Research Article
Implementing A Mixed-Gender Ward Policy to Curtail Admission Cancelations and Enhance Occupancy Rates
- Dr. Abdulmajeed Al Shehah 1
- Mr. Ali M. Al Yasin 2*
- Dr. Ahmad Al Mousa 3
- Dr. Anas Al Shuhayeb 4
- Dr. Ali Al Zahrani 4
- Mr. Riyadh Al Ameer 5
- Mr. Ahmad Alomar 2
- Dr. Abdulaziz Al Dihan 4
- Dr. Haitham Badr 6
- Dr. Fahad Al Awfi
1Assistant Director General for Medical Operations, Security Forces Hospital Program, Riyadh, Saudi Arabia.
2General Nursing Administration, Security Forces Hospital Program, Riyadh, Saudi Arabia.
3Assistant Director General for Medical Affairs, Security Forces Hospital Program, Riyadh, Saudi Arabia.
4General Medical Administration, Security Forces Hospital Program, Riyadh, Saudi Arabia.
5General Administration for patient services affairs and eligibility, Security Forces Hospital Program, Riyadh, Saudi Arabia.
6General Administration of Quality, Security Forces Hospital Program, Riyadh, Saudi Arabia.
7General Administration of Academic Affaires & Health Education, Security Forces Hospital Program, Riyadh, Saudi Arabia.
*Corresponding Author: Ali M. Al Yasin, General Nursing Administration, Security Forces Hospital Program, Riyadh, Saudi Arabia.
Citation: Abdulmajeed A. Shehah, A.M.A. Yasin, Ahmad A. Mousa, Anas A. Shuhayeb, Ali A. Zahrani, et al. (2024). Implementing A Mixed-Gender Ward Policy to Curtail Admission Cancelations and Enhance Occupancy Rates. Clinical Research and Reports, BioRes Scientia Publishers. 2(3):1-7. DOI: 10.59657/2995-6064.brs.23.022
Copyright: © 2024 Ali M. Al Yasin, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 18, 2024 | Accepted: February 05, 2024 | Published: February 15, 2024
Abstract
This paper analyzes the implementation of mixed-gender inpatient wards at Security Forces Hospital in Riyadh, KSA, between 2018 and 2023. Historically, hospitals separate wards by gender, leading to operational issues, including appointment cancelations and low bed occupancy rates. This hospital responded by assembling a team to analyze the problem and propose solutions. The key recommendation was to eliminate gender restrictions in wards to allow universal bed access while preserving patient privacy. A descriptive exploratory study design enabled an in-depth analysis of the factors causing admission cancelations and poor bed utilization. Comprehensive hospital data from 2018–2023 permitted an analysis of trends over several years. Implementation of mixed-gender wards eliminated patient cancelations from 1,094 in 2018 to zero and increased midnight bed utilization rates (61% to 79%), indicating enhanced operational efficiency. Crucial factors contributing to success included obtaining executive management support to drive organizational change, actively engaging patients to address cultural sensitivities, specialized training to equip staff for the new model of care, strategic input from nursing administration regarding workflows and staffing, and adapting security practices to ensure patient safety. Key lessons for hospital administrators considering similar initiatives include focusing on patient-centric care, optimizing operational efficiency through improved resource allocation, securing buy-in from organizational leadership, demonstrating cultural competence, investing in education and training for healthcare providers, engaging nursing administration strategically, and updating security protocols to match patient flow. In conclusion, this hospital’s experience illustrates how implementing mixed-gender inpatient units with a flexible, patient-focused approach can transform patient care delivery, augment bed utilization, streamline hospital operations, and nurture an inclusive, culturally sensitive healthcare environment. This multifaceted and collaborative strategy provides a model for healthcare facilities pursuing positive system-wide changes.
Keywords: mixed-gender ward; patient care delivery; patient-primarily based technique; bed utilization; streamlined clinic operations; nursing administration flow
Introduction
In the ever-changing realm of healthcare administration, enhancing bed distribution and occupancy levels is essential to guarantee efficient patient care and resource usage. This paper investigates the transformative process of a medical facility confronted by issues related to gender-specific inpatient wards, culminating in admission cancelations and an unsatisfactory occupancy rate. The institution’s strategy included the establishment of a multidisciplinary team assigned to review the matter and propose effective solutions. The crucial proposal, unanimously supported by the team, suggested eliminating gender distinction in inpatient wards and using universal bed accessibility while maintaining patient confidentiality and emotional comfort.
