Research Article
Exploratory Laparotomy Diagnostic and Management Mainstay in A Case of Huge Ovarian Cyst Torsion on Late Post Postpartum Period, At Resource Limited Set Up of Leku General Hospital, Sidama, Ethiopia, Case Report
- Asfaw Kibret *
- Efrem Bayu
General Hospital, Ethiopia.
*Corresponding Author: Asfaw Kibret, General Hospital, Ethiopia.
Citation: Kibret A., Bayu E. (2023). Exploratory Laparotomy Diagnostic and Management Mainstay in A Case of Huge Ovarian Cyst Torsion on Late Post Postpartum Period, At Resource Limited Set Up of Leku General Hospital, Sidama, Ethiopia, Case Report. Clinical Obstetrics and Gynecology Research, BioRes Scientia Publishers. 2(1):1-5. DOI: 10.59657/2992-9725.brs.23.005
Copyright: © 2023 Asfaw Kibret, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 25, 2023 | Accepted: September 08, 2023 | Published: September 15, 2023
Abstract
Background: Huge ovarian cyst is a rare occurrence in postpartum period. Once existing ovarian cyst passes the pregnancy period, it is a risk for torsion on postpartum days when the gravid uterus involuted. Here we present a case of huge ovarian cyst torsion on late post-partum period which is diagnosed and managed in our resource limited set up.
Case presentation: This is a case of 30yrs old female patient who is on her 30th post-partum date after she gave alive fetus at home. Then she noticed that her abdomen failed to decrease after delivery and waited for spontaneous decrement and lastly, she visited health center for the newly developing worsened pain since last 3 days of her presentation to health center.
Conclusion: This case reports that huge ovarian cyst accompanied pregnancy might not affect the pregnancy and vaginal delivery is possible but torsion is common in this case due to the involution of the postpartum uterus. Exploratory laparotomy in low resource set up is still the main stay for diagnosis and management of such emergency cases.
Keywords: ovary; delivery; ultrasound
Introduction
In the world 0.2-2% pregnancies are accompanied by ovarian cysts of which most of it is functional cysts and regresses in the 2nd TM pregnancy. They rarely become large and their persistence is their organic nature. Those cysts are generally identified incidentally during ante natal surveillance of the pregnancy obstetrics ultrasound. But in low resource set up and in area where antenatal follow up is poor it is not identified early till it is symptomatic [1,2]. Actually, ovarian torsion adnexal torsion is performed by twisting axis defined by the lumbo-ovarian ligament and the tubo-ovarian ligament. The pathogenic mechanism would be the displacement of the adnexa secondary to the physiological involution of the uterus and the relaxation of the supporting tissues, increasing the mobility of the mass and the risk of the adnexal torsion [2,3].
Case Report
this is a 32yrs old lady with 3 alive parities and currently she is on her 30th post postpartum dates after she gave birth her last baby at home. she gave birth after she stayed on laboring pain of 10hrs.she told that her baby was delivered spontaneously and cried immediately and the cord was clumped traditionally. the placenta was also delivered spontaneously. After her delivery she waited for spontaneous decrement of her abdominal size but failed. She had no ANC follow up due to her remote village far from health facility. Currently she presented with history of failure of the abdominal size after delivery of her fetus and the new onset of abdominal discomfort and pain which started since last one week and worsened since last 3 days. she had 2 episodes of vomiting. For these complain she visited health center which was 40km away from her village and the health center referred her to the leku general hospital for further investigation and management.
Upon arrival she was acutely sick looking her vital signs were BP=90/60Mmgh, PR=110bpm, RR=24br/min, T=37.6, PSO2=94%. She had moderately pale conjunctiva, dry buccal mucosa, on abdominal examination she looks late term gravid mother, with minimally tender huge abdominopelvic mass, which was regular, per vaginal digital examination shows closed cervix. On laboratory investigation revealed CBC (WBC- 17000, HCT-23.2%, PLT-198 x10*3). On bedside ultrasound there was huge abdomen pelvic cystic mass, which was difficult to measure the boarder, the uterus was empty, there was no septation on the cystic mass.
