid pathology, inflammatory changes were established with increased expression of markers of plasma cells CD138, macrophages CD68 and natural killers CD56, as well as increased processes of cell proliferation in the stroma and apoptosis in the epithelium. It should be noted that there was no correlation between the level of expression of all markers in the endometrium and the titer of antithyroid antibodies in blood serum, and autoantibodies were considered markers of generalized autoimmune dysfunction.
In addition, a significant violation of receptivity was noted, as evidenced by a more than 3-fold decrease in the expression of LIF in the endometrium, which allows us to consider the presence of antibodies to thyroperoxidase as a prognostic marker of implantation disorders. The results of the qualitative analysis of follicular fluid in women with infertility on the background of thyroid pathology indicate that the level of sFas was directly correlated with the number and percentage of high-quality embryos (g=0.5 and g=0.7, respectively) obtained in the in vitro fertilization program, a decrease in the level of sFas led to an increase in the number of embryos of poor quality and deterioration of embryological indicators, an increase in the level of sFas-L led to a sharp deterioration of embryological indicators. The level of antibodies to thyroperoxidase, sFas and sFas-L in follicular fluid can serve as predictors of adverse outcomes due to the influence on the number and quality of received oocytes and embryos.
Stimulation of superovulation in extracorporeal fertilization programs in women with thyroid pathology leads to hyperstimulation of the thyroid gland in the early stages of induced pregnancy compared to the initial one by 1.5-2 times, but these changes in women without thyroid pathology are transient. With compensated hypothyroidism, they indicate the need to increase the dose of L-thyroxine earlier than with spontaneous pregnancy, and with the presence of antibodies to thyroperoxidase, they lead to relative hypothyroxinemia due to a decrease in the adaptive capabilities of the thyroid gland affected by the autoimmune process.
Transient gestational hyperthyroidism, combined with early toxicosis of pregnant women, is observed in multiple induced pregnancies 3.5-3.8 times more often than in singleton induced and spontaneous pregnancies, and directly depends on the level of human chorionic gonadotropin. A third of pregnant women (33.3%) without thyroid pathology with a severe form of ovarian hyperstimulation syndrome develop subclinical hypothyroidism caused by supraphysiological concentrations of estradiol. In women carrying antibodies to thyroperoxidase, a significant increase in the frequency of early toxicosis of pregnant women, the threat of abortion, detachment and hypoplasia of the chorion, and early reproductive losses was noted compared to patients without thyroid gland pathology.
A comparative analysis of the frequency of complications of the first trimester of pregnancy in women with thyroid pathology compared to healthy women showed a significantly higher frequency: early toxicosis of pregnant women by 1.9 times (12.5% and 6.7%), threatened termination of pregnancy by 1.5 times (42.2% and 28.9%), chorionic detachment 1.7 times (18.7% and 11.1%), chorionic hypoplasia 2.1 times (14.1% and 6.7%), and antiphospholipid antibodies (20.3% and 4.4%) and antibodies to human chorionic gonadotropin (15.6% and 6.7%) are also found.
All women suffering from infertility and, above all, patients planning to restore their reproductive function with the help of assisted reproductive technologies, we evaluated the function of the thyroid gland (thyroid-stimulating hormone, free fractions of thyroxine) and antibodies to thyroperoxidase at the initial stage of the examination for infertility.
When pathology was detected, timely correction of violations was carried out together with the endocrinologist at the stage of preparation for programs of assisted reproductive technologies. Special attention was paid to the mandatory assessment of the level of antibodies to thyroperoxidase in women with infertility, which allowed us to identify a group of women at risk of low effectiveness of infertility treatment, to predict the development of hypothyroxinemia or hypothyroidism in the early stages of pregnancy, as well as to identify a group of women at risk of developing postpartum thyroiditis.
All women at the stage of planning methods of assisted reproductive technologies should be prescribed individual iodine prophylaxis in the form of precisely dosed preparations of potassium iodide (iodomarin or iodine balance 250 mcg per day) or vitamin and mineral complexes for pregnant women containing iodine (vitrum prenatal forte) combined with potassium preparations iodide Individual iodine prophylaxis was carried out throughout pregnancy and the period of breastfeeding.
Women with isolated carriers of antibodies to thyroperoxidase without impaired thyroid function should be recommended to carry out an in vitro fertilization program at a TSH level of less than 2.5 mU/l and to monitor the levels of thyroid-stimulating hormone and free fractions of thyroxine every 6-8 weeks throughout the entire gestation period.
