Case Report
Immediate Placement and Immediate Loading Within 72 Hours: Where Time Meets Demand
1Head, Department of Prosthodontics, Crown and Bridge; Desh Bhagat Dental College and Hospital, Mandi Gobindgarh, India.
2The Specialist Clinic, Delhi, India.
3Private practice, Silver Spring, Maryland, United States.
4Professor, Dept of Prosthodontics, Crown and Bridge; Desh Bhagat Dental College and Hospital, Mandi Gobindgarh, India.
5Post Graduate Student (3rd Year), Dept of Prosthodontics, Crown and Bridge; Desh Bhagat Dental College and Hospital, Mandi Gobindgarh, India.
*Corresponding Author: Gregori M. Kurtzman,Private practice, Silver Spring, Maryland, United States.
Citation: Manmeet S. Gulati, Mahesh L, Gregori M. Kurtzman, Singh M, Singla L. (2024). Immediate Placement and Immediate Loading Within 72 Hours: Where Time Meets Demand, Dentistry and Oral Health Care, BioRes Scientia Publishers. 3(2):1-8. DOI: 10.59657/2993-0863.brs.24.032
Copyright: © 2024 Gregori M. Kurtzman, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 06, 2024 | Accepted: March 20, 2024 | Published: March 23, 2024
Abstract
Oral health and oral health care are important aspects in order to maintain proper mastication, deglutition, digestion, and psychological well-being. Mutilation of teeth is henceforth a traumatic experience for the patient. This case report reiterates that successful implant supported prosthesis can be placed in patients with fresh extraction sockets following the immediate implant placement, conditioned that comprehensive treatment planning including all relevant investigations are done and the surgical trauma is kept to a minimum.
Keywords: oral health care; implant supported prosthesis; immediate implant placement; comprehensive treatment planning
Introduction
The use of dental implants to replace missing teeth has increased enormously in the last decade, rendering new treatment options, such as implant-supported fixed restorations for fully and partially edentulous patients [1]. However, immediate extraction of all teeth and immediate rehabilitation with fixed full arch implant-supported prostheses requires a lengthy treatment period but current modern working lives make it difficult for patients to undergo lengthy treatments involving numerous sessions. The field of implantology is advancing at an unbeatable pace, leading to the evolution of various placement, and loading protocols to provide a quicker and easier surgical approach. For patients who have their own teeth but who will eventually lose them, and who plan to undergo implant-supported rehabilitation, all residual teeth can be extracted, and implants installed in a single procedure [2].
The advantages of immediate implant placement include reduction in the number of surgical interventions, a shortened rehabilitation time and higher patient satisfaction compared with delayed implant placement [5,4]. Another advantage of immediate implant placement in the extraction socket is the counteracting of the hard tissue resorption that occurs following tooth extraction. In the literature, previous research shows that survival rates for immediately placed implants are comparable to those of implants placed in healed alveolar bone [5,7]. Misch suggested a terminology for immediate restoration or occlusal loading. The immediate occlusal loading protocol is an implant supported temporary or definitive restoration in occlusal contact within two weeks of the implant insertion. Nonfunctional immediate restoration describes implant prosthesis with no direct occlusal load within two weeks of implant and is primarily considered in partially edentulous patients [8,9]. This case report involves immediate implant placement in both upper and lower arches in a patient undergoing extraction of all residual teeth for rehabilitation with fixed full-arch implant supported prostheses.
Case Report
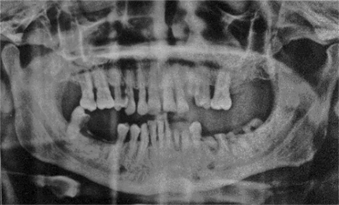
A 46-year-old male patient from Scotland reported to the practice with the chief complaint of badly looking teeth and also wanted replacement for the missing teeth. The medical history of the patient was found to be relatively insignificant. Complete intra oral examination was performed noting extensive caries of the remaining dentition (Figure 1).
Figure 1: Pre-operative presentation demonstrating extensive generalized decay.
