Research Article
Fractional CO2 Laser with Platelet-Rich Plasma Versus Fractional CO2 Laser with Topical Insulin in The Treatment of Postacne Atrophic Scars
- Fatma Faisal El Dakrory *
- Shaymaa El-Mongy Mohammed
- Sawsan Kassem Gomaa
- Shereen Ezz al regal Alashry
Dermatology, Andrology & STDs Department, Faculty of Medicine, Mansoura University, Egypt.
*Corresponding Author: Fatma Faisal El Dakrory, Dermatology, Andrology & STDs Department, Faculty of Medicine, Mansoura University, Egypt.
Citation: F.F.E. Dakrory, S.E.M Mohammed, Sawsan K Gomaa, S.E. Alashry. (2023). Fractional CO2 Laser with Platelet-Rich Plasma Versus Fractional CO2 Laser with Topical Insulin in The Treatment of Postacne Atrophic Scars. Dermatology Research and Reports, BRS publishers. 2(2); DOI: 10.59657/2993-1118.brs.23.007
Copyright: © 2023 Fatma Faisal El Dakrory, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 18, 2023 | Accepted: August 12, 2023 | Published: August 18, 2023
Abstract
Background: Postacne atrophic scars (PAS) are a common acne consequence. When paired with a fractional CO2 laser, topical insulin and PRP may both help. Objective: To compare the effectiveness of a fractional CO2 laser plus PRP versus a fractional CO2 laser with TI in the management of PAS.
Methods: This research was conducted on 20 patients suffering from PA atrophic scars. Enrolled patients received four sessions of FCL plus topical PRP in addition to FCL+ topical insulin on left as well as right sides of the face, respectively, at monthly intervals. One month following the fourth session, the last assessment was completed. Side effects were recorded. Patients were encouraged to use photoprotective precautions.
Results: There was a statistically significant difference of acne scar grade post treatment between right and left side. Higher improvement is detected among right side treatment than left side. There was a statistically considerable difference between studied groups regarding improvement degree between both sides. For right side 10% excellent improvement, 65% good and 25% fair improvement versus 75% fair improvement and 25% good improvement for left side (P=0.001*).
Conclusions: In PAS of skin-of-color populations, TI and PRP coupled with Fractional CO2 laser may both provide improvement with an excellent safety profile. However, the ease of access, low cost, and noninvasive characteristics of TI make it preferable to PRP. The degree of improvement was statistically considerably greater with TI than with PRP (P=0.001*).
Keywords: PAS (Postacne atrophic scars); TI (Topical insulin); PRP (platelet-rich plasma)
Introduction
Postacne atrophic scars are a common acne consequence. Peels, platelet-rich plasma, subcision, dermabrasion, lasers, punch methods, and fillers are effective in 2 PAS; nevertheless, most of these are linked with dyspigmentation and scarring, restricting their general usage, particularly in those with darker skin [1]. Fractional CO2 laser (FCL) monotherapy is a well-recognized scar therapy method. This treatment is relied on the fractional photo thermolysis theory. It generates small thermal wounds in order to cause homogenous thermal damage at a certain depth beneath the skin [2].
Insulin functions not only as a glucose-regulating hormone, but also as a growth-like factor and cytokine regulator, which may speed up wound healing [3]. In diabetic and nondiabetic people, topical insulin (TI) stimulates wound healing without changing blood glucose values [4]. TI stimulates tahe phosphatidyl inositol 3-kinase (PI3K)/protein kinase B (PKB/Akt) pathways to enhance vascular endothelial growth factor. Following TI, enhanced synthesis and maturation of collagen fibers, mostly type III, takes place in a basket weave-like organization (normal skin) rather than a crisscross way (scar). Thus, combining PRP or insulin with a fractional CO2 laser boosts PAS improvement [5].
The aim of the study
To compare the effectiveness of Fractional CO2 laser with platelet-rich plasma vs. a Fractional CO2 laser with topical insulin in the management of post acne atrophic scars.
Patients and Methods
This study was conducted on 20 patients with PA atrophic scars. All patients were enrolled from those attending the outpatient clinic of Dermatology, Andrology & STDs Department, Mansoura University Hospitals, Mansoura, Egypt, in the period from July 2022 to February 2023.
