Case report
Functional and Efficacy Evaluation of Surgical Treatment for Osteonecrosis of The Humeral Head: A Systematic Review with Meta-Analysis
- Bianca Gabriella de Oliveira 1*
- Rafael Fernandes da Silva 2
- Vitória Torrano Carvalho Pereira Peixoto 3
- Ravi Cavalcanti Mendes 4
- Denilson Ribeiro Werneck 5
- Laís Cristina Pereira da Silva 6
- Melissa Alves Aires Marques 7
- marcella rodrigues costa simões 8
1Medical Student at Universidade Salvador-UNIFACS, Salvador, BA, Brazil.
2Resident doctor in Orthopedics and Traumatology at the Hospital Adriano Jorge Foundation, Manaus, AM.
3Resident doctor in Orthopedics and Traumatology at Hospital São Rafael, Salvador, BA.
4Resident doctor in Orthopedics and Traumatology at the Hospital das Clínicas of the Federal University of Bahia.
5Resident doctor in Orthopedics and Traumatology at the Dona Lindu State
6Traumatology and Orthopedics Hospital, Paraíba do Sul, RJ.
7Medical Student at the University of Salvador-UNIFACS, Salvador, BA, Brazil.
8Doctor Orthopedist and traumatologist at Hospital da Baleia, Belo Horizontes, MG; hand and microsurgery surgeon at Hospital Maria Amélia Lins (FHEMIG), Belo Horizonte, MG, Brazil.
*Corresponding Author: Bianca Gabriella de Oliveira, Medical Student at Universidade Salvador-UNIFACS, Salvador, BA, Brazil.
Citation: Bianca G. Oliveira, Rafael F. Silva, V.T.C.P. Peixoto, Ravi C. Mendes, Denilson R. Werneck. (2024). Functional and Efficacy Evaluation of Surgical Treatment for Osteonecrosis of The Humeral Head: A Systematic Review with Meta-Analysis, Clinical Interventions and Clinical Trials, BioRes Scientia Publishers. 2(2):1-09. DOI: 10.59657/2993-1096.brs.24.018
Copyright: © 2024 Bianca Gabriella de Oliveira, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 13, 2024 | Accepted: February 28, 2024 | Published: March 09, 2024
Abstract
Objective: to investigate the results of the efficacy of surgical treatment in patients with osteonecrosis of the humeral head (ONHH) by means of a systematic review of comparative analysis of hemiarthroplasty (HA) and total shoulder arthroplasty (TSA) with meta-analysis. Materials and methods: a retrospective study using a systematic review with METANALYSIS.8 The search was carried out using the following search terms in the PubMed, EMBASE, Scopus, Ovid and Cochrane Library databases. A text search strategy was employed using the search string osteonecrosis of the humeral head OR avascular necrosis OR head replacement or hemiarthroplasty or total shoulder arthroplasty. Results: The 05 articles selected presented patients diagnosed with osteonecrosis of the humeral head who underwent treatment by total arthroplasty or hemiarthroplasty. The degrees of elevation, external and internal rotation of the shoulder after the established procedures were analyzed, in addition to the VAS (pain analogue assessment) and ASES (American Shoulder and Elbow Surgeons) scales present in some of these studies. A total of 271 patients were included, 144 of whom underwent hemiarthroplasty and 127 total shoulder arthroplasty. The studies showed that TSA was preferentially used in older patients, with HA being preferred in cases where the glenoid cartilage remains intact or almost intact. Both HA and TSA provided significant relief in pain and limb function. Conclusion: HA (hemiarthroplasty) should preferably be indicated in young patients without glenoid injury. TSA (total arthroplasty) is indicated for grade V or other stages in conjunction with a damaged glenoid.
