Case Report
Gluteal Diclofenac Injection Lesion Can Mimic an Abscess on MRI
- Makgabo John Tladi *
FCS and MMed ortho, Louis Pasture Hospital, Pretoria, South Africa.
*Corresponding Author: Makgabo John Tladi, FCS and MMed ortho, Louis Pasture Hospital, Pretoria, South Africa.
Citation: Makgabo J. Tladi. (2023). Gluteal Diclofenac Injection Lesion Can Mimic an Abscess on MRI. Clinical Case Reports and Studies, BRS Publishers. 2(2); DOI: 10.59657/2837-2565.brs.23.019
Copyright: © 2023 Makgabo John Tladi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 09, 2023 | Accepted: February 01, 2023 | Published: February 08, 2023
Abstract
Intramuscular diclofenac injection is commonly used for pain management. Case reports have shown that after injection of diclofenac, local complications can occur but still underestimated. Acute muscle trauma can be found at the injection site. Limited studies have dealt with muscular radiological findings after diclofenac injection. This is a case report of an incidental gluteal lesion that was suggestive of an abscess on MRI following diclofenac intramuscular injection.
Keywords: NSAIDs; diclofenac; voltaren
Introduction
Pain can result with morbity, hence one will try to find a mechanism to relive it. Various types of analgesia can be found over the counter or through a prescription. Medications for pain can either be given oral, topical, intravenous (IV) or intramuscular (IM) which can result with local or systemic complications. The complications can either be minor or severe that can result with chronic medical conditions or death if not identified early and treated accordingly. Commonly, non-steroidal anti-inflammatory (NSAIDs) are used to manage pain [1.2]. Diclofenac as a NSAIDs can either be given as topical, oral or IM. The bioavailability of IMI is greater than oral route.3 Probst et.al. found that plasm creatine activity was elevated more than sixfold within eight hours after the IMI and returned to normal values after one week [4]. Local side effects have been reported to be lower with diclofenac. Abscess and tissue necrosis at the site of injection has been reported following diclofenac injection [5].
Case Report
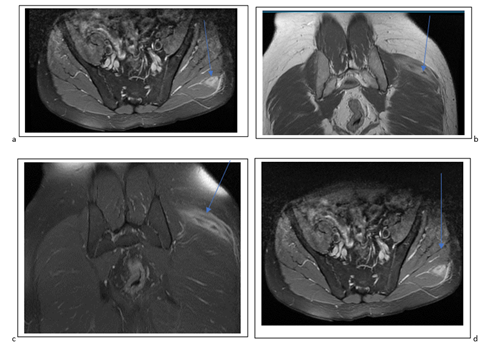
A 43 years old male presented with atraumatic backache for 4 weeks. He was a referred by his family physician after not responding to oral pain medication. According to the referral letter, he was given diclofenac injection, oral analgesia and topical anti-inflammatory four weeks ago. Clinical examination revealed tense paraspinal back muscles and decrease sensation along L4/5 distribution. He had a normal lower limbs motor power. His rectal and bladder sphincter control were also normal. He did not have signs of spinal cord or nerve roots compression. The was a non-tender smooth, mobile 1x 1 cm mass on his right buttock. He reports that it was the area that his doctor injected him. The lumbar and pelvis x rays were normal. The MRI showed lumbar spondylosis, small L4/5 disc bulging and also a lesion (figure 1) on his left gluteal muscle with an enhancement. The lesion was suggestive of an abscess. The radiologist called the surgeon to inform him that the MRI shows signs suggestive of an infection.
Figure 1: MRI (a-d) showing an enhanced lesion (blue arrows) of the left gluteal maximus muscle
Inflammatory markers (erythrocyte sedimentation rate, and C-reactive protein), full blood count with differentials and random glucose were within normal ranges. A diagnosis of diclofenac lesion was made. He was given analgesia and referred to physiotherapy for his backache. When he came back after six weeks, the nodule had disappeared, and backache was better.
Pain can result with morbity; hence one will try to find a mechanism to relive it. Various types of analgesia can be found over the counter or through a prescription. Medications for pain can either be given oral, topical, intravenous (IV) or intramuscular (IM) which can result with local or systemic complications. Some of the complications can either be minor or severe that can result with irreversible tissue damage or death if not identified early and treated accordingly. Commonly, non-steroidal anti-inflammatory (NSAIDs) are used to manage pain [1,2]. Diclofenac as a NSAIDs can be administrate as topical, oral or IM. The bioavailability of IMI is greater than oral route [3]. Probst et.al. found that plasm creatine activity was elevated more than sixfold within eight hours after the IMI and returned to normal values after one week [4]. Local side effects have been reported to be lower with diclofenac injection. Abscess and tissue necrosis at the site of injection has been reported following diclofenac injection [5].