Inclusion criteria: Recently diagnosed cases exhibiting atrophic scars on any part of the face. Fitzpatrick skin types IV to VI in age group from 18 to 35 years. The patient had not previously received scar therapy within two months before the research.
Exclusion criteria: Active acne or infections, or both, on the face; patients using systemic retinoids in the previous 6 months or topical retinoids in the last 2 weeks.
Patients underwent ablative or non-ablative laser skin resurfacing within the previous year or laser therapy for acne scar. Patients who are suffering from another dermatological disease. Patients receiving systemic treatment. History of keloidal tendency, bleeding disorders, and deranged blood glucose levels. History of chronic liver or autoimmune diseases, collagen vascular disease. Patients with chronic debilitating diseases, uncontrolled systemic infection and a history of malignancy. Patients with herpes, HIV and HBV infection. Pregnant and lactating females or who were using hormonal treatment, all were excluded from the study.
The included patients were exposed to the following:
- History taking: A detailed history including age, sex, family history, duration of disease, BMI, smoking, other dermatological diseases and previous medical history.
- Clinical examination: Complete general and dermatological exams, including skin phototyping using Fitzpatrick's skin type categorization [6]. The existence of post inflammatory hyperpigmentation, hypertrophic scars, and keloids was assessed. Scar distribution (on the forehead, cheeks, chin, or arms), texture, color, atrophy, and overall look were all considered while evaluating post-acne scars.
- Dermoscopic examination: all patients were examined by dermoscopy.
The subtypes of atrophic acne scars (ice pick, boxcar, and rolling scars) were studied. Furthermore, the color of acne scars, whether skin-colored, erythematous, or hyperpigmented, was observed in order to identify any change in scar color at the conclusion of therapy. Finally, atrophic acne scars were graded using the Goodman and Baron scaring grading method [7]. This approach categories acne scars into grades 1-4 depending on scar severity (macular, mild, moderate, and severe, respectively): lesions with a combination of two patterns are classed based on the most severe pattern. The scar is further classified according to its distribution, with "A" indicating focused involvement of a single aesthetic region and "B" indicating two to three distinct sites of involvement.
The included patients were categorized into the following groups according to the type of therapy:
Group 1: 20 patients were treated with FCL with PRP on the left side.
Group 2: the same 20 patients were treated with FCL with topical insulin (TI) on the right side.
Enrolled patients received four sessions of FCL+ topical PRP in addition to FCL+ topical insulin on left and right sides of the face, respectively, at monthly intervals. One month following the fourth session, the last assessment was completed. Side effects were recorded. Patients were encouraged to use photoprotective precautions.
A 30-W FIRE-XEL ablative FCL device from Bison Medical, licensed by the Korean FDA, was employed as a fractional CO2 device.
PRP preparation: A 2 stage centrifuging procedure were done utilizing an R8C centrifuge device (REMI Sales & Engineering Ltd. Goregaon (East), Mumbai – 400063. Maharashtra, India) to obtain PRP. Whole blood samples (10 mL) were drawn from patient’s medial cubital vein taking into account the infection control measures and transferred to a vial containing an anticoagulant (Acid citrate dextrose). It was centrifuged at 1500 rpm for 10 min. Platelet-poor plasma, PRP, and a few RBCs were aspirated into a new tube and centrifuged at 3000 rpm for 20 min. The middle layer that contains the PRP were aspirated for topical use instantly after the FCL treatment on left side of the face. The patient stayed in the recumbent position until the site of PRP application dried up [8].
Topical insulin: Preprocedural and post procedure blood glucose levels were measured, topical fast-acting insulin (40 IU/ml of human insulin and 0.3% meta cresol), we used Human act rapid insulin 100 IU/ml® solution (Act rapid; Novo 4 Nordisk Pharmaceuticals Ltd, Bagsvaerd, Denmark, was applied to the RT side of the face in 40 unit (dilution was 40IU of insulin +60 IU of distilled water) [9].
Adverse effects on both sides of the face were noted which are easily avoided by post session precautions. Post-session advice: Patients were advised to use sunscreens throughout the daytime and bland emollient throughout night time, and mild cleansers for facewash. They were warned about the possibility of developing transitory erythema, edema, hyperpigmentation, and dryness.