Figure 2: Panoramic radiograph at presentation demonstrating extensive generalized decay of the remaining dentition and minimal bone loss in both arches.
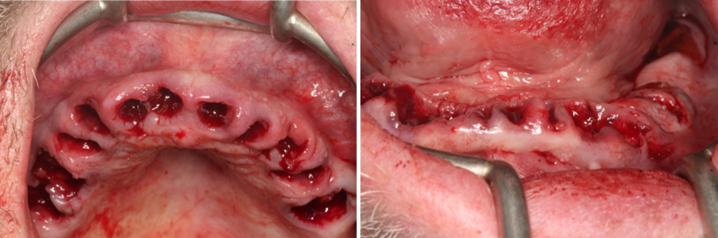
A panoramic radiograph was taken to evaluate the dentition. The patient was given a detailed explanation concerning the present state, alternative treatment plans and the proposed procedure which included extraction of the remaining dentition, immediate implant placement and immediate loading using a milled acrylic hybrid followed by zirconia prosthesis over titanium bar framework after a period of 3-4 months. The patient was very conscious about his aesthetics and was very keen for the earliest possible restoration of his teeth and so he opted for the proposed treatment procedure. Relevant lab investigations and Cone Beam Computed Tomography examination (CBCT) were done and found to be favorable for prognosis of the proposed treatment. Preparations for surgery were performed according to the standard protocols. Pre- operative diagnostic records were made and surgical procedures were performed under local anesthesia (2% lidocaine with 1: 100,000 epinephrine). Before implant placement, selected teeth were extracted carefully to preserve the residual alveolar bone; this was performed on the day of surgery, within the same surgical procedure (Figure 3).
Figure 3: Maxillary (left) and mandibular (right) arches following extraction of the dentition.
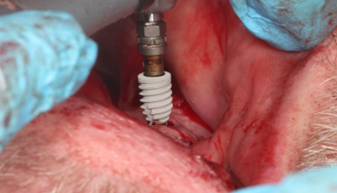
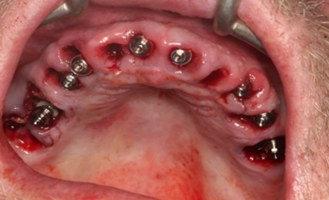
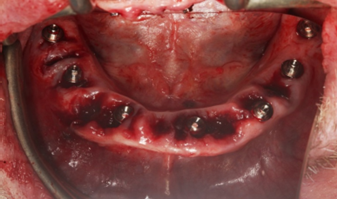
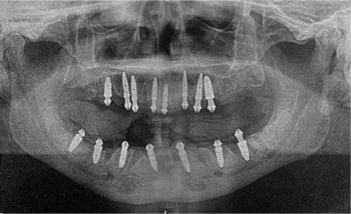
After complete curettage of the extraction sockets immediate implant placement was done achieving significant primary stability (45 Ncm). 8 implants (Bioner Dental Implants) were placed in the maxillary arch and 7 in the mandibular arch post extractions (Figures 4 and 5).
Figure 4: Implant placement (Bioner Dental Implants) in maxillary immediate extraction sockets.
Figure 5: Implant placement (Bioner Dental Implants) in mandibular immediate extraction sockets.
The longest and widest possible implants were placed in the residual crest and the extraction sockets in order to achieve an aesthetic profile and maximum vertical preservation. As the patient had to go back overseas so immediate loading was planned for which scan body impressions were taken (Figure 6).
Figure 6: Scan bodies placed on the immediately placed implants in the maxillary arch in preparation for a digital impression using the TRIOS 5 unit.
Using intraoral scanner (TRIOS 5) and sent to lab (STL format) for the fabrication of provisional restoration made from milled acrylic. Following this, multiunit abutments (Bioner Dental Implants) were fastened over all the implants (Figures 7 and 8).
Figure 7: Maxillary arch following immediate implant placement and insertion of MUA on each implant.
Figure 8: Mandibular arch following immediate implant placement and insertion of MUA on each implant.
