Research Article
Exercise Testing in Children with Cerebral Palsy
1Research Laboratory, Adaptations Physiologiques a Exercice et Readaptation a effort, Faculty of Sciences and Sport, University of Picardie Jules Verne, Amiens, France.
2Faculty of Kinesiology and Physical Education, University of Toronto, PO Box 521, Brackendale, Canada.
Reprint requests to: Said Ahmaidi, Faculty of Sciences and Sport, Amiens, France.
*Corresponding Author: Angeline Nsenga Leunkeu, Faculty of Sciences and Sport, Amiens, France.
Citation: Angeline N Leunkeu, Roy J Shephard, S Ahmaidi. (2022). Exercise Testing in Children with Cerebral Palsy. Journal of Neuroscience and Neurological Research, BRS Publishers. 1(1); DOI: 10.59657/2837-4843.brs.22.002
Copyright: © 2022 Angeline Nsenga Leunkeu, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 01, 2022 | Accepted: September 26, 2022 | Published: October 07, 2022
Abstract
Objectives: To examine if cardiorespiratory requirements assess during the 6-minute walking test (6WT) and the cardiopulmonary exercise test (CPET) before and after training are the same in children with cerebral palsy (CP).
Methods: 24 children with CP (16 boys and 8 girls, with the mean age of 14.2±2 years (10 to 16 years) classified at gross Motor Function Classification System level I and II were recruted from a school for special education in France. Participants were randomly assigned both the cardiopulmonary exercise test (CPET) and the 6WT and were divided to either training group (n = 12) or the control group (n = 12). The training group met twice per week for 40 minutes of exercise training.
Results: Cardiorespiratory data did not differ between the CPET and the 6WT before training (VO2 Peak: p=0.86; VE Peak: p=0.87 and HR Peak: p= 0.41) and after training (p=0,41, p=0,26 et p=0,65) respectively.
Conclusions: These findings demonstrate that cardiorespiratory responses obtained during the 6WT and the CPT before and after training did no differ in children with cerebral palsy.
Keywords: children with cp; cardiopulmonary exercise test; 6wt; exercise training
Introduction
Exercise fitness is commonly used to assess the functional status of children with cerebral palsy (CP) (Nsenga Leunkeu et al. 2017, Tim Takken et al. 2017, Zwinkels Marenka et al. 2017). Some physiotherapists used the six-minute walk test (6WT) or the cardio-Pulmonary exercise test (CPET) in interventions (Nsenga Leunkeu et al. 2017 et 2012, Tim Takken et al. 2017), or before and after certain surgery or treatments in children with CP (Nsenga Leunkeu et al. 2017 …….). However, there is paucity studies which think to explorate the 6WT and the CPET before and after training. Whereas it could be informative to provide an excellent tool in clinical rehabilitation. We had already investigated the 6WT and the CPET in children with CP (Nsenga et al 2012 and 2013). Even if the tests are used in rehabilitation programs, we did not compare the both tests before and after training. However, it could be useful to help and provide some information keys to clinicians. So that, the choice of each test can match with some type of CP children that professional want to evaluate. Meanwhile, no data are yet available concerning the comparison of the 6MWT and the CPET in children with cerebral palsy. By doing the comparison of the 6MWT and the CPET in children with CP GMFCS levels I and II, the medical staff who work for the rehabilitation and treatments in this population of children can feel free to realize a choice which is appropriated.
The purpose of this study is to provide the comparison of the cardio respiratory parameters of the 6WT and the CPET in children with CP before and after training; and then it overviews of its current applications in each type of children with CP.