The degree of improvement, as perceived by the patients, was evaluated. At the last session, patients were asked about their level of satisfaction with the outcomes in contrast to the pre-treatment condition on both sides, and they were assessed on a five-point scale as excellent, good, fair, or bad according to the client and doctor satisfaction questionnaire (CSQ) [10].
Statistical analysis and data interpretation
SPSS software, version 18 (SPSS Inc., PASW statistics for Windows version 18), was used to analyze the data. SPSS Inc. is based in Chicago. Numbers and percentages were used to describe qualitative data. For non-normally distributed data, the median (minimum and maximum) and mean were used to characterize quantitative data. Standard deviation for normally distributed data after the Shapiro Wilk test for normality. The significance of the results obtained was determined at the (0.05) level. Whitney Mann The U test was developed to compare two sets of data that were not regularly distributed. To compare more than two examined eras, the Wilcoxon signed Rank test was utilized. Spearman's rank order correlation is used to assess the strength and direction of a linear relationship between two non-normally distributed continuous and/or ordinal variables.
Results
Mean age of the studied cases was 25.05 with 5.43 SD ranging from 17 to 35 years, 70percentage females and 30% males, Table 1.
Table 1: sociodemographic characteristics of the studied cases.
| N=20 | % | |
| Age /years | ||
| Mean ± SD | 25.0±5.43 | |
| (Min-Max) | (17-35) | |
| Sex | ||
| Male | 6 | 30.0 |
| Female | 14 | 70.0 |
| Occupation | ||
| Student | 2 | 10.0 |
| Employee | 11 | 55.0 |
| Manual worker | 3 | 15.0 |
| Housewife | 4 | 20.0 |
| Residence | ||
| Mansoura | 15 | 75.0 |
| Mahla | 5 | 25.0 |
| Marital status | ||
| Single | 13 | 65.0 |
| Married | 7 | 25.0 |
All cases had gradual onset, progressive course of disease with median disease duration is 9.5 years ranging from 2 to 20 years, Table 2.
Table 2: disease characteristics among studied cases.
| N=20 | % | |
| Onset Gradual | 20 | 100.0 |
| Course(progressive) | 20 | 100.0 |
| Duration / years Median (Min-Max) | 9.5(2-20) | |
75% of the studied cases had disfigurement, 5% positive associated symptoms including itching and pain, Table 3.
Table 3: clinical characteristics of the studied cases.
| N=20 | % | |
| Disfigurement | ||
| No | 5 | 25.0 |
| Yes | 15 | 75.0 |
| Associated symptoms | ||
| -ve | 19 | 95.0 |
| +ve | 1 | 5.0 |
| Presence of active acne | 0 | 0.0 |
| Renal & hepatic | 0 | 0.0 |
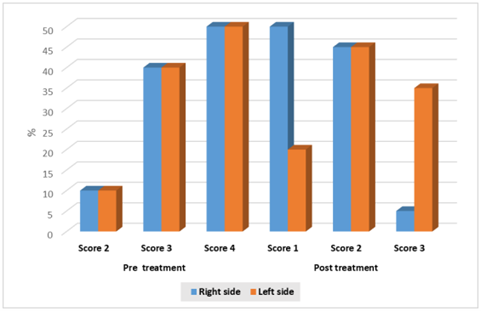
Table 4: Distribution of the studied cases according to scar score before and after treatment.
| Score of scars | Right side | Lift side | Test of significance (Mann Whitney U test) |
| Pre treatment | |||
| Mild | 2(10.0) | 2(10.0) | P=1.0 |
| Moderate | 8(40.0) | 8(40.0) | |
| Severe | 10(50.0) | 10(50.0) | |
| Post treatment | |||
| Very mild | 10(50) | 4(20) | Z=3.46 |
| Mild | 9(45) | 9(45) | P=0.001* |
| Moderate | 1(5) | 7(35) | |
| Wilcoxon signed | Z=4.06 | Z=4.13 | |
| rank test | P<0> | P<0> | |
Table 5: distribution of the studied cases according to scar score before and after treatment.
| Improvement grade | Right side N=20(%) | Left side N=20(%) | Test of significance (Steuart Maxwell test) |
| Grade | |||
| Fair | 5(25.0) | 15(75.0) | P=0.001* |
| Good | 13(65.0) | 5(25.0) | |
| Excellent | 2(10.0) | 0 | |
Table 6: comparison of side effects between treatment sides.