Keywords: functional surgical treatment; efficacy evaluation of surgical treatment; osteonecrosis; humeral head
Introduction
The humeral head is a bone structure susceptible to avascular necrosis, an anatomical region with a higher prevalence of loss of blood supply and/or increased intraosseous pressure, with a higher prevalence after the femoral head [1,2]. Osteonecrosis of the humeral head leads to incongruence of the glenohumeral joint and consequent alterations due to the degenerative process, which can include severe complications such as loss of range of movement, intense pain and can lead to subchondral fractures and/or arthritis and arthrosis [3,4,5]. Some etiologies for osteonecrosis can be cited: steroid and/or alcohol use, prolonged corticosteroid therapy, the presence of sickle cell disease, systemic lupus erythematosus and/or rheumatological pathology, post-traumatic events, exposure to radioactive factors and idiopathic causes. Faced with the diagnostic challenge, a stage-based classification was created as follows: stage 1 presents a positive finding on MRI or bone scintigraphy with a normal humeral head on plain radiographs, stage 2 marked by sclerotic alteration without cephalic collapse, stage 3 designated subchondral bone collapse without or with mild loss of cephalic sphericity, stage 4 by advanced head collapse with intact glenoid and stage 5: AGH incongruence and arthritic alteration [8,9]. Osteonecrosis may not be identified initially because there is no significant weight load on the shoulder, since there is no significant load on the joint, and because the symptoms may be mild or slight. As far as pain is concerned, it is usually pulsatile and deep, radiating from the shoulder to the elbow, although it is difficult to pinpoint the exact location of the pain.With regard to mobility, active movement is generally limited, while passive movement is maintained [10].
Therapeutic management is the most important in controlling the patient's quality of life and reducing the risk of complications, so staging is taken into account and treatment options include: non-operative management, arthroscopic debridement, core decompression, osteochondral autograft or allograft transplantation, surface replacement, hemiarthroplasty (HA) and total shoulder arthroplasty (TSA). Thus, the therapeutic indication is based on the classification, such as the example of arthroplasty which is performed on patients with substantial pain with functional disability in late stage 3 to stage 5 and who do not respond to non-operative treatment [6,7].
Conservative treatment can be effective in stages I and II or early stage III (Robert G et al., 2008). When radiological and clinical progression is evident, approaches that preserve the joint are chosen, such as core decompression and arthroscopic debridement. Then, in cases of advanced stages (III, IV or V), with progression of ON too painful subchondral fractures, irregular articular surfaces and subsequent degenerative changes, prosthetic replacement is constantly advised. Hemiarthroplasty (HA) or humeral head replacement has been indicated for stage III and IV pathology, when the glenoid cartilage is intact, and total shoulder arthroplasty (TSA) for stage V [11,12,13]. Due to its high prevalence at a young age, it is essential to scientifically evaluate the results of therapeutic management. Arthroplasty provided limited results, and most studies had few cases or only short-term follow-up. Therefore, investigating the clinical outcomes, complications and reoperations of each arthroplasty is important, as is comparing the effectiveness of other surgical techniques [7]. The aim of this study was to investigate the results of the effectiveness of surgical treatment in patients with osteonecrosis of the humeral head (ONHH) by means of a systematic review of comparative analysis of hemiarthroplasty (HA) and total shoulder arthroplasty (TSA) with metanalysis.
Methodology
The systematic review protocol was registered in the International prospective register of systematic reviews (PROSPERO) under ID CRD42024508197 in order to improve the quality and suitability of the results to the proposed objectives. This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline and is a retrospective study carried out using a systematic review with METANALYSIS.8 The search was carried out using the following search terms in the PubMed, EMBASE, Scopus, Ovid and Cochrane Library databases. A text search strategy was employed using the search sequence osteonecrosis of the humeral head OR avascular necrosis OR head replacement or hemiarthroplasty or total shoulder arthroplasty, excluding all non-shoulder articles. As this was a meta-analysis of published studies, there was no need for approval by the ethics committee or institutional scientific review board. The reference lists of included and previously published articles were searched for more relevant studies that met the eligibility criteria. The inclusion criteria for the selection of studies were constructs whose sample included patients with osteonecrosis of the humeral head treated by surgical procedures. Studies addressing osteonecrosis of another anatomical region were excluded from the search.