Background
Historically, hospitals have separated inpatient wards by gender to conform to societal norms and privacy considerations. This frequently caused operational difficulties, including admission cancelations and low occupancy rates. The case being examined had a substantial number of cancelations due to the unavailability of beds in gender-specific wards. This not only obstructed the swift provision of medical services but also added to dwindling occupancy rates throughout the institution.
The long-established policy of assigning beds based on gender, albeit justifiable, posed functional complications in directing patient progression and bed utilization effectively. Examples of beds lying vacant inside one gender’s ward, while another grappled with crowding, emphasized the necessity for an adaptable and patient-focused scheme. The shortcomings of the existing framework motivated the institution to commence an extensive probe into the root origins of the difficulty.
Importance of Addressing Bed Allocation and Occupancy Rates
Proper bed distribution and ideal occupancy rates are indispensable for healthcare facilities’ effective operation. In England’s National Health System, a recent disclosure of 13,178 incidents involving mixed-sex wards since last October underlines this issue’s seriousness [1]. With many patients subjected to stressful situations, it is crucial for hospitals to prioritize patient dignity and satisfaction.
The suspension of gender-specific accommodations during the pandemic revealed that the policy had been an obstacle in dealing with the growing demand for beds. Balancing occupancy levels and bed allocation while preserving privacy requires a meticulous focus on patient flow administration, capacity preparation, and targeted resource allotment [2]. The influence of these factors goes beyond logistical considerations, affecting patient results, resource exploitation, and comprehensive organizational efficacy. Regarding this case study, the inability to admit patients quickly due to gender-specific ward limitations led to adverse effects on the quality and timeliness of healthcare delivery.
Moreover, decreased occupancy rates result in poor resource utilization, adding to the institution’s financial encumbrance. Confronting challenges in bed allocation and occupancy rates can augment their capability to cater to a more extensive patient population, boost resource proficiency, and alleviate monetary restraints.
This study delves into the organization’s experiment to transition from conventional gender-specific ward allocation to an open and adjustable strategy. The sections below describe the methodology, notable findings, and the consequences of this endeavor and offer valuable insights for healthcare experts and supervisors aiming to optimize bed allocation and occupancy levels in their healthcare facilities.
Aim of the Study
The aim of this investigation is to analyze the effects of introducing a mixed-gender ward policy on decreasing admission cancelations and enhancing occupancy rates. Employing real-life experiences at the Security Forces Hospital in Riyadh as a case study, this inquiry will evaluate the strategies and describe the suggestions proposed by a team that examined this issue and its outcomes.
By examining the implementation process, results, and hindrances faced during the shift from a gender-focused bed allocation to a more efficient method, this research will furnish invaluable insights on the advantages and obstacles of creating mixed-gender wards. Moreover, it aims to clarify the essential steps healthcare providers must undertake to ensure a transition that positively benefits patients and hospitals without undermining cultural values and patient confidentiality.
This study also aspires to showcase an appropriate data analysis technique utilizing matrix tables that effectively convey the outcome measures of interest and the potential benefits of embracing innovative bed allocation approaches to optimize resource utilization in health care.
Methods
Study Design
The investigation applied a descriptive-exploratory study design for an exhaustive examination of the challenges associated with gender-specific bed allocations and the consequent impact of transitioning to a mixed-gender model [3]. This design facilitated an intensive exploration of factors contributing to admission cancelations and low occupancy rates, providing invaluable insights into patient care dynamics in the Security Forces Hospital in Riyadh.
The descriptive components of the study allowed a thorough examination of historical data, identifying patterns, tendencies, and relationships. The exploratory aspect allowed the researchers to delve deeper than surface-level observations, investigating the underlying causes of the identified issues. By merging these two methodologies, the investigation aimed to deliver a comprehensive understanding of the intricacies surrounding gender-specific bed allocations in hospital settings.
Sample and Sample Size
The inquiry used a comprehensive dataset extracted from hospital records in the period 2018 to 2023. This extensive timeframe permitted a meticulous examination of trends across numerous years, capturing fluctuations in-patient admissions, cancelations, and occupancy rates. Incorporating multiple years into the analysis provided a holistic perspective on the development of identified issues and the efficacy of implemented modifications.
The dataset encompassed a range of patient demographics, such as age, medical conditions, and gender. Integrating this broad array of information bolstered the inquiry’s ability to generalize findings to a larger patient population and draw significant conclusions concerning the impact of a mixed-gender approach.
Setting
The investigation took place in the context of the Security Forces Hospital in Riyadh, a prominent medical institution dedicated to offering all-encompassing healthcare services. The hospital’s diverse patient base and specialized medical treatments rendered it a suitable environment to study the consequences of shifting from gender-specific to mixed-gender inpatient wards.