| Side effects | Right side N=20(%) | Left side N=20(%) | Test of significance (Mann Whitney U test) |
| Erythema | 0 | 0 | P=1.0 |
| Oedema | 1(5.0) | 1(5.0) | P=1.0 |
| Infection | 5(25.0) | 1(5.0) | P=0.07 |
| Hyperpigmentation | 0 | 0 | P=1.0 |
| Pain | 0 | 0 | P=1.0 |
| Total complications | |||
| No | 14(70.0) | 18 (90) (90) | P=0.113 |
| Yes | 6(30.0) | 2(10) | |
Table 7: comparison of patient satisfaction between treatment sides.
| Patient satisfaction | Right side N=20(%) | Left side N=20(%) | Test of significance (Mann Whitney U test) |
| Poor | 0 | 1(5.0) | P=0.006* |
| Fair | 2(10.0) | 5(25.0) | |
| Good | 3(15.0) | 10(50.0) | |
| Excellent | 15(75.0) | 4(20.0) |
Figure 1: acne scar score distribution among right and left sides pre and post treatment.
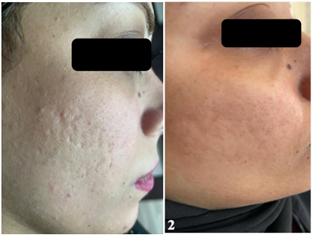
Figure 2: Case 1, 22 years old male grade 4 before ttt and grade 2 after ttt on RT side (TI).
Figure 3: Grade 4 before ttt and grade 3 after ttt on LT side (PRP).
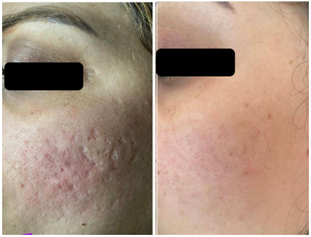
Figure 4: Case 2, 28 years old female grade 4 before ttt and grade 1 after ttt on RT side (TI).
Figure 5: Grade 3 before ttt and grade 2 after ttt on left side (PRP).
Discussion
In the existing study, a statistically significant higher improvement was detected among right side than left side (p<0 P=.01) P=.03)>
Abbas et al., (2022) [11] compared the anti-scarring effects of topical insulin and micro needling to that of topical vitamin C and micro needling for post-acne scars. The overall improvement was greater on the vitamin C-treated side (p = 0.0036). In another investigation, insulin intralesional injection or topical spraying inhibited the formation of hypertrophic scars (HS) after wound injuries in sensitive patients [12]. In our study, a statistically significant difference between studied groups as regard patient satisfaction with excellent satisfaction was detected among right side treatment than left side (75% & 20%, respectively) (P=0.006*).
Opposing to our study, Abbas et al., (2022) [11] used a four-grade Likert scale (bad, fair, good, or outstanding) to measure their acne scarring relative to baseline. Fourteen patients, 14/30 (46.7%), expressed great satisfaction with their acne scarring on the right (vitamin C-treated) side, whereas only two, 2/30 (6.7%), reported excellent satisfaction on the left (insulin-treated) side. On the left (insulin treated) side, nine patients (9/30) reported a bad result. Patients were much more satisfied with the vitamin C-treated (right) side than with the insulin-treated (left) side (p 0.001). This might be related to distinct patient groups and varied TI administration procedures (low TI concentration).
In the current study, non-statistically significant difference between studied groups as regard side effects of treatment. Incidence of complications was 30% among right side versus 10% for left side in the form of erythema, oedema, infection, pain and hyperpigmentation.
Adverse effects in Pawar& Singh, (2021) [5] study included transient erythema (n=8), pain (n=6), and edema (n=3); however, there was no dyspigmentation or scarring. Pawar& Singh, (2021) [5] did not observe any changes in blood glucose levels as in our study. In Abbas et al., (2022) [11] study, no major adverse events were registered. The most common side effect reported was edema followed by erythema. There was no difference in side effects seen on either side (p=0.97) as in our study. No adverse outcomes stayed at the last follow up.
In our study, there was non-statistically significant difference between studied groups as regard dermoscopic findings of PAS before and after ttt either by PRP or TI. This is in agreement with Chae et al., (2015) [13] who studied ttt of PAS with fractional photo thermolysis with non-statistically significant difference between before and after ttt groups.