We sought to analyze the applicability of the surgical procedure in the approach to humeral osteonecrosis, eligibility criteria for the procedure, associated risks and benefits, correlation between the procedure and functionality after surgery or length of hospital stay after the procedure. Three independent reviewers applied the eligibility criteria and selected the studies for inclusion in the systematic review. The researchers were blind to each other's decisions. Information on study design, study methodology, participant demographics (age, gender), baseline characteristics (degree of osteonecrosis, previous surgeries) was extracted from the studies. The Systematic Review Data Repository-Plus software tool was used. It was also decided to use the Cochrane risk of bias tool for greater reliability of the results.9 The results were synthesized qualitatively, as well as by combining data from individual studies that addressed the associated benefits and/or risks.
Results
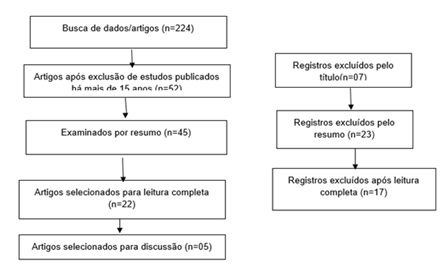
Initially, 224 articles were selected in the data search process, excluding those that had been published for more than 15 years, leaving 52 studies. After evaluating the title and abstract, 30 articles were eliminated, leaving 22 for full reading. Of these, 17 were excluded because they did not meet the inclusion criteria and 5 were included in the study (Figure 1).
Figure 1: Selection of studies according to the PRISMA methodology.
Source: Authorship own (2024).
The 05 articles selected presented patients diagnosed with osteonecrosis of the humeral head who had undergone treatment by total arthroplasty or hemiarthroplasty. The degrees of elevation, external and internal rotation of the shoulder after the established procedures were analyzed, in addition to the VAS (pain analogue assessment) and ASES (American Shoulder and Elbow Surgeons) scales present in some of these studies. A total of 271 patients were included, of whom 144 underwent hemiarthroplasty and 127 total shoulder arthroplasty. Table 1 shows the articles selected and their outcomes (Table 1) [13,14,15,16,17].
Table 1: Studies analyzed and their outcomes.
| Study | Approach Surgical | Patients F/M | Results |
| Schoch et al | Hemiarthroplasty Total arthroplasty | 100/41 | VAS; Degree of elevation, external and internal rotation of the limb; Level of patient satisfaction |
| Feeley et al | Hemiarthroplasty Total arthroplasty | 26/38 | ASES; Degree of elevation, external and internal rotation of the limb; complications |
| Orfaly et al | Hemiarthroplasty Total arthroplasty | 14-Jul | ASES; VAS; Degree of elevation, external and internal rotation of the limb; complications |
| Mansat et al | Hemiarthroplasty Total arthroplasty | 12-Jul | Degree of elevation, external and internal rotation of the limb; degree of satisfaction |
| Rhee et al | Hemiarthroplasty Total arthroplasty | Dec-14 | VAS; UCLA score; ASES; Degree of elevation, external and internal rotation of the limb; degree of satisfaction |
VAS - Pain Analog Scale; ASES - American Shoulder and Elbow Surgeons.
Tables 2 and 3 show the range of motion of patients undergoing hemiarthroplasty and total arthroplasty, respectively, for the treatment of osteonecrosis of the humeral head (Table 2 and Table 3) [10,11,12,13,14].