The hospital’s commitment to optimizing patient care generated a favorable atmosphere for implementing and evaluating policy alterations related to bed allocation. The Riyadh setting contributed an essential aspect to the study, permitting consideration of cultural subtleties and regional intricacies that could affect patient preferences and beliefs.
Data analysis
To assess the applied modification’s effectiveness, a robust data analysis strategy was employed. A matrix table was designed incorporating critical metrics related to bed occupancy rates and admission cancelations. Comparing pre- and post-implementation information allowed a quantitative appraisal of the impact of mixed-gender methodology on hospital performance.
The data analysis included an intricate examination of multiple parameters, including gender-focused occupancy rates, cancelations, and overall usage of inpatient beds. Statistical techniques such as trend analysis and comparative statistics were leveraged to discern significant patterns and statistically meaningful disparities between the pre- and post-interventions phases.
Results
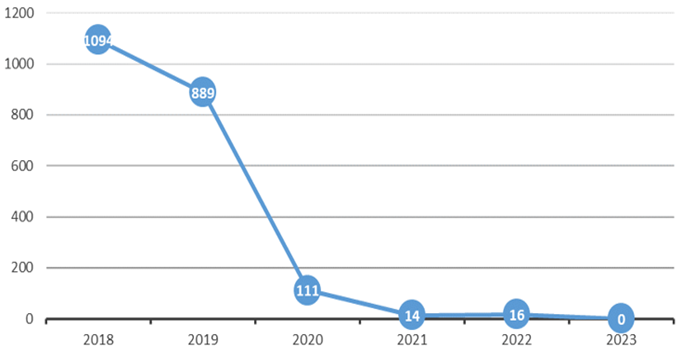
Implementing mixed-gender wards in the Security Forces Hospital in Riyadh resulted in a substantial decline in patient cancelations, transforming the landscape of inpatient care. A comprehensive analysis of annual data from 2018 to 2023 (Table 1) highlights the progressive improvement in patient cancelation numbers and midnight bed utilization percentages.
Table 1: Comparison of pre- and post-implementation metrics.
| Year | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 |
| Patient cancelations | 1094 | 889 | 111 | 14 | 16 | 0 |
| Midnight bed utilization (%) | 61 | 63 | 65 | 68 | 69 | 79 |
Patient cancelations and bed occupancy rate results
The charts below present data trends over time, showing the correlation between introducing mixed-gender wards, lowering patient cancelation figures, and raising usage rates for beds at midnight (Figure 1&2).
Figure 1: Bed Occupancy Rates.
Figure 2: Figure showing admission cancellations impacted by gender separation.
These charts illustrate the striking data progression over time, delineating the association between the establishment of mixed-gender wards, the minimization of patient cancelations, and the augmented use rates of beds at midnight. They underscore the transformational impact of this experiment on patient care processes, accentuating the favorable outcomes achieved through a calculated adaptation in assigning inpatient beds. As evidenced by the data, the decline in patient cancelations aligns with the hospital’s far-reaching objectives of augmenting service delivery, improving patient outcomes, and fine-tuning resource application.
The switch from gender-specific inpatient wards to mixed-gender wards played an essential role in significantly decreasing patient cancelations. This initiative’s success becomes apparent when examining the annual statistics, which demonstrate a consistent reduction in cancelation figures alongside a corresponding upsurge in usage rates of beds at midnight.
Enhanced Bed Availability
The termination of gender-focused ward restrictions resulted in a more adaptable and proficient bed allocation. Patients were no longer restricted to particular wards based on gender, permitting a dynamic apportioning of admissions across all accessible beds. This approach maximized resource use and resolved the bottleneck issue that previously led to cancelations.
Optimized Operational Efficiency
The mixed-gender ward model contributed to streamlining hospital operations. With the elimination of inflexible gender-centric classifications, patients could be accommodated in any available bed, thereby simplifying admission procedures. This not only reduced cancelations, but also enhanced total patient flow, contributing to the observed escalation in usage rates for beds at midnight.
Patient-Centric Approach
The transition to mixed-gender wards showcased a dedication to prioritizing patients’ needs. By placing bed accessibility above traditional gender-specific allocation, the hospital displayed adaptability to meet the diverse requirements of its patients. This approach resonated with patients and reflected an atmosphere of inclusivity while bolstering patient satisfaction.
Adoption of Best Practices
The project’s accomplishment stems from the hospital’s willingness to adjust and adopt optimal practices. Deciding to abandon conventional norms for a more progressive, patient-centered model necessitated a shift in mentality and organizational culture. The hospital’s adaptability, combined with effective change management strategies, facilitated the ongoing success of this initiative.