A panoramic radiograph was taken to document implant placement anatomically and verify full seating of the MUA’s. (Figure 9) Post surgery instructions were delivered to the patient and prescribed with antibiotic therapy, anti-inflammatory agents, and mouth rinse for 1 week. The patient was recalled one day post-surgery, and the provisional restorations (Milled acrylic) were placed (Figure 10) and was happy and satisfied with the esthetics. Telephonic follow up of the patient was scheduled and carried out at definite time intervals.
Figure 9: Panoramic radiograph of the immediate placed implants in the maxillary and mandibular arches with attached MUA.
Figure 10: Verification stent fabricated intraorally on the maxillary implants.
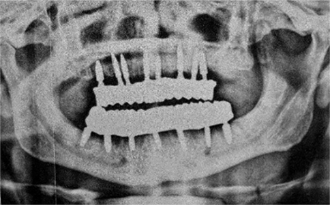
After a period of approximately 3 months, the patient came back for the final restoration. Open tray impression copings were placed and intraoral splinting was performed utilizing GC pattern resin (Figures 11 and 12) followed by impressions made utilizing VPS impression material (Flexceed; GC). Jig trial verification was performed, and any necessary corrections were performed by splitting and re-joining the jig (Figure 13). The bite of the patient was recorded. On the next appointment, the titanium framework was tried in to verify passive fit to the implants in each arch. The screw-retained hybrid prosthesis was completed with the addition of zirconia over the titanium bar framework. The finished final hybrid prosthetics was inserted intraorally. (Figures 14 and 15). The patient was immensely satisfied with the esthetic outcome. A panoramic radiograph was taken to verify complete seating of the prosthesis. (Figure 16) Follow ups were scheduled for the patient.
Figure 11: Verification stent fabricated intraorally on the mandibular implants.
Figure 12: Maxillary and mandibular verification stents following removal intraorally.
Figure 13: Provisional restorations made of milled acrylic inserted intraorally.
Figure 14: Screw retained zirconia over titanium bar framework final prosthesis on the maxillary and mandibular arches.
Figure 15: Screw retained zirconia over titanium bar framework final prosthesis on the maxillary and mandibular arches.
Figure 16: Panoramic radiograph of the completed immediate screw retained hybrid prosthetics on the immediate placed implants.
Discussion
In the modern era, the immediate implant concept is gaining popularity for replacing missing teeth, especially in cases of full mouth rehabilitations. Krump and Barnett reported high success rates with dental implants placed at the time of extraction [10,11]. Immediate implant placement presents advantages such as implants in fresh extraction sites can be placed in the same location as the extracted tooth thereby minimizing the need for angled abutments, osseointegration is more favorable, preventing atrophy of the alveolar ridge thereby preventing recession of the mucosal and gingival tissues and many more. Immediate placement and immediate loading of implants is more predictable and successful [12-15]. However, this approach cannot be applied to every immediate implant patient. In comparison to conventional implant treatment, the immediate loading procedure requires more chair-side time at the time of implant placement for both the restorative dentist and the patient. Careful patient screening and selection are required when an immediate implant placement with immediate loading procedure is a treatment consideration. Primary stability of immediately placed implant seems to be the most important factor in immediate loading.
Conclusion
This case report demonstrates that it is possible to achieve greater efficiency in our efforts to give patient sound, timely and economical treatment. Based on the outcomes of the present case report and short review of the literature, it can be concluded that immediate implant placement with immediate loading may prove to be a viable treatment option for judiciously selected cases requiring earliest restoration of teeth to be extracted. However, this mode of treatment is highly technique sensitive and requires expertise for its execution. Careful case selection, proper treatment plan and follow-up of surgical and prosthetic protocols are the keys to success.
Conflicts of interest
There were no conflicts of interest.
References
- Touyz L. Z. G. (2023). Orally Transferred Aphorisms of Dentistry. Dentistry and Oral Health Care. BRS Publishers, 2(2).
Publisher | Google Scholor - Touyz L. Z.G. (2023). More Orally Transmitted Aphorisms (OTA’s-2) in Dentistry. Dentistry and Oral Health Care. BioRes Scientia Publishers, 2(2):1-4.