Discussion
Diclofenac is a NSAIDs of the phenylacetic acid class with anti-inflammatory, analgesic, and antipyretic properties. Mechanism of action is through inhibition of both cyclooxygenase (COX-1 and COX-2) enzymes. This inhibits the synthesis of prostanoids (prostaglandin [PG]-E2, PGD2, PGF2, prostacyclin [PGI2], and thromboxane) [2,3]. Studies have suggested that local tissue damage following diclofenac is due to direct cytotoxicity, osteoblast and tumor cells. Gluteal muscle damage can be seen after the injection. Plasma creatine levels are initially higher but return to normal within a week [4]. Inflammatory marks are normally with normal range [4] just like in this case report.
MRI findings after diclofenac injection include increased signal intensity due to oedema of the muscles. At approximately 30 minutes after gluteal injection, they can be rapid enhancement of the T2-weighted image. The enhancement disappeared after five weeks. Only one case report was found that describe MRI findings of gluteal diclofenac injection [4].
Severe local reaction following diclofenac injection include Nicolau syndrome (also known as embolia cutis medicamentosa or livedoid dermatitis). This rare condition occurs after intramuscular injection of various drugs. Drugs that have been seen to be associated with this condition include diclofenac, pencilling, corticosteroids and triple vaccination. The pathogenesis is unknown. Presentation include pain around the injection site after the injection, followed by erythema, livedoid patch, haemorrhagic patch and finally necrosis of the skin, subcutaneous fat and muscle tissues [6, ,7, 8]. The are no radiological description of the condition. Ultrasound can show thickening of the skin and subcutaneous fat layer while MRI can show tissue oedema and fluid collection [9]. The radiological investigations can assist with evaluating the extend of the condition. Supportive management can be used for this condition [7,8,9].
Death following the diclofenac injection can occur. Rygnestad and Kvam reported streptococcal myositis and tissue necrosis that resulted with death of a young patient after the injection [2]. Although diclofenac can be used to manage pain, its side effects may be detrimental.
Conclusion
Clinicians should be aware of the local and systemic complications that that are associated with the use of NSAIDs. Diclofenac muscular infiltration lesion and Nicolau syndrome should be part of differential if MRI shows inflammatory soft tissue changes following the injection.
Conflict of interest
Author declares no conflict of interest
References
- Abdu N, Mosazghi A, Teweldemedhin S, Asfaha L, et al. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Usage and co-prescription with other potentially interacting drugs in elderly: A cross-sectional study. PLOS ONE 15(10):e0238868.
Publisher | Google Scholor - Rygnestad T, Kvam AM. (1995). Streptococcal myositis and tissue necrosis with intramuscular administration of diclofenac (Voltaren). Acta Anaesthesiol Scand. 39(8):1128-1130.
Publisher | Google Scholor - Altman R, Bosch B, Brune K et al. (2015). Advances in NSAID development: evolution of diclofenac products using pharmaceutical technology. Drugs, 75:859–877.
Publisher | Google Scholor - Probst M, Kühn JP, Modeß C, Scheuch E, Seidlitz A et al. (2017). Muscle injury after intramuscular administration of diclofenac: A Case Report Supported by Magnetic Resonance Imaging. Drug Saf Case Rep, 4(1):7.
Publisher | Google Scholor - Chung C. (2002). The use of injectable nonsteroidal anti-inflammatory drugs in local accident & emergency practice. Hong Kong Journal of Emergency Medicine, 9(2):65-71.
Publisher | Google Scholor - Lie C, Leung F, Chow SP. (2006). Nicolau syndrome following intramuscular diclofenac administration: a case report. J Orthop Surg (Hong Kong). 14(1):104-107.
Publisher | Google Scholor - Luton K, Garcia C, Poletti E, Koester G. (2006). Nicolau Syndrome: three cases and review. Int J Dermatol. Nov;45(11):1326-1328.
Publisher | Google Scholor - Lie C, Leung F, Chow SP. (2006). Nicolau syndrome following intramuscular diclofenac administration: a case report. J Orthop Surg (Hong Kong). 14(1):104-107.
Publisher | Google Scholor - Park HJ, Kim MS, Park NH, et al. (2011). Sonographic findings in Nicolau syndrome following intramuscular diclofenac injection: a case report. J Clin Ultrasound. 39(2):111-113.
Publisher | Google Scholor