Discussion
Executive Management Support
Executive management backing was crucial in successfully initiating the mixed-gender inpatient ward project at the Security Forces Hospital in Riyadh. Approval from high-ranking executives provided the necessary momentum to traverse a complex organizational change. Their support was evident in resource allocation, alignment with institutional objectives, and incessant encouragement throughout the effort.
Executive leaders played an instrumental role in assembling the multidisciplinary team charged with analyzing and implementing modifications. Their engagement ensured that the project acquired the requisite focus and resources for success. This endorsement filtered down to middle management and frontline personnel, establishing a collaborative atmosphere devoted to shared organizational goals.
Additionally, executive backing was pivotal in obtaining widespread acceptance among staff members. Through active contextualization of the rationale for the change and emphasizing its strategic significance, executives formulated a cohesive vision transcending departmental limits. Aligning with top-tier leadership not only eased implementation processes, but also developed a sense of proprietorship and pride among hospital employees.
Patient Services
The success of the venture relied significantly on efficacious patient interactions. Patient viewpoints, preferences, and expectations were accurately anticipated throughout the shift to mixed-gender inpatient wards. Through a patient interview on daily round, a pivotal facet was ascertaining that patients were comfortable with the novel arrangement and retained a sense of safety, tackling apprehensions tied to seclusion and cultural sensitivities.
The hospital acknowledged the significance of transparent dialogue with patients and proactively pursued their input during the trial stage. This patient-focused approach not only boosted the palatability of the modification, but also added to a favorable depiction of the hospital as an institution receptive to patient necessities. Patient relations were preserved by supplying information regarding the undertaking, its aims, and the precautions employed to ensure a considerate and respectful setting for everyone.
Persistent involvement with patients and their families aided in pinpointing and tackling potential hurdles regarding the mixed-gender stratagem. This joint approach nurtured a sense of alliance between medical professionals and patients, underscoring the hospital’s commitment to patient-driven care.
Cultural Differences
Steering through cultural distinctions was an essential aspect of instituting the mixed-gender inpatient ward framework. The cultural milieu in Riyadh called for a nuanced tactic that respected conventional ethics and public expectations concerning gender segregation. Identifying these sensitivities, the hospital embarked upon an exhaustive cultural competency training curriculum for employees.
Cultural competency coaching aimed to heighten cognizance among healthcare suppliers about the diversity of patient origins and inclinations [4]. It dispensed insights into potential cultural factors that may sway patients’ perceptions of mixed-gender wards. This training was vital not just for the frontline workforce but also for leadership and clerical staff who interact with patients and their families.
Additionally, the hospital communicated with civic leaders, spiritual scholars, and cultural consultants to affirm that adjustments conformed to local customs and principles. This hands-on attitude not only displayed esteem for cultural variety, but also helped procure community backing for the project. The hospital presented itself as an institution that respects and integrates cultural considerations into its operations, nurturing a harmonious rapport with the neighborhood it serves.
The successful negotiation of executive administration assistance, patient relations, and cultural variances laid a sturdy base for the groundbreaking project. These constituents collectively aided the hospital’s ability to maneuver through the complexities of organizational transformation, certifying that the transition to mixed-gender inpatient wards was not merely effective but also harmonized with values and anticipations of both internal stakeholders and the community at large.
Change Management for Patient Services
Change administration for patient services was a crucial facet of the shift to mixed-gender inpatient wards at the Security Forces Hospital in Riyadh. Supervising alterations in a healthcare milieu entails not just amending physical edifices, but also remolding organizational ethos and functional processes. The incorporation of mixed-gender wards demanded an exhaustive change management plan that tackled the interests of both staff and patients.
The health center employed a methodical tactic to change management, entailing an array of premeditated and synchronized actions. This encompassed lucid communication of the reasoning behind the modification, its benefits for patient care, and each staff member’s involvement in its successful realization. Routine communication conduits, such as town hall congregations, bulletins, and training seminars, were harnessed to disseminate data and address any misapprehensions or anxieties [5]. Approximately a hundred and twenty individuals attended the workshop in the city hall congregation. Around 95 groups of workers underwent the education during the education consultation, which was scheduled for 8 hours for every 2 hours. The head of the training branch inside the facilitated become on top of things of the education session.
Furthermore, the change management blueprint underscored frontline staff participation in decision-making processes. This not only empowered workers but also cultivated a sense of ownership and accountability for the project’s success. Staff members were encouraged to communicate their outlooks, contribute ideas, and proactively partake in the adaptation procedure.