Table 2: Analysis of patients’ range of motion undergoing hemiarthroplasty for the treatment of osteonecrosis of the humeral head.
| Study | Sample | Age average | Limb elevation degree -rotation (level vertebra) | External rotation degree | Level |
| Schoch et al | 67 patients | 56 years | 147º +- 38 | 61° +- 26 | L3 |
| Feeley et al | 35 patients | 57 years old | 150º+-8.0 | 54.4º +- 5.7 | L1 |
| Orfaly et al | 15 patients | 54 years | 129th +- 5.0 | 45º +- 4.2 | T12 |
| Mansat et al | 14 patients | 56 years | 110º +- 5 | 28.5º +- 4 | L3 |
| Rhee et al | 13 patients | 55 years | 123.1º +-5 | 43.2°+-4 | L3 |
Table 3: Analysis of patients’ range of motion undergoing total arthroplasty for the treatment of osteonecrosis of the humeral head.
| Study | Sample | Age average | Limb elevation degree -rotation (level vertebra) | External rotation degree | Level |
| Schoch et al | 67 patients | 56 years | 132º +- 43 | 53° +- 25 | L3 |
| Feeley et al | 35 patients | 57 years old | 90º +- 12.6 | 50º +- 8.5 | L1 |
| Orfaly et al | 15 patients | 54 years | 123º +- 5.6 | 44th +- 5.0 | T12 |
| Mansat et al | 14 patients | 56 years | 110º +- 5.0 | 28.5° +- 4.0 | L3 |
| Rhee et al | 13 patients | 55 years | 96.9°+-5 | 43.2°+-4 | L3 |
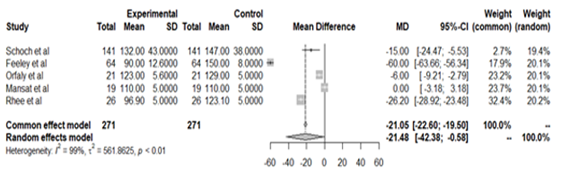
Figure 2 shows a comparative analysis of the range of motion of limb elevation in patients undergoing total arthroplasty and humeral head hemiarthroplasty (Figure 2). [13,14,15,16,17].
Figure 2: Analysis comparative range of motion when lifting the limb of patients undergoing total arthroplasty and hemiarthroplasty of the humeral head.
The study by Schoch et al10 showed that the main causes of humeral osteonecrosis were steroid use (56 percentage) and idiopathic causes (26 percentage). The VAS scores of patients treated with HA and TSA were similar (2.3 +- 1.5 versus 2.5 +- 1.3), while 85% and 77% of these patients, respectively, were very satisfied with their post-operative results. Feeley et al11 demonstrated a better range of movement in patients undergoing hemiarthroplasty (150º+-8.0 versus 90º +- 12.6), and the complication rate was significantly higher with TSA (22 percentage) than with HA (8 percentage). With regard to the ASES score, a tool for assessing shoulder function, the data showed 70.8 +- 7 and 52.3+-6.1, after HA and TSA, respectively. The study by Orfaly et al12 showed similar results between the range of motion of the limb of patients undergoing hemiarthroplasty and total arthroplasty (129º +- 5.0 versus 123º +- 5.6). With regard to the VAS scale for pain, the TSA and HA groups obtained values of 18 and 17, respectively. While the study by Mansat et al13, evaluating the degree of limb mobility after hemiarthroplasty and total arthroplasty, showed insignificant differences between the findings, with a degree of limb elevation after surgery for corticosteroid causes (main causes) of 110°, 28.5° for external rotation and internal rotation for L3.
Finally, Rhee et al14 demonstrated a mean VAS pain score, UCLA score (functional shoulder assessment scale) and ASES score with significant improvement from 6.3, 11.6 and 35.0 before surgery to 2.2, 28.9 and 82.6 at the final follow-up assessment. A greater angle of elevation was observed in patients who underwent hemiarthroplasty compared to those who underwent total arthroplasty (123.1° versus 96.9°), and there were no differences in the other ranges of movement.