Conclusion
In PAS of skin-of-colour populations, TI and PRP coupled with Fractional CO2 laser may both provide improvement with an excellent safety profile. However, the ease of access, low cost, and non-invasive characteristics of TI make it preferable to PRP. The degree of improvement was statistically considerably greater with TI than with PRP (P=0.001*). Likewise, excellent satisfaction was detected among TI side treatment than PRP side (75% & 20%, respectively) (P=0.006*).
Ethical consideration: The study protocol was approved by Institution Research Board (IRB) of Mansoura Medical College (MS.22.09. 2131.R1). All individuals in this study provided written informed consent. All levels of the study protected confidentiality and personal privacy. All data were only utilized for research reasons.
Recommendations
Further studies with, larger case numbers, longer duration of treatment and follow up are recommended for better evaluation of long-term effect of the treatment.
References
- Ghanian S & Wambier, C. G. (2021). Response to “Microneedling with autologous platelet rich plasma versus microneedling with topical insulin in the treatment of postacne atrophic scars: A simultaneous split-face comparative study.” Journal of the American Academy of Dermatology, 85(6):395-396.
Publisher | Google Scholor - Sharma S, Kaur J, Kaur T & Bassi R. (2021). Fractional carbon dioxide laser versus combined fractional carbon dioxide laser with platelet-rich plasma in the treatment of atrophic post-acne scars: a split-face comparative study. Journal of Cutaneous and Aesthetic Surgery, 14(1):41.
Publisher | Google Scholor - Wang J & Xu J. (2020). Effects of topical insulin on wound healing: a review of animal and human evidences. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 13:719.
Publisher | Google Scholor - Sridharan K & Sivaramakrishnan, G. (2017). Efficacy of topical insulin in wound healing: A preliminary systematic review and meta‐ analysis of randomized controlled trials. Wound Repair and Regeneration, 25(2):279-287.
Publisher | Google Scholor - Pawar M & Singh M. (2021). Microneedling with autologous platelet-rich plasma versus microneedling with topical insulin in the treatment of postacne atrophic scars: a simultaneous split-face comparative study. Journal of the American Academy of Dermatology, 84(3):810-811.
Publisher | Google Scholor - Fitzpatrick T. B. (1988). The validity and practicality of sun-reactive skin types I through VI. Archives of Dermatology, 124(6):869–871.
Publisher | Google Scholor - Goodman G. J & Baron J. A. (2006). Postacne scarring–a quantitative globalscarring grading system. Journal of Cosmetic Dermatology, 5(1):48-52.
Publisher | Google Scholor - Zhu J.-T, Xuan M, Zhang Y.-N, Liu H.-W, Cai J.-H, Wu Y, Xiang X.-F, Shan G.-Q & Cheng B. (2013). The efficacy of autologous platelet-rich plasma combined with erbium fractional laser therapy for facial acne scars or acne. Molecular Medicine Reports, 8(1):233-237.
Publisher | Google Scholor - Abdelkader D. H, Osman M. A, Elgizaway S. A, Faheem A & McCarron P. A. (2016). The role of insulin in wound healing process: mechanism of action and pharmaceutical applications. Journal of Analytical & Pharmaceutical Research, 2(1).
Publisher | Google Scholor - Larsen D. L, Attkisson C. C, Hargreaves W. A & Nguyen T. D. (1979). Assessment of client/patient satisfaction: development of a general scale. Evaluation and Program Planning, 2(3):197-207.
Publisher | Google Scholor - Abbas M. A. M, Elgamal E. E. A. E, Zaky M. S &Elsaie M. L. (2022). Microneedling with topical vitamin C versus microneedling with topical insulin in the treatment of atrophic post‐ acne scars: A split‐ face study. Dermatologic Therapy, 35(5):15376.
Publisher | Google Scholor - Hu Z, Tang B, Guo D, Zhang J, Liang Y, Ma D & Zhu J. (2014). Expression of insulin‐ like growth factor‐ 1 receptor in keloid and hypertrophic scar. Clinical and Experimental Dermatology, 39(7):822-828.
Publisher | Google Scholor - Chae WS, Seong JY, Jung HN, Kong SH, Suh HS & Choi YS. (2015). The consideration of dermoscopic findings during atrophic acne scar treatment: a pilot study. Korean journal of dermatology, 23-29.
Publisher | Google Scholor