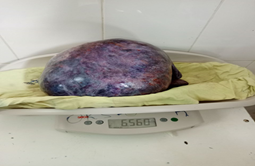
Then the patient was decided to had gynecologic emergency and prepared for OR and taken to OT. Under General anesthesia mid-line exploratory laparotomy was done and intra-operatively there was 6.5kg (Fig.1a) cystic rt adnexal mass which was trotted 720 degree over the adnexal pedicle (Figure 1b). It was gangrenous. Rt adnexectomy done. The contra lateral adnexal was healthy looking. The mas was sent for histopathology and result came back with serous cyst adenoma with no malignant features. The post operative course was uneventful and patient discharged on 5th post operation day.
Figure 1(a): The 6.5kg cystic ovarian torsioned mass after adnexectomy.
Figure 1(b): Intra operative picture of the torsion.
Discussion
Adnexal torsion is considered when there is rotation of at least one turn of the ovary and part of Fallopian tube around its vascular pedicles. It is the rare cause of gynecologic emergency. Risk factors for ovarian torsion includes pregnancy, ovarian stimulation, previous abdominal surgery, and tubal ligation. However, torsion is frequently associated with ovarian pathologies that result in enlarged ovaries. The most frequently encountered pathology is that of an ovarian dermoid, although other structures include paramos/tubal cysts, follicular cysts, endometriomas and serous/ mucinous cystadenoma [2,3,4].
窗体底端
Mature teratomas are by far the most common persistent adnexal masses during pregnancy. Ovarian cysts of the huge are extremely rare in the gravid-puerperium period. They represent less than 1% of the set of cysts associated with pregnancy The first two trimesters of pregnancy are the preferred periods for the occurrence of adnexal torsion (70% to 90% of cases), but it can sometimes occur during the third trimester of pregnancy, although the increase in the size of the uterus in the third trimester reduces the mobility of the ovary. In the postpartum period, ovarian torsion mainly occurs during the three weeks following vaginal delivery. Studies suggested that this might be due to the involution of the post partial uterus and relaxation of the adnexal ligaments which predispose sudden torsion of the ovarian cyst that was there during the pregnancy course or developed after the delivery [5].
The main feature of torsion is ovarian enlargement due to venous/lymphatic engorgement, edema, and hemorrhage. Secondary signs include free pelvic fluid, an underlying ovarian lesion, reduced or absent vascularity and a twisted dilated tubular structure corresponding to the vascular pedicle. Adnexal torsion is commonly unilateral, with a slight (3:2) right-sided predilection (presumably due to the protective effects of the sigmoid colon on the left) [6, 8]. Currently different imaging modalities give diagnostic clues for ovarian cyst torsion. Ultrasound is the commonest and most of the time the initial imaging modalities of choice [7, 9].
Sonographic features include: enlarged (>4 cm) ovary, if the ovaries are normal in size and symmetric, torsion is unlikely. Ovarian edema variable echogenicity (hypo- or hyperechoic) a long-standing infarcted ovary may have a more complex appearance with cystic or hemorrhagic degeneration, peripherally displaced follicles with hyperechoic central stroma, follicular ring sig, midline ovary position. Doppler findings in torsion are widely variable :little or no ovarian venous flow (common; sensitivity of 100% and specificity of 97%) absent arterial flow (a less common, sign of poor prognosis),absent or reversed diastolic flow, normal vascularity does not rule out intermittent torsion, normal Doppler flow can also occasionally be found due to dual supply from both the ovarian and uterine arteries, whirlpool sign of twisted vascular pedicle, an underlying ovarian lesion may be seen (possible lead point for torsion),ovary tenderness to transducer pressure, free pelvic fluid may be seen in >80% of cases.