Discussion
The therapeutic indication for the treatment of osteonecrosis of the humeral head takes into account the age range and staging of the disease. The studies showed that TSA was preferentially used in older patients, with HA being preferred in cases where the glenoid cartilage remains intact or almost intact. Both HA and TSA provided significant pain relief and limb function, with HA being related to a greater degree of limb mobility. However, the reoperation rate is more common in partial arthroplasties. Furthermore, core decompression is safe and effective for treating low-grade osteonecrosis of the humeral head, while hemiarthroplasty and total shoulder arthroplasty should be considered for high-grade osteonecrosis. However, there is still controversy over the choice of arthroplasty type according to stage. The most important factor in deciding the type of arthroplasty is the incongruity of the AGJ or arthritic change of the glenoid due to long-term problems, glenoid wear in patients with HA and glenoid loosening in patients with TSA can be problematic and necessitate revision surgery. In one scientific study, the choice between HA and TSA was based on intraoperative findings; when four-fifths or more of the glenoid area was covered by cartilage, HA was performed. However, TSA was performed in patients with severe glenoid wear or humeral head subluxation in the deficient glenoid area. In general, hemiarthroplasty is indicated when glenoid wear is minimal or non-existent, while total shoulder arthroplasty is usually indicated when both the humerus and glenoid are involved [18,19].
Hemiarthroplasty is widely accepted for patients with intact rotator cuffs and no or little glenoid wear, two circumstances present in osteonecrosis. However, in young individuals with wear of this joint, there is no agreement on the ideal type of arthroplasty [20,21]. In young, active patients, HA is effective, especially in those with minimal glenoid wear. However, the results are potentially less pain relief, less mobility, lower patient satisfaction and a more constant need for revision surgery. Possible advantages include less blood loss, shorter surgical time and a technically easier surgical procedure.22, 2:. A known complication of HA is the development of erosion of the glenoid cavity, which is the main cause of unfavorable evolution in the medium and long term, culminating in progressive loss of range of motion, decreased shoulder function, pain and, consequently, increased dissatisfaction rates for the operated individual. It is also the main reason for clinical deterioration and revision to total arthroplasty [24,25,26,27,28,28,30]. With regard to TSA, it causes a risk of loosening of the glenoid component, which becomes increasingly common over the years and correlates with increased pain and decreased functionality. In addition, changes in bone stock are common after the procedure and complicate revision surgery. Therefore, the selection of the best type of prosthesis should be based on reasons that influence the survival of the prosthesis and functional results [31,32]. Both total and partial arthroplasty have shown satisfactory clinical results in short, medium and long-term follow-up, with both HA and TSA considerably improving the clinical function of affected patients after 8.2 years. Revision surgeries due to glenoid wear were low, while complications following TSA were high, with 32 percentage presenting with glenoid loosening and 26 percentage of patients undergoing revision surgery [33,34,35].
Conclusion
Hemiarthroplasty revisions due to glenoid erosion are not routine, while total shoulder arthroplasty revisions are more common and require greater technique, as well as greater care with bone stock, due to the risk of intraoperative fracture. This is why HA should preferably be indicated in young patients without glenoid injury. TSA, on the other hand, is indicated for grade V or other stages in conjunction with a damaged glenoid. But both allow for good clinical results and therefore patient satisfaction.
This study has no conflicts of interest
This study received no financial support from public, commercial or non-profit sources.
References
- Na SS, Kim DH, Choi BC, Cho CH. (2022). Outcomes and complications after arthroplasty in patients with osteonecrosis of humeral head- systematic review. J Orthop Sci, 28(4):772-777.
Publisher | Google Scholor - Smith KL, Matsen FA 3rd. (1998). Total shoulder arthroplasty versus hemiarthroplasty. Current trends. Orthop Clin North Am, 29(3):491-506.
Publisher | Google Scholor - Le Coz P, Herve A, Thomazeau H. (2021). Surgical treatments of atraumatic avascular necrosis of the shoulder. Morphologie, 105(349):155-161.
Publisher | Google Scholor - Alkhateeb JM, Arafah MA, Tashkandi M, Al Qahtani SM. (2021). Surgical treatment of humeral head avascular necrosis in patients with sickle cell disease: a systematic review. JSES Int, 5(3):391-397.