Publisher | Google Scholor - Touyz L.Z.G. (2017). The Pathophysiology of Oral Biofilms and it’s relation to Initial Gum Disease and Caries. J Dent Oral Disord Ther. 5(4):1-6.
Publisher | Google Scholor - McAllister B. S., & Haghighat K. (2007). Bone augmentation techniques. Journal of periodontology, 78(3):377-396.
Publisher | Google Scholor - Buser, D. Sennerby, L., & De Bruyn H. (2017). Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontology, 73(1):7-21.
Publisher | Google Scholor - Chiapasco M., Casentini P., & Zaniboni M. (2009). Bone augmentation procedures in implant dentistry. International Journal of Oral & Maxillofacial Implants, 24.
Publisher | Google Scholor - Friberg B. (2016). Bone augmentation for single tooth implants: A review of the literature. Eur J Oral Implantol, 9(Suppl 1), S123-S134.
Publisher | Google Scholor - Sayed M. E., Mugri M. H., Almasri,M. A., Al-Ahmari M. M., Bhandi S., Madapus, T. B., Patil, S. (2021). Role of stem cells in augmenting dental implant osseointegration: a systematic review. Coatings, 11(9):1035.
Publisher | Google Scholor - Touyz L.Z.G. (2018.) Unwanted stress arising from break- down in communication. Coping strategies. Jnl Cosmetol & Oro-Facial Surg, 4:1-3.
Publisher | Google Scholor - Touyz L.Z.G. (2015). Management and Coping Strategies of stress in Dentistry. Jnl of Dentistry and Management. DRM, 1:9-15.
Publisher | Google Scholor - Xie Q., Närh, T. O., Nevalainen J. M., Wolf J., Ainamo A. (1997). Oral status and prosthetic factors related to residual ridge resorption in elderly subjects. Acta Odontologica Scandinavica, 55(5):306-313.
Publisher | Google Scholor - Kovačić I., Čelebić A., Knezović Zlatarić D., Petričević N., Buković D., Bitanga P., Ognjenović M. (2010). Decreasing of residual alveolar ridge height in complete denture wearers. A five year follow up study. Collegium anthropological, 34(3):1051-1056.
Publisher | Google Scholor - Wyatt C. C. (1998). The effect of prosthodontic treatment on alveolar bone loss: a review of the literature. The Journal of prosthetic dentistry, 80(3):362-366.
Publisher | Google Scholor - Martori E., Ayuso-Montero R., Martinez-Gomis J., Viñas M., Peraire, M. (2014). Risk factors for denture-related oral mucosal lesions in a geriatric population. The Journal of prosthetic dentistry, 111(4):273-279.
Publisher | Google Scholor - Mercier P., Lafontant R. (1979). Residual alveolar ridge atrophy: classification and influence of facial morphology. The Journal of prosthetic dentistry, 41(1):90-100.
Publisher | Google Scholor - Nucera R., Lo Giudice A., Bellocchio M., Spinuzza P., Caprioglio A., Cordasco G. (2017). Diagnostic concordance between skeletal cephalometric, radiograph-based soft-tissue cephalometric, and photograph-based soft-tissue cephalometric. European journal of orthodontics, 39(4):352-357.
Publisher | Google Scholor - Rohlin M., Akesson L., Hakansson J., Hakansson H., Nasstrom K. (1989). Comparison between panoramic and periapical radiography in the diagnosis of periodontal bone loss. Dent maxillofacial Radiology, 18(2):72-76.
Publisher | Google Scholor - White S. C., Atchiso K. A., Hewlett E. R., Flack V. F. (1995). Clinical and historical predictors of dental caries on radiographs. Dent maxillofacial Radiology, 24(2):121-127.
Publisher | Google Scholor - Tyndall D. A., Rathor, S. (2008). Cone-beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications. Dental Clinics of North America, 52(4):825-841.
Publisher | Google Scholor - Preshaw P. M. (2015). Detection and diagnosis of periodontal conditions amenable to prevention. BMC oral health, 15(1):1-11.