In women with manifest hypothyroidism, we recommend the use of L-T4 replacement therapy (L-thyroxine, euthyrox) at the rate of 1.6 μg/kg of body weight. Programs of assisted reproductive technologies should be carried out only on the condition that stable compensation of hypothyroidism is achieved (the level of thyroid-stimulating hormone is less than 2.5 mU/l). For women with initially compensated hypothyroidism and a thyroid-stimulating hormone level of less than 2.5 mU/l, in whom it is possible to predict the development of ovarian hyperstimulation syndrome in assisted reproductive technology programs, control the levels of thyroid-stimulating hormone and the free fraction of thyroxine every 6-8 weeks and, if necessary, increased the dose of L-thyroxine (approximately 50 μg/day).
Thyrotoxicosis to a lesser extent than hypothyroidism leads to a decrease in fertility in women. In women with detected thyrotoxicosis, the choice of the optimal method of treatment (thyrostatic therapy, surgical treatment, radioactive iodine therapy) was carried out together with an endocrinologist, taking into account the age and state of the ovarian reserve.
The tactics of managing an induced pregnancy in women with thyroid pathology depends on the functional state of the thyroid gland, the causes of female infertility, endocrine and immune status, changes in the level of thyroid hormones and the functional state of the fetoplacental complex, which requires the development and use of an individualized pregnancy management plan and delivery method.
Conclusion
The use of the improved algorithm in women with a history of infertility on the background of thyroid pathology allows to reduce the frequency of reproductive losses from 19.1% to 6.7%; premature births from 20.3% to 6.7%; placental dysfunction from 39.4% to 13.3% and total perinatal pathology from 20.3% to 10.0%, respectively.
References
- Bucci I, Giuliani C, Di Dalmazi G, Formoso G, Napolitano G. (2022). Thyroid Autoimmunity in Female Infertility and Assisted Reproductive Technology Outcome. Front Endocrinol (Lausanne), 26(13):768363.
Publisher | Google Scholor - Dosiou C. Thyroid and Fertility.(2020). Recent Advances. Thyroid, 30(4):479-486.
Publisher | Google Scholor - Unuane D, Velkeniers B. (2020). Impact of thyroid disease on fertility and assisted conception. Best Pract Res Clin Endocrinol Metab, 34(4):101378.
Publisher | Google Scholor - Khizroeva J, Nalli C, Bitsadze V, Lojacono A, Zatti S, Andreoli L, Tincani A, Shoenfeld Y, Makatsariya A. (2020). Infertility in women with systemic autoimmune diseases. Best Pract Res Clin Endocrinol Metab, 33(6):101369.
Publisher | Google Scholor - Korevaar TIM, Mínguez-Alarcón L, Messerlian C, de Poortere RA, Williams PL, Broeren MA, Hauser R, Souter IC. (2018). Association of Thyroid Function and Autoimmunity with Ovarian Reserve in Women Seeking Infertility Care. Thyroid. 28(10):1349-1358.
Publisher | Google Scholor - Koyyada A, Orsu P. (2020). Role of hypothyroidism and associated pathways in pregnancy and infertility: Clinical insights. Tzu Chi Med J, 32(4):312-317.
Publisher | Google Scholor - Kucukler FK, Gorkem U, Simsek Y, Kocabas R, Guler S. (2018). Evaluation of ovarian reserve in women with overt or subclinical hypothyroidism. Arch Med Sci, 14(3):521-526.
Publisher | Google Scholor - Maraka S, Singh Ospina NM, Mastorakos G, O'Keeffe DT. (2018). Subclinical Hypothyroidism in Women Planning Conception and During Pregnancy: Who Should Be Treated and How? J Endocr Soc, 2(6):533-546.
Publisher | Google Scholor - Mazzilli R, Medenica S, Di Tommaso AM, Fabozzi G, Zamponi V, Cimadomo D, Rienzi L, Ubaldi FM, Watanabe M, Faggiano A, La Vignera S, Defeudis G. (2022). The role of thyroid function in female and male infertility: a narrative review. J Endocrinol Invest.
Publisher | Google Scholor - Medenica S, Abazovic D, Ljubić A, Vukovic J, Begovic A, Cucinella G, Zaami S, Gullo G. (2022). The Role of Cell and Gene Therapies in the Treatment of Infertility in Patients with Thyroid Autoimmunity. Int J Endocrinol.