Publisher | Google Scholor - Franceschi F, Franceschetti E, Paciotti M, et al. (2017). Surgical management of osteonecrosis of the humeral head: a systematic review. Knee Surg Sports Traumatol Arthrosc, 25(10):3270-3278.
Publisher | Google Scholor - Harreld KL, Marker DR, Wiesler ER, Shafiq B, Mont MA. (2009). Osteonecrosis of the humeral head. J Am Acad Orthop Surg. 17(6):345-355.
Publisher | Google Scholor - Lin CC, Karlin E, Boin MA, et al. (2021). Operative Treatment of Proximal Humeral Fractures with Reverse Total Shoulder Arthroplasty in Patients ≥65 Years Old: A Critical Analysis Review. JBJS Rev, 10(5):21.00245.
Publisher | Google Scholor - Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC et.al. (2020). declaração PRISMA 2020: diretriz atualizada para relatar revisões systematics [The PRISMA 2020 statement: an updated guideline for reporting systematic reviewsDeclaración PRISMA 2020: una guía actualizada para la publicación de revisiones sistemáticas]. Rev Panam Salud Publica, 30(46):112.
Publisher | Google Scholor - (2012). The Cochrane Collaboration. History. Oxford (UK): The Cochrane Collaboration.
Publisher | Google Scholor - FRANCESCHI, Francesco et al. (2017). Surgical management of osteonecrosis of the humeral head: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy, 25:3270-3278.
Publisher | Google Scholor - SMITH, Robert G. et al. (2008). Shoulder hemiarthroplasty for steroid-associated osteonecrosis. Journal of shoulder and elbow surgery,17(5):685-688.
Publisher | Google Scholor - SARRIS, Ioannis. WEISER, Robert. SOTEREANOS, Dean G. (2004). Pathogenesis and treatment of osteonecrosis of the shoulder. Orthopedic Clinics, 35(3):397-404.
Publisher | Google Scholor - Schoch BS, Barlow JD, Schleck C, Cofield RH, Sperling JW. (2016). Artroplastia do ombro para osteonecrosis atraumática da cabeça úmera. J Ombro Cotovelo Surg, 25(2):238-45.
Publisher | Google Scholor - Feeley BT, Fealy S, Dines DM, Warren RF, Craig EV. (2008). Hemiarthroplasty and total shoulder arthroplasty for avascular necrosis of the humeral head. J Shoulder Elbow Surg,17(5):689-694.
Publisher | Google Scholor - Orfaly RM, Rockwood CA Jr, Esenyel CZ, Wirth MA. Shoulder arthroplasty in cases with avascular necrosis of the humeral head. J Shoulder Elbow Surg, 16(3):27-32.
Publisher | Google Scholor - Mansat P, Huser L, Mansat M, Bellumore Y, Rongieres M, Bonnevialle P. (2005). Shoulder arthroplasty for atraumatic avascular necrosis of the humeral head: nineteen shoulders followed up for a mean of seven years. J Shoulder Elbow Surg, 14:114-120.
Publisher | Google Scholor - Rhee SM, Kim DH, Rhee YG, Cho CH. (2023). Long-term outcomes after humeral head replacement and total shoulder replacement for osteonecrosis of the humeral head: a mean follow-up of 8 years. Arch Orthop Trauma Surg, 143(8):4597-4604.
Publisher | Google Scholor - MIYAZAKI, Alberto Naoki et al. (2021). Osteonecrose da cabeça do úmero: Avaliação dos resultados da artroplastia parcial com seguimento minimum de 10 anos. Revista Brasileira de Ortopedia, 56:91-97.
Publisher | Google Scholor - MERCADO, Juan Sebastián Castillo et al. (2022). Atraumatic osteonecrosis of the humeral head: pathophysiology and current concepts of evaluation and treatment. JSES Reviews, Reports, and Techniques, 2(3):277-284.