Publisher | Google Scholor - Viner M. D., Robson J. (2017). Post-Mortem Forensic Dental Radiography-a review of current techniques and future developments. Journal of Forensic Radiology and Imaging, 8:22-37.
Publisher | Google Scholor - Heinrich A., Güttler F., Wendt S., Schenkl S., Hubig M., Wagner, R., Teichgräber U. (2018). Forensic odontology: automatic identification of persons comparing antemortem and postmortem panoramic radiographs using computer vision. In RöFo-Fortschritte auf dem Gebiet der Röntgenstrahlen und der bildgebenden Verfahren, 190(12):1152-1158.
Publisher | Google Scholor - Otto, T., De Nisco S. (2002). Computer-aided direct ceramic restorations: a 10-year prospective clinical study of Cerec CAD/CAM inlays and onlays. International Journal of Prosthodontics, 15(2).
Publisher | Google Scholor - Otto T., Schneider D. (2008). Long-term clinical results of chairside Cerec CAD/CAM inlays and onlays: a case series. The International journal of prosthodontics, 21(1):53-59.
Publisher | Google Scholor - Otto T. (2017). Up to 27-years clinical long-term results of chairside Cerec 1 CAD/CAM inlays and onlays. International journal of computerized dentistry, 20(3).
Publisher | Google Scholor - Arnim S.S. (1963). The Use of Disclosing Agents for Measuring Tooth Cleanliness. The Journal of Periodontology, 34(3):227-230. https://doi.org/10.1902/jop.1963. 34.3.227-30.
Publisher | Google Scholor - Touyz L.Z.G. (2017). The Pathophysiology of Oral Biofilms and it’s relation to Initial Gum Disease and Caries. J Dent Oral Disord Ther, 5(4):1-6.
Publisher | Google Scholor - TOUYZ L.Z.G., Nassani L.M., Touyz S.J.J. (2019). Patterns of hard tissue dental abfractions as indicators of extrinsic etiologies. Scientific Archives of Dental Science. ICMJ Scientific Archives of Dental Sciences, (2)3:21-24.
Publisher | Google Scholor - Touyz L.Z.G., Mehio A. (2006). Dental Ravages from Acidulated Soft Drinks. Jnl Aesthetic and Implant Dentistry, 8(3):20-33.
Publisher | Google Scholor - Ferrari C.I.C, Touyz L.Z.G (2013) Clinical implications from an in vitro and in vivo investigation of Acidity, Erosion and Pain from common Pop-Acidulated Drinks. International Journal of Clinical Dentistry, 6(3):279-290.
Publisher | Google Scholor - Borjian A., Ferrari C.I.C.F., Anouf A., and TOUYZ L.Z.G. (2010). Pop-Cola Acids and Tooth Erosion: An In Vitro, In Vivo, Electron-Microscopic, and Clinical Report. International Journal of Dentistry, 12.
Publisher | Google Scholor - Oreskes N. (2023). Masked Confusion. Scientific America, 4:90-91.
Publisher | Google Scholor - Bonchek, L. I. (2016). Absence of evidence is not evidence of absence. The Journal, 11(3): 65.
Publisher | Google Scholor - Londero, A. B., Reiniger, A. P. P., Tavares, R. C., Ferreira, C. M., Wikesjö, U. M., Kantorski, K. Z., & Moreira, C. H. C. (2022). Efficacy of dental floss in the management of gingival health: a randomized controlled clinical trial. Clinical Oral Investigations, 26(8): 5273-5280.
Publisher | Google Scholor - Bosma, M. L., McGuire, J. A., Sunkara, A., Sullivan, P., Yoder, A., Milleman, J., & Milleman, K. (2022). Efficacy of Flossing and Mouthrinsing Regimens on Plaque and Gingivitis: A randomized clinical trial. American Dental Hygienists' Association, 96(3):8-20.
Publisher | Google Scholor - Vernon, L. T., Seacat, J. D. (2017). In defense of flossing: can we agree it's premature to claim flossing is ineffective to prevent dental caries? Journal of Evidence Based Dental Practice, 17(2):71-75.
Publisher | Google Scholor