Publisher | Google Scholor - Orouji Jokar T, Fourman LT, Lee H, Mentzinger K, Fazeli PK. (2018). Higher TSH Levels Within the Normal Range Are Associated With Unexplained Infertility. J Clin Endocrinol Metab, 103(2):632-639.
Publisher | Google Scholor - Poppe K. (2021). MANAGEMENT OF ENDOCRINE DISEASE: Thyroid and female infertility: more questions than answers?! Eur J Endocrinol, 184(4):123-135.
Publisher | Google Scholor - Rao M, Wang H, Zhao S, Liu J, Wen Y, Wu Z, Yang Z, Su C, Su Z, Wang K, Tang L. (2020). Subclinical Hypothyroidism Is Associated with Lower Ovarian Reserve in Women Aged 35 Years or Older. Thyroid, 30(1):95-105.
Publisher | Google Scholor - Ren B, Zhu Y. (2022). A New Perspective on Thyroid Hormones: Crosstalk with Reproductive Hormones in Females. Int J Mol Sci, 23(5):2708.
Publisher | Google Scholor - Samsami A, Ghasmpour L, Moradi Alamdarloo S, Davoodi S, Rahmati J, Karimian A, Tavasoli M. (2020). Women with Autoimmune Thyroiditis have Lower Reproductive Life Span or Not? A Cross- Sectional Study. Int J Community Based Nurs Midwifery, 8(4):305-310.
Publisher | Google Scholor - Unuane D, Velkeniers B. (2020). Impact of thyroid disease on fertility and assisted conception. Best Pract Res Clin Endocrinol Metab, 34(4):101378.
Publisher | Google Scholor - Vannucchi G, Persani L, Fugazzola L. (2022). Thyroid pathology and female fertility: Myth or reality? Ann Endocrinol (Paris), 83(3):168-171.
Publisher | Google Scholor - Wadhwa L, Marghret KM, Arora S. (2020). Evaluation of Reproductive Outcome in Infertile Hypothyroid Women on Thyroxine Therapy. J Hum Reprod Sci,13(4):272-276.
Publisher | Google Scholor - Zhu Q, Xu QH, Xie T, Wang LL, Liu H, Muyayalo KP, Huang XB, Zhao SJ, Liao AH. (2021). Recent insights into the impact of immune dysfunction on reproduction in autoimmune thyroiditis. Clin Immunol.
Publisher | Google Scholor - Kim DJ, Seok SH, Baek MW, Lee HY, Juhn JH, Lee S, Yun M, Park JH. (2020). Highly expressed recombinant human follicle-stimulating hormone from Chinese hamster ovary cells grown in serum-free medium and its effect on induction of folliculogenesis and ovulation. Fertil Steril, 93(8):2652-2660.
Publisher | Google Scholor - Berger E, Chabloz P, Quay N, Sann A, Walton S, Germond M, Birkhauser M. (2019). An open, randomized, group‐comparative bi‐centre study comparing recombinant FSH Follitropinum beta 150 IU and highly purified urinary FSH 225 IU as a fixed dose regimen in IVF/ICSI treatment. Human Reproduction, 14(1):61‐62.
Publisher | Google Scholor - Beall SA, DeCherney A. (2019). History and challenges surrounding ovarian stimulation in the treatment of infertility. Fertil Steril, 97(4):785-801.
Publisher | Google Scholor - Youssef MA, Al-Inany HG, Aboulghar M, Mansour R, Abou-Setta AM. (2021). Recombinant versus urinary human chorionic gonadotrophin for final oocyte maturation triggering in IVF and ICSI cycles. Cochrane Database Syst Rev.
Publisher | Google Scholor - A.P. Ferraretti, A. La Marca, B.C.J.M. Fauser Hum Reprod. (2011). ESHRE consensus on the definition of ―poor response‖ to ovarian stimulation for in vitrofertilization: the Bologna criteria, 26:(16).16-162.
Publisher | Google Scholor - Thyroid dysfunction in infertile women S.G. Perminova Federal Research Center of Obstetrics, Gynecology, and Perinatology named after V.I.Kulakov Ministry of Health and Social Development of Russia, Moscow.
Publisher | Google Scholor - Bostanjyan L.L. (2005). Influence of superovulation stimulation on the functional state of the thyroid system in patients of the IVF and ET program: Dis. cand. medical Sciences. M.
Publisher | Google Scholor