Case Report
False-Negative MRI in Acute Ischemic Stroke of Young Adult: Case Report and Literature Review
1.Faculty of Medicine and Biomedical Sciences of Garoua, Cameroon.
2.Neurosurgery Department, Yaounde Central Hospital, Cameroon.
3.Neurosurgery Unit, Essos Hospital Centre, Yaounde, Cameroon.
4.Cardiology Department, Douala Gyneco-Obstetric and Pediatric Hospital, Cameroon.
5.Imaging Department, Yaounde General Hospital, Cameroon.
6.Imaging Department, Yaounde Military Hospital, Cameroon.
*Corresponding Author: Alain Jibia, Faculty of Medicine and Biomedical Sciences & Neurosurgery, Yaounde Central Hospital, Unit, Essos Hospital Centre, Yaounde, Cameroon.
Citation: Jibia A, Yomba A Michel, Asseme N Nadege, Haoua T. (2023). False-Negative MRI in Acute Ischemic Stroke of Young Adult: Case Report and Literature Review, Journal of Neuroscience and Neurological Research, BRS Publishers. 2(2); DOI: 10.59657/2837-4843.brs.23.010
Copyright: © 2023 Jibia Alain, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 06, 2023 | Accepted: July 24, 2023 | Published: July 28, 2023
Abstract
The diagnosis of acute cerebral stroke is currently based on radiologic and clinical evidences: a persistent sudden neurological disorder associated to concordant radiological finding. We report a radio clinical unconformity of an acute cerebral infarction with normal conventional MRI. A 3 months wet-nurse of 30-year-old presented a brutal left hemiparesis preceded 2 days before by a transitory aura. The initial MRI done after 36 hours of delay did not show any damage. The subsequent cardiovascular etiological record was normal. We noticed a partial recovery of the neurodeficit after 1 week, and total recovery after intensive physiotherapy. We discussed about transient ischemic attack (TIA) without lesion. A very small volume of cerebral infarction can be initially MRI-undetectable corresponding to a false-negative. The diffusion weighted imaging (DWI) with fine cuts and decreased apparent diffusion coefficient (ADC) allows accurate diagnosis.
Keywords: dwi-mri; false-negative; ischemic stroke; normal mri
Introduction
Ischemic stroke is the second leading cause of death worldwide according to the WHO [1]. The positive diagnosis, essentially radio clinical, is based on a sudden persistent neuro deficiency, particularly in a person with cardiovascular risk factors, and a consistent lesion focus found on magnetic resonance imaging (MRI) [2,3]. However, although this is very sensitive, there are false negatives that could make early initial management perplexing [4,5,6,7]. We report the case of a lady who presented a constituted ischemic stroke with normal cerebral MRI. This is a rare unusual radio clinical presentation and the first of its kind in Africa with regard to Literature.
Case Report
Mrs. D.L is a right-handed 30-year-old nurse anaesthetist, G4P4 nurse for 3 months, with a history of eclampsia with coma 10 years ago (G1P0) with no history of contraceptives oral intake, but a period of personal stress. She was admitted to the emergency room for a sudden fall from her height and brief loss of consciousness, which had occurred a few hours earlier, without any notion of comitiality. She had presented 2 days before a faintness such as intense chest pain with left hemiparesthesia, feelings of heaviness in the upper limb and suffocation, isolated mild systolic arterial high blood pressure (HBP) at 140/80 mm Hg. Acetylsalicylic Acid-based self-medication (Aspirin®) 200 milligrams (mg) was made and a complete regression of symptoms noted by the patient 1 hour later. A consultation in the emergency room followed and was unremarkable, in particular the electrocardiogram (ECG) performed. A second dose of Aspirin® will be taken the next day, after a new feeling of suffocation.
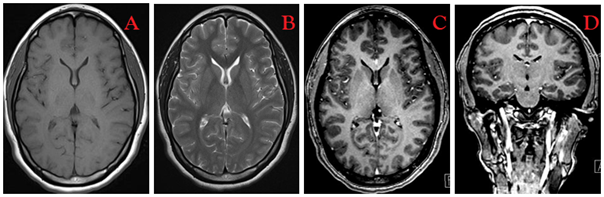
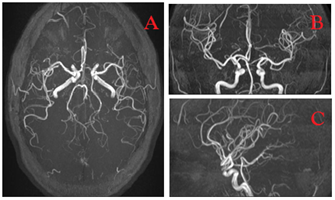
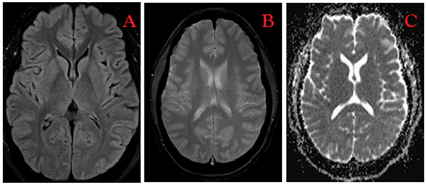
The clinical examination on admission found normal alertness with predominantly crural left hemiparesis (2/5 and 3/5, according to the MRC_ Medical Research Council scale), without central facial paralysis with normal initial blood pressure. The initial NIHSS (National Institute of Health Stroke Score) score was 7. The emergency brain scan was normal, as was the ECG. Biology essentially evoked HDL hypercholesterolemia at 0.78 g/l. The cerebral MRI performed approximately 36 hours after the onset signs, according to the T2 FLAIR, T2 Gradient Echo T2*, Diffusion, ADC (Apparent Diffusion Coefficient), T1, T2, TOF (Time of Flight) sequences, found no radiological lesion (Figures 1,2,3). An analgesic treatment was started with Atorvastatin 10 mg/day and resumption of Aspirin 100 mg/day. Transcranial Doppler Ultrasound or Electroencephalogram was not performed. The subsequent cardiological consultation revealed an isolated tachycardia. Supra-aortic trunks and cardiac Doppler found no significant abnormality. A clear regression of the neurological deficit (4/5 and 3/5) was noted one week later. Functional rehabilitation initiated secondarily allowed better motor recovery with slight limping and resumption of activities. The mRS (modified Rankin Scale) score was of 1.