Publisher | Google Scholor - Walch G, Boileau P, Noël E. (2010). Shoulder arthroplasty: evolving techniques and indications. Joint Bone Spine, 77:501-505.
Publisher | Google Scholor - Boileau P, Sinnerton RJ, Chuinard C, Walch G. (2006). Arthroplasty of the shoulder. J Bone Joint Surg Br, 88:562-575.
Publisher | Google Scholor - Levy O, Tsvieli O, Merchant J, et al. (2015). Surface replacement arthroplasty for glenohumeral arthropathy in patients aged younger than fifty years: results after a minimum ten-year follow-up. J Shoulder Elbow Surg, 24:1049-1060.
Publisher | Google Scholor - ABLOVE, Robert H. (2016). Total shoulder arthroplasty: historical perspective, indications, and epidemiology. Techniques in Shoulder & Elbow Surgery,17(1):5-6.
Publisher | Google Scholor - SCHOCH, Bradley S. et al. (2016). Shoulder arthroplasty for post-traumatic osteonecrosis of the humeral head. Journal of Shoulder and Elbow Surgery, 25(3):406-412.
Publisher | Google Scholor - Herschel R, Wieser K, Morrey ME, Ramos CH, Gerber C. et.al. (2023). Risk factors for glenoid erosion in patients with shoulder hemiarthroplasty: an analysis of 118 cases. J Shoulder Elbow Surg, 26(02):246-252.
Publisher | Google Scholor - Schoch BS, Barlow JD, Schleck C, Cofield RH, Sperling JW. (2016). Shoulder arthroplasty for atraumatic osteonecrosis of the humeral head. J Shoulder Elbow Surg, 25(02):238-245.
Publisher | Google Scholor - Mansat P, Huser L, Mansat M, Bellumore Y, Rongières M. et.al. (2005). Shoulder arthroplasty for atraumatic avascular necrosis of the humeral head: nineteen shoulders followed up for a mean of seven years. J Shoulder Elbow Surg, 14(02):114-120.
Publisher | Google Scholor - Gadea F, Alami G, Pape G, Boileau P, Favard L. (2012). Shoulder hemiarth- roplasty: outcomes and long-term survival analysis according to etiology. Orthop Traumatol Surg Res, 98(06):659-665.
Publisher | Google Scholor - Smith RG, Sperling JW, Cofield RH, Hattrup SJ, Schleck CD. (2008). Shoulder hemiarthroplasty for steroid-associated osteonecrosis. J Shoulder Elbow Surg, 17(05):685-688
Publisher | Google Scholor - Bryant D, Litchfield R, Sandow M, Gartsman G, Guyatt G. et.al. (2005). A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoul- der arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am, 87:1947-1956.
Publisher | Google Scholor - GADEA, F. et al. (2012). Shoulder hemiarthroplasty: outcomes and long-term survival analysis according to etiology. Orthopaedics & Traumatology: Surgery & Research, 98(6)659-665.
Publisher | Google Scholor - Feeley. B.T, Fealy. S, Dines. D.M, Warren. R.F, Craig. E.V. (2008). Hemiarthroplasty and Total Shoulder Arthroplasty for Avascular Necrosis of the Humeral Head. J. Shoulder Elb. Surg, 17:689-694.
Publisher | Google Scholor - Mansat. P, Huser. L, Mansat. M, Bellumore. Y, Rongières. M. et.al. (2005). Shoulder Arthroplasty for Atraumatic Avascular Necrosis of the Humeral Head: Nineteen Shoulders Followed up for a Mean of Seven Years. J. Shoulder Elb. Surg,14:114-120.
Publisher | Google Scholor - Parsch. D, Lehner. B, Loew. M. (2003). Shoulder Arthroplasty in Nontraumatic Osteonecrosis of the Humeral Head. J. Shoulder Elb. Surg, 12:226-230.
Publisher | Google Scholor