CT is useful for ruling out ovarian torsion if normal ovary/adnexa is seen on ultrasound. There are many features seen on CT which favor ovarian torsion: enlarged ovary, involved ovary shifted to the midline and most often anterior to the uterus, lead mass may be identified, twisted pedicle in the adnexa, uterus displaced to the involved side, minimal free fluid, fat stranding in the adnexa. The appearance of a twisted ovarian pedicle on CT is pathognomonic for ovarian torsion. HU >50 on non-contrast CT suggests hemorrhagic necrosis. A lack of contrast enhancement may be seen. Hemorrhagic necrosis is a sign of nonviability. An underlying ovarian lesion may be present (lead point for torsion) [7]. But these all be entertained in accessible set up. Otherwise, it is better to proceed based on the patient condition and presentation. As in our case, patients may present in emergency condition. In that case you wouldn’t have time to further investigate, since you had no access for ideal imaging and specialist hands of radiology.
Conclusion
This case reports that huge ovarian cyst accompanied pregnancy might not affect the pregnancy and vaginal delivery is possible but torsion is common in this case due to the involution of the postpartum uterus. Exploratory laparotomy in low resource set up is still the main stay for diagnosis and management of such emergency cases. Moreover, further delay is not necessary in the low resource setups and better to proceed with exploratory laparotomy even with minimal suspicion of torsion in the presence of cysts which are huge.
Acknowledgment
We would like to thank all those leku general hospital professionals who were involved on the management of the patient. Special thanks for anesthesia professionals (Ayalew and Tariku) for their commitment and cooperation to give anesthesia in the absence of blood product. Last but not least special gratitude for nurses and MCH midwives who were dedicated to follow the post operative courses of the patient.
References
- Daykan, Y., Bogin, R., Sharvit, M., Klein, Z., Josephy, D., et al. (2019). Adnexal Torsion during Pregnancy: Outcomes after Surgical Intervention—A Retrospective Case- Control Study. Journal of Minimally Invasive Gynecology, 26:117-121.
Publisher | Google Scholor - Eichenberger-Gautschi, T., Smith, A. And Sayasneh, A. (2018) Ovarian Masses in Pregnancy: A Single Centre Retrospective Study. British Journal of Medical Practitioners, 11(1).
Publisher | Google Scholor - Kiemtoré, S., Zamané, S.K., Sawadogo, Y.A., Sansan, S.R., Komboigo, E., Ouédrao-go, A. and Bonané, B. (2019). Diagnosis and Management of a Giant of Ovarian Cyst in the Gravid-Puerperium Period: A Case Report. BMC Pregnancy and Childbirth, 19(523).
Publisher | Google Scholor - Bassi, A., Czuzoj-Shulman, N. and Abenhaim, H.A. (2018). Effect of Pregnancy on the Management and Outcomes of Ovarian Torsion: A Population-Based Matched Cohort Study. Journal of Minimally Invasive Gynecology, 25(1260-1265).
Publisher | Google Scholor - Tanaka, Y., Koyama, S. and Shiki, Y. (2015). Torsion of a Normal Ovary during the Early Postpartum Period. CRSLS MIS Case Reports
Publisher | Google Scholor - Condous, G., Khalid, A., Okaro, E. and Bourne, T. (2004). Should We Be Examining the Ovaries in Pregnancy? Prevalence and Natural History of Adnexal Pathology Detected at First Trimester Sonography.
Publisher | Google Scholor - Ultrasound in Obstetrics & Gynecology, 24:62-66.
Publisher | Google Scholor - Ovarian torsion | Radiology Reference Article
Publisher | Google Scholor - Huchon C, Staraci S, Fauconnier A. (2010). Adnexal torsion: a predictive score for pre-operative diagnosis. Hum Reprod., 25(9):2276-2280.
Publisher | Google Scholor - Shadinger LL, Andreotti RF, Kurian RL. (2008). Preoperative sonographic and clinical characteristics as predictors of ovarian torsion. J Ultrasound Med Off J Am Inst Ultrasound Med. 2008;27(1):7-13.
Publisher | Google Scholor