Figure 1: MRI of the patient without radiological particularities. Axial T1 (A), Axial T2 (B), Axial T1 Gadolinium (C), Coronal T1 Gadolinium (D) sections.
Figure 2: 3D TOF MRI showing the 2 vascular systems without focal point of obstruction. Axial (A), Coronal (B), Sagittal (C) reconstructions.
Figure 3: MRI without radiological particularities. Slices: Axial Diffusion (A), Axial T2* (gradient echo) (B), Axial ADC (Apparent Diffusion Coefficient) (C).
Discussion
The risk of occurrence of an ischemic stroke after a transient ischemic attack (TIA) is 2.5–5% at 48 hours, as noted in our case [8]. Currently, a distinction is made between TIA with or without radiological lesion with regressive neuro deficit in 1 hour (without exceeding 24 hours) [8]. Mrs D.L, 30, presented at 3 months of her delivery a persistent hemiparesis over 1 week and partially improved at 1 month; therefore, it was of a constituted ischemic stroke with undetermined etiology. The cerebral thrombophlebitis or brain focal infarction were not objectified on the initial MRI; they are plausible aetiologies evoked in postpartum or in patients with eclampsia history. The incidence of cerebral ischemia during pregnancy or at 2 weeks of delivery is 43 per million deliveries per year [9]. Thirty to fifty percent of cerebral ischemia in young subjects has no identified cause. The main ones are cervical arterial dissection or embolic heart disease, especially rheumatic valve disease [10].
Cerebral MRI remains the gold standard for the early positive diagnosis of cerebral infarction in the acute phase [11,12,13]. From the outset, it is preferred to CT and allows the visualization of: recent ischemia (Diffusion MRI), arterial occlusion (Angio-MR) and the hypo perfused area (Perfusion MRI) [12]. This possible examination in our context is not systematically done urgently and is expensive to perform, justifying the 36-hour delay observed in our case. According to the American Heart Association (AHA) in the event of clinical suspicion of acute stroke, the rapid application protocol in neurovascular emergency proposes the performance of an MRI not to exceed 20 minutes and comprising DWI (Diffusion-Weighted Imaging)–T2*–FLAIR (FLuid-Attenuated-Inversion-Recovery)–AMR 3D TOF (Angio-Magnetic Resonance Three-Dimensional Time of Flight) ± Transcranial Echo-Doppler [12,13].
The diffusion sequence is the current gold standard because it allows very early diagnosis (from the 30thminute) of cytotoxic cerebral edema with a drop in the apparent diffusion coefficient (ADC)–by reduction of the movement of the proton in the edema – and to some extent the penumbra zone, better assessed by perfusion MRI [12,13,14]. The B2000 optimized diffusion sequence in thin slices makes it possible to find small cerebral infarcts (lacunae) in the acute phase, if conventional MRI proves to be non-contributory [7]. False-negatives in diffusion MRI are possible with a prevalence of 1.5–25.6%, due according to several studies to the latency of this sequence and to the site of the lesion [4]. This can be noticed equally and/or both for small posterior lesions and large anterior ones [5]. It also takes several tens of minutes for the cytotoxic edema to be hyperintense [14].
The T2 Gradient Echo sequence (T2*) establishes the difference between hematoma and ischemia. The FLAIR sequence also better assesses subcortical or paraventricular ischemia, due to the better contrast between the black cerebrospinal fluid and the hyperintense ischemic lesion. The only particularity is its long acquisition. The Angio-MR_3D TOF sequence looks for intracranial vascular steno-occlusive atheromatous or dissection lesions [15].
The MRI performed in all the sequences can be normal or subnormal in the case of acute ischemic stroke, as in our clinical case (Figures 1,2,3). Three possible reasons: a very small volume lesion (≈ 1 millilitre = ml), the low signal/noise ratio observed 24 hours after the onset of the signs, brainstem signal artefacts [4,7]. Several studies propose in this case the repetition of this examination as much as possible as long as the initial neuro deficit persists [4,5,7]. This was not done in our case. Bergot et al found a lesion in the territory of the anterior cerebral artery after 48 hours of a normal initial MRI, related to a recent ischemic stroke [4]. Chang W-L et al reported a diagnostic delay of 14 days (336 hours) for left ischemic lacunae of the brainstem and the cerebellar hemisphere [16]. This repeated MRI, difficult in the context of limited healthcare costs, could be planned weekly or substituted for a brain CT-scan if neurological worsening.