Continuous feedback circuits were implemented to keep track of the repercussions of the change and promptly tackle surfacing challenges. This methodology allowed for ongoing adjustments to the execution strategy anchored in the real-time occurrences and perspicacity of personnel on the front lines of patient care.
Security Changes in Practice to Ensure Patient Safety
To enhance the safety of patients in mixed-gender inpatient wards, the hospital implemented thoughtfully planned security modifications. These alterations involved transforming the physical setting, patient flow, and protective measures. The hospital committed resources to constructing private, safe areas within the wards, devising secluded rooms with appropriate security features to ensure patient privacy and well-being.
Conforming to the revamped model, security protocols underwent adjustments, tailoring access regulations to preserve seclusion while retaining a hospitable healthcare ambiance [6]. Prominent signs and direction systems were established to assist patients, family members, and staff in navigating the renovated layout.
Culturally mindful security staff members were recruited to tackle possible apprehensions tied to mixed-gender wards. This preemptive strategy elevated patient safety and overall satisfaction. The hospital integrated periodic evaluation and scrutiny of security methods into its quality assurance guidelines, permitting alterations based on feedback to sustain effective security practices tailored to the distinct challenges presented by a mixed-gender healthcare setting.
Conclusion
This investigation of diversified-gender wards at the Security Forces Hospital in Riyadh reveals a successful shift from gender-centric assignment to a patient-centered approach. The decline in patient withdrawals and enhanced bed utilization resulted from executive administration endorsement, patient connection, cultural awareness, transformative supervision, staff guidance, nursing management participation, and protective protocols. This article presents vital information for hospital leaders contemplating similar adjustments.
Essential points to consider involve concentrating on patient-driven care by eliminating gender-based constraints and focusing on operational competence via refined resource distribution. Executive backing is vital for overcoming opposition and nurturing an atmosphere of a positive transformation. Addressing cultural concerns, allocating resources to staff growth and training, involving nursing authorities in strategizing and implementation, and establishing sufficient safety precautions are indispensable elements of incorporating mixed-gender wards.
The Security Forces Hospital program functions as a model for boosting patient-focused care and functional efficacy through integrated-gender inpatient ward assimilation. The inclusive method, together with cultural sensitivity and employee advancement, has positively revolutionized the patient care setting. The outcomes demonstrate the potential for change when adaptability, patient-oriented principles, and calculated organizational transformations are welcomed.
Acknowledgements
We express our heartfelt gratitude to all who contributed to the development of this investigation. The Security Forces Hospital’s executive administration played a pivotal role in its accomplishment, significantly improving patient treatment. The combined efforts and expertise of the project team members navigated intricate challenges, leading to collective success. Healthcare experts and personnel displayed adaptability and an unwavering commitment to high-quality care. Patients and families showed trust and willingness to accept the change, helping to shape a patient-centric healthcare atmosphere. The paper exemplifies our shared dedication to healthcare excellence and ongoing improvements.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
All the authors contributed substantially to the conception and design of this work and revised and drafted the manuscript. The authors approved the final version to be published and is accountable for all aspects of this work.
Conflict of Interest Statement
None declared.
Disclosure
The authors report no conflicts of interest in this work.
References
- Scully, E. (2022). Mixed wards rules broken 13,000 times as NHS breaches blamed on lack of beds. The Mirror.
Publisher | Google Scholor - Schäfer, F., Walther, M., Hübner, A., & Kuhn, H. (2019). Operational patient-bed assignment problem in large hospital settings including overflow and uncertainty management. Flexible Services and Manufacturing Journal, 31, 1012-1041.
Publisher | Google Scholor - Hunter, D., McCallum, J., & Howes, D. (2019). Defining exploratory-descriptive qualitative (EDQ) research and considering its application to health care. Journal of Nursing and Health Care, 4(1).
Publisher | Google Scholor - Young, S. & Guo, K. L. (2020). Cultural diversity training: The necessity of cultural competence for health care providers and in nursing practice. The Health Care Manager, 39(2),100-108.
Publisher | Google Scholor - Stewart, E. C., Davis, J. S., Walters, T. S., Chen, Z., Miller, S. T., et al. (2023). Development of strategies for community engaged research dissemination by basic scientists: A case study. Translational Research, 252:91-98.
Publisher | Google Scholor - Nowrozy, R., Ahmed, K., Wang, H., & Mcintosh, T. (2023). Towards a universal privacy model for electronic health record systems: An ontology and machine learning approach. In Informatics MDPI, 10 (3):60.
Publisher | Google Scholor