Materials and Methods
Participants
Twenty-four children with CP (age, 14.2±2 years; weight, 45.5±7.8 kg; height, 154±11 cm) familiarized with cycling activity participated in this study. All were volunteers from local specialized school. All subjects underwent a cardiopulmonary test (CPET) and had a standardized 6WT with gas exchange measurement with a portable gas analyser (Cosmed K4b2, Cosmed, Rome, Italy). All children were spastic classified at level I or II on the gross motor function classification system (GMFCS) as expanded and revised for children > 12 years (Palissano et al. 2000). Twelve subjects were randomly selected and (age, 12±4 years; weight, 42.5±6.3 kg; height, 160±13 cm) underwent a second 6WT to assess its reproducibility. There was a one-week gap between the 6WT tests. Two groups of twelve children matched for age (14±2 years); weight (43±5.7 kg), height (158±14 cm), sex (6 boys and 3 girls), type of CP, and GMFCS participated in the exercise training study. One group underwent the 8-week training programme and the other group represented a control group, who continued with their normal therapy. Twenty children were classified as hemiplegic (involvement of one side of the body) and four were classified as diplegic (involvement of the lower part of the body). The participants were independent ambulators and were able to follow simple verbal commands. Participants were excluded if they had had orthopedic surgery or neurosurgery and/or botulinium toxin injection (s) within 6 months prior to study entry or cardiac or respiratory conditions that could negatively be affected by exercise. The study was approved by a local ethics committee and in accord with the ethical standard of the Helsinki Declaration of 1975 and 1983 and in an investigation that met the ethical standards of this journal as detailed by Harris and Atkinson [14]. Children were excluded if they undergone a surgical procedure influencing mobility during the past year, were taking medication that could affect muscular function. A medical examination was performed and anthropometric data were collected on each subject. The clinical characteristics of the children with CP are stated in Table 1. A physician assessed the spasticity of each child, using the method of Ashworth (1964) [15]. All children were independently ambulatory and maturity was assessed by Tanner staging [16,17]. For children, an informed consent was obtained from the parents as well as from the child. Before the testing sessions, a medical examination was performed and their anthropometric data were measured.
| Characteristic | Children and adolescents with CP (controls, n=10) | Children and adolescents with CP (training group, n=10) |
| Age (years) | 14±1.8 | 14±1.9 |
| Body mass (kg) | 45.4±6.3 | 45.5±5.7 |
| Height (m) | 1.58±0.12 | 1.59±0.13 |
| Sex: boys/girls | 8 boys / 4 girls | 8 boys / 4 girls |
| Hemiplegia | 10 | 10 |
| Diplegia | 2 | 2 |
| GMFCS | Level I: 9, level II: 3 | Level I: 9, level II: 3 |
Table 1: Clinical characteristics of children and adolescents with CP GMFCS levels I and II (Values are mean values ± SD).
Methods
Cycle-ergometer exercise testing
Exercise testing was performed on a leg cycle ergometer (Ergometer 824 E, Monark Exercise AB, Kroonsväg 1, S-780 50 Vansbro, Sweden) using previously determined protocol (Nsenga et al 2013). Thorough familiarization and habituation procedures were followed as recommended (Nsenga et al 2013). Children with CP underwent two cycle ergometer exercise testing sessions. The first test was a habituation test, which was also used to check the protocol and to determine whether the children with CP needed to be attached to the pedals (Rogers et al 2008). One week later, children then underwent an incremental protocol exercise test on the cycle-ergometer with an initial power of 30 W and was increased thereafter by 15 W every minute. The pedalling rate was fixed at 50 rpm and the cadence was maintained by using a metronome. The feet were fixed to the pedals by velcro strapping. Individual protocols were constructed such that the total exercise time ranged between 6 and 12 minutes. All the tests were preceded by a 5 min warm-up period. Vigorous verbal encouragements were given throughout the tests to achive maximal effort. During the CPET, cardiorespiratory gas exchange measurements were obtained with the portable gas analyzer (Cosmed K4b2, Cosmed, Rome, Italy). The inspiratory air flows and the fraction of expired O2 (Fe O2) and CO2 (Fe CO2) were calculated by computer every 5 respiratory cycles. One-minute averages were then established for minute ventilation (VE: L. min-1, BTPS), O2 uptake (VO2: L min-1, STPD), CO2 production VCO2 (L.min-1, STPD) ventilatory equivalent for O2 (VE. VO2-1), and CO2 (VE. CO2-1) and breathing frequency (f, cycle. min-1). The test ended when fatigue or dyspnea occurred making the child stop the effort. The VO2 peak obtained at the end of maximal exercise testing was considered as the maximal VO2 uptake. Exercise tolerance and cardiorespiratory requirement were assessed through the values obtained at maximal effort: oxygen uptake (VO2), ventilation (VE), heart rate (HR). At the end of the test, subjects had 5 minutes of passive recovery.
The 6-Minute Walking Test
Before they began the 6WT, children with CP were fitted with a portable gas analyzer Cosmed K4b2, (Cosmed, Rome, Italy) to assess respiratory gas exchanges. Children with CP performed the 6WT between 2 lines set 20 m apart in the corridor, according to usual recommendation (Paap et al 2005). Cardiorespiratory requirement was assessed from cardiorespiratory gas exchange measures: oxygen uptake (VO2 in mL.kg-1min-1), ventilation (VE in L.min-1), and heart rate (in beats.min-1). Samples of these variables were taken during rest, 6 minutes during exercise, and 5 minutes during the recovery period. One-minute averages were then established for minute ventilation (VE: L. min-1, BTPS), O2 uptake (VO2: L min-1, STPD), CO2 production VCO2 (L.min-1, STPD) ventilatory equivalent for O2 (VE. VO2-1), and CO2 (VE. CO2-1) and breathing frequency (f, cycle. min-1). All tests were performed between 9: 00 AM and 12: 00 PM, in the same place, and followed the same protocol to control for circadian variation. Participants were instructed to walk as far as possible and to cover the distance as long as possible in 6 minutes. They also received vigurous verbal encouragements with the standard statements. Every 30 seconds subjects were advised of the remaining time and distance covered. They turned round a marker at each end of the 20 m. Furthermore, they did not use any orthotics or forearm crutches. The distance covered was measured at the end of the test.
Borg scale
Children quoted the exercise perception during both the 6WT and CPET at 5 minutes after the tests stopped. The Borg Scale with the level range from 6 to 20 was used (Borg 1982). Children were instructed to put a cross on a no graduated scale between two adjectives (very easy to very difficult) indicating the degree of the difficulty they felled during the tests.
Exercise training
The 6-Minute Walking Test
The group of the 12 children with CP were tested first and then have a training. Before the exercise training started, a trial of 30 minutes was performed by the training group to check out the speed used as training intensity. The training intensity used corresponded to the mean walking speed recorded on the 2 preceding 6 WT trials. Once the initial training walking speed was determined, the exercise training started 3 days after. Prior to and following the training programme, 6WT with cardiorespiratory gas analysis was conducted: oxygen uptake (VO2), ventilation (VE) and heart rate (HR) were measured. The training programme consisted of 30 min of walking three times per week for eight weeks. All training sessions were performed in the morning at 10:00 am on the same place (indoor) and according to the same protocol. Exercises sessions were performed 3 times per week, each on a separated day. The training was supervised by a physician and a paediatric physical therapist. To enhance the palatability of the training program, verbal encouragement was given to all the children to motivate them to finish the training session. To control for circadian variation, all tests were performed between 9: 00 am and 12: 00 (noon). To assess the effect of the eight weeks of exercise training, children were tested immediately after the eight-week using the 6 WT.
Cycle-ergometer exercise training
Training sessions were held three times per week, on separated days (Monday, Wednesday and Friday), 40 min (5 min of warm-up + 30 min of test + 5 min of recovery) at 50% the firsth and the second week, at 55% the third and the fourth week, at 60% the fifth and the sixth week and at 65% the seventh and the eighth week. Cycle ergometer training was chosen because most children with CP who have problems with movement coordination and equinus position of the foot find difficulty with the increasing speed and slope of treadmill exercise [21]. All training sessions were held at 10 am; immediately previously, the 12 children underwent 30 minutes of stretching of leg, thigh and arm muscles and breathing exercises under the supervision of the physiotherapist. They were given verbal encouragement to complete each training session. Training began with a 5 min warm up; they then undertook 30 minutes of pedalling (50 rpm with an initial power output of 30 w), 50% of the  O2 observed. The training load increased by 15 w every minute during the training. When they improved their performance, we increased the intensity 2 weeks by 2 weeks until they reached 8weeks. To assess the effect of the eight weeks of exercise training, children were tested immediately after the eight weeks.
O2 observed. The training load increased by 15 w every minute during the training. When they improved their performance, we increased the intensity 2 weeks by 2 weeks until they reached 8weeks. To assess the effect of the eight weeks of exercise training, children were tested immediately after the eight weeks.
Analysis of Data
All data are expressed as mean, standard deviation (SD). The normality of the data was tested using Kolmogorov-Smirnov test. The cardio respiratory data (Peak VO2, Peak VE and Peak HR) obtained during 6WT were compared to those assessed during the CPET before and after training period, and the Borg scale using an ANOVA (Statview 5.0, SAS, USA). For the correlation between the 6MWT and the CPET, we used Spearman correlation. A p value less than 0.05 was considered significant.
Results
Participants
A total of 28 participants were assessed for eligibility for this study: four participants did not complete the study. Two participants were awaiting surgery and were obligated to stop the training sessions before the end. Two participants did not wear a face mask because the thought of breathing through the mouthpiece frightened them. Twenty-four participants completed the entire study.
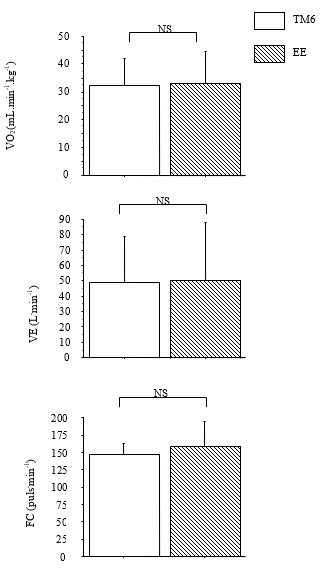
Comparison of the 6WT and the CPET cardio respiratory peak responses before training
The cardiorespiratory responses obtained during the 6WT and the CPET at the start of the 8 weeks in children with CP did not show significant differences for VO2 peak (6WT: 33.13±7.14 vs. CPET: 32.31±6.28 mL.kg-1.min-1, p=0.86); VE peak (6WT: 50.70±23.50 vs. CPET: 49.03±18.69 L.min-1, p=0.87) and HR peak (6WT: 156.62±22.42 vs. CPET: 148.40±25.1 beats.min-1, p= 0.41). Cardio respiratory peak values of the TM6 were 0.90 % for the VO2, 1,19 % for the VE et 1,05 % for the FC high to those that measured in CPET respectively. Moreover, there was a correlation for VO2 peak (r=0.80), VE peak (r=1), and HR peak (r=0.80). The results of the comparison of the cardio respiratory 6WT and the CPET before training are shown in figure 1.
Figure 1: Cardiorespiratory data of VO2peak (Fig. 3A), VEpeak (Fig. 3B) and HRpeak (Fig. 3C) measured during the 6WT and the CPET before training period. Values are mean values±standard deviation (SD). NS: no significant.
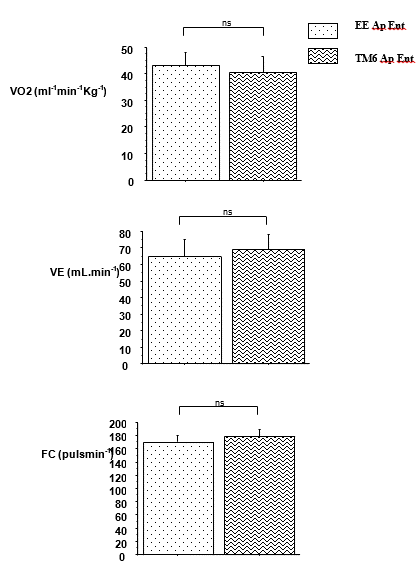
Comparison of cardio respiratory data of the 6WT and the CRET after training
Peak VO2, peak VE and peak FC of the 6WT after training did not differ from those of the CRET after training (p=0,41, p=0,26 et p=0,65) respectively. Cardio respiratory peak values of the 6MWT were 0.97 % for the VO2, 1,05 % for the VE et 1,04 % for the FC high to those that measured in CPET. Moreover, there was a correlation for VO2 peak (r=-0.40), VE peak (r=0.92), and HR peak (r=0.50). The results of the comparison of the cardio respiratory data 6WT and the CPET after training are shown in figure 2.
Figure 2: Cardiorespiratory data of VO2peak (Fig. 3A), VEpeak (Fig. 3B) and HRpeak (Fig. 3C) measured during the 6WT and CPET after training period. Values are mean values±standard deviation (SD). NS: no significant.
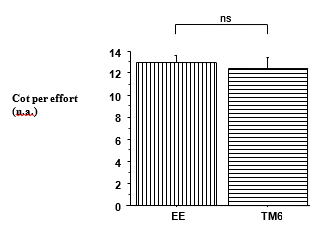
Figure 3: Borg scale
Discussion
This study demonstrates that the cardio respiratory responses obtained during the 6WT and the CPET were similar before and after training in children with CP classified at GMFCS level I and II.
The novelty of our investigation was to study comparison of the cardio respiratory requirement during the 6WT and the CPET before and after training. Results obtained demonstrated that the cardio respiratory responses obtained during the 6WT were similar to those obtained during the CPET. Indeed, O2 uptake, ventilation, heart rate responses and performance did not differ between these two tests. The results from the present study agree with the previous studies conducted in healthy children and children with other pathologic populations (Paap et al 2005). These also indicated the utility of the 6WT and the CPET for assessing functional capacity and cardio respiratory fitness in children with CP classified at GMFCS level I and II. Moreover, Borg scale outlined that the exercise perception was similar in both tests in children with CP. It could be assumed that, under this condition, the quotation of the perception of the effort confirmed the fact that cardio respiratory gas exchanged during the 6WT and the CPET are not different in children with CP GMFCS level I and II.
Given that physiotherapist and clinicians consider making the 6MWT a standard component of assessments for children and adolescents with CP at GMFCS levels I and II (A Nsenga Leunkeu et al 6MWT), the correlation with the CPET can be a type of measurements which potentially aid in treatment planning and in rehabilitation fitness in child with CP (A Nsenga Leunkeu IJSM). We previously found the effect of exercise training in children with CP GMFCS levels I and II during the 6MWT and the CPET (Archive, IJSM). We though and feared that CPET could not had been matched, and feet, and appropriate for children with CP, when we found that children with CP usually show quadriceps femoris weakness and thus a poor peak aerobic power when exercise isometric test (A nsenga Leunkeu et al). As it is well known that children and adolescents with CP are very weak and have lower performance, related fitness and cardiorespiratory fitness compared to children who are typically developing (ANsenga Leunkeu et al). Then, we focus our study on the comparison of cardiorespiratory data of the 6MW and the CPET instead of the treadmill because speed remained problematic for CP (Potter et al 2005). In the literature there is study assessed a new reference value for cardiorespiratory exercise testing in children (Joel Blanchard et al 2018). Whereas their study did not mention if their methodolody can be applied in children with cerebral palsy.
The current study compared the cardiorespiratory data (VO2, ventilation and heart rate) between the 6MWT and the CPET before and after training in children with CP. The results demonstrate that the cardio respiratory responses obtained when exercise during the both tests are similar. To the best of our knowledge, this is the first demonstration of the comparison of two methods of aerobic fitness: the 6MWT and the CPET in children with CP GMFCS level I and II. We found in Borg Scale that children with CP GMFCS level I and II felled the same effort during the 6MWT and the CPET. This result argued with the opinion that the 6MWT and the CPET can be both feasible in children with CP GMFCS levels I and II. We also found a correlation between the 6MWT and the CPET before and after training in those children. However, some studies only shown the comparison without correlation and more over without training. Whereas it is necessary and usual for the fiability and the validity of a test to assess the comparison before and after training. More over in clinical rehabilitation especially in children with cerebral palsy. We have now found that the 6MWT and the CPET in children with CP GMFCS level I and II could similarly assess aerobic fitness in children with CP GMFCS levels I and II. We provided and recommended to medical staff or searcher in children with CP to find this comparison like a good tool of evaluation in fitness, training and the improvement of the healthiness in their practices with their patients.
Conclusion
Viewed in concert the data of the 6MWT matched closely to the findings of the laboratory cycle-ergometer testing before and after training in children with CP GMFCS level I and II. Moreover, the 6MWT and the CPET can be used to evaluate cardiopulmonary function during rehabilitation program in children with CP GMFCS level I and II. These insights in the positive effects of exercise training should ideally lead to implementation in clinical practice.
Acknowledgements
Conflict of interest: none
Financial Disclosure
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of this manuscript.
Suppliers
Cosmed Srl, Via dei Piani di Monte Savello, 37, PO Box 3, Pavona di Albano, Rome, I-00040, Italy.
SAS Institute Inc, SAS Campus Dr, Cary, NC 27513, U.S.A.
References
- Angeline Nsenga Leunkeu, Daniel Keefer, Miladi Imed, Said Ahmaidi. (2010). Electromyographic Analysis of Skeletal Muscle Fatigue in children with cerebral palsy during isometric contraction of quadriceps. Journal of Child Neurology. 25(3):287-293.
Publisher | Google Scholor - Angeline Nsenga Leunkeu, Said Ahmaidi. (2012). Longitudinal assessment of muscle function and oxygen cost during isometric testing in children with cerebral palsy. Isokinetics and Exercise Science. (20)2:107-113.
Publisher | Google Scholor - A.L. Nsenga, R.J. Shephard, S. Ahmaidi. (2012). Aerobic training in children with cerebral palsy. Int J Sport Med. 33:1-5.
Publisher | Google Scholor - Angeline Nsenga Leunkeu, Roy J. Shephard, Said Ahmaidi. (2012). Six-Minute Walk Test in Children with Cerebral palsy Gross Motor Function Classification System Levels I and II: Reproducibility, validity and Training effects. Arch Phys Med Rehabil. 93:2333-2339.
Publisher | Google Scholor - Angeline N Leunkeu, Roy J Shephard and Said Ahmaidi. (2017). Optimizing Rehabilitation: The potential to Assess cardiorespiratory, Neuromuscular and Biomechanical Adaptations to Exercise of Children with Cerebral Palsy in the face of Intra-Individual Variation. J Nov Physiother Phys Rehabil. 4(2): 042-047.
Publisher | Google Scholor - Palisano R, Hana SE, Rosenbaum P, Walter SD, Wod EP, Raina PS, Galuppi BE. (2000). Validation of a model of Gross Motor Function for children with Cerebral Palsy. Phys Ther. 80:974-985.
Publisher | Google Scholor - Harris DJ, Atkinson G. (2011). Update-ethical standards in sport and exercise science research. Int J Sports Med. 32(11):819-821.
Publisher | Google Scholor - Ashworth B. (1964). Preliminary trial of carisoprodol in multiple sclerosis. Practitioner. 192:540-542.
Publisher | Google Scholor - Worley G, Houlihan CM, Herman-Giddens ME, O'Donnell ME, Conaway M, et al. (2002). Secondary sexual characteristics in children with cerebral palsy and moderate to severe motor impairement: a cross-sectional survey. Pediatrics. 110(5):897-902.
Publisher | Google Scholor - Henderson RC, Gilbert SR, Clement ME, Abbas A, Worley G, et al. (2005). skeletal maturation in moderate to severe cerebral palsy. Dev Med Child Neurol. 47(4):229-236.
Publisher | Google Scholor - Rogers A, Furler BL, Brinks S, Darrah JA. (2008). Systematic review of the effectiveness of aerobic exercise interventions for children with cerebral palsy: an AACPDM evidence report. Dev Med Child Neurol. 50:808-814.
Publisher | Google Scholor - Paap E, van der Net JV, Helders PJ, Takken T. (2005). Physiologic response of the six-minute walk test in children with juvenile idiopathic arthritis. Arthritis Rheum. 53:351-356.
Publisher | Google Scholor - Borg GA. (1982). Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 14:377-381.
Publisher | Google Scholor - Verschuren O, Ketelaar M, Takken T, Helders PJ, Gorter JW. (2008). Exercise programs for children with cerebral palsy: a systematic review of the literature. Am J Phys Med Rehabil. 87(5):404-417.
Publisher | Google Scholor - Blanchard J, Blais S, Chetaille P, Bisson M, Counil P. F. (2018). New reference values for cardiopulmonary exercice testing in children. Med Sci Sports Exerc. 50(6):1125.
Publisher | Google Scholor - Potter C, Unnithan VB. (2005). Interpretation and implementation of oxygen uptake kinetics studies in children with spastic cerebral palsy. Dev Med Child Neurol. 47:353-357.
Publisher | Google Scholor - Maltais D, Bor O, Pierrynowski M, Galea V. (2003). Repeated treadmill walks affect physiologic responses in children with cerebral palsy. Med Sci Sports Exerc. 35:1653-1661.
Publisher | Google Scholor - Enright PL. (2003). The six-minute walk test. Respir Care. 48:783-785.
Publisher | Google Scholor - Ethical Standards in Sport and Exercise Science Research. Int J Sports Med, 2009. 30:701-702.
Publisher | Google Scholor - ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. (2