Cerebral MRI in the clinical situation of stroke has a triple purpose diagnostic, therapeutic and prognostic [7,12]. Its normal aspect in the acute phase can be confusing to the treatment or even to the prognosis; the clinic should therefore always take precedence over the paraclinical to avoid any aggravation or dramatic recurrence. Our patient continued long-term platelet aggregation inhibitor treatment and lipid-lowering drug as recommended during an established ischemic stroke [8]. The indication for thrombolysis by recombinant tissue plasminogen activator (rt-PA or Alteplase) was exceeded at the time of diagnosis.
Conclusion
Ischemic stroke cannot be formally excluded simply because of a normal initial MRI. The non-negligible false-negatives justify its constant repetition in fine sections, especially if the neuro deficit persists, and an appropriate medication in advance to limit possible complications.
References
- Organisation Mondiale De La Sante. (2020). Les 10 Principales Causes de Mortalite. https://www.who.int/fr/news-room/fact-sheets/detail/the-top-10-causes-of-death
Publisher | Google Scholor - Boulois G. (2018). Imagerie des AVC Ischémiques a la Phase Aigue Objectif Recanalisation.
Publisher | Google Scholor - Oppenheim C, Naggara O, Arquizan C, Brami-Zylberberg F, Mas JL, Meder JF, Fredy D. (2005). MRI of acute ischemic stroke. J Radiol. 86(9 Pt2):1069-1078.
Publisher | Google Scholor - Bergot N, Kosowski J, Thiebaud PC. (2018). False-Negative MRI in Acute Ischemic Stroke. Ann Fr Med Urgence. 8:187-188.
Publisher | Google Scholor - Oppenheim C, Stanescu R, Dormont D, Crozier S, Marro B, Samson Y, Rancurel G, Marsault C. (2000). False-negative diffusion-weighted MR findings in acute ischemic stroke. AJNR Am J Neuroradiol. 21(8):1434-40.
Publisher | Google Scholor - Bulut HT, Yildirim A, Ekmekci B, Eskut N, Gunbey HP. (2014). False-negative diffusion-weighted imaging in acute stroke and its frequency in anterior and posterior circulation ischemia. J Comput Assist Tomogr. 38(5):627-633.
Publisher | Google Scholor - Lemahafaka G, Camara A, Rajaonarison L, Vallet F. (2016). Ischemic stroke despite normal brain MRI: about a case. Pan Afr Med J. 25:22.
Publisher | Google Scholor - National Agency for Accreditation and Evaluation in Health (Anaes). (2014). Diagnosis and immediate treatment of transient ischemic attack in adults.
Publisher | Google Scholor - Di X, Mai H, Zheng Z, Guo K, Morse An, Liu H. (2018). Neuroimaging findings in women who develop neurologic symptoms in severe preeclampsia with or without eclampsia. Hypertens Res. 41(8):598-604.
Publisher | Google Scholor - Khammassi N, Sassi Yb, Aloui A, Kort Y, Abdelhedi H, Cherif O. (2015). Ischemic stroke in Young Patients: about 6 cases. Pan Afr Med J. 22:142.
Publisher | Google Scholor - Lovblad KO, Altrichter S, Viallon M, Sztajzel R, Delavelle J, Vargas Mi, El-Koussy M, Federspiel A, Sekoranja L. (2008). Neuro-imaging of cerebral ischemic stroke. J Neuroradiol. 35(4):197-209.
Publisher | Google Scholor - De Roquefeuil E, Molinier S, Dousset V. (2014). Neuroimaging of stroke. La Lettre du Neurologue. 18(4):121-128.
Publisher | Google Scholor - High Authority Of Health (Has). (2009). Stroke : early management (alert, pre-hospital phase, initial hospital phase, indications for thrombolysis). HAS/Good Professional Practices Department.
Publisher | Google Scholor - Adam G, Ferrier M, Patsoura S, Gramada R, Meluchova Z, Cazzola V, Darcourt J, Cognard C, Viguier A, Bonneville F. (2018). Magnetic resonance imaging of arterial stroke mimics: a pictorial review. Insights Imaging. 9(5):815-831.
Publisher | Google Scholor - Gauvrit JY, Leclerc X, Leys D, Pruvo JP. (2003). Sub-acute phase of cerebral ischemia: value of MRI. J Radiol. 84(2):121-129.
Publisher | Google Scholor - Chang WL, Lai JC, Chen RF, Hu HH, Pan CS. (2017). Case Report of False-Negative Diffusion-Weighted Image of Brain Magnetic Resonance Imaging (MRI) in Acute Ischemic Stroke. Am J Case Rep. 18:76-79.
Publisher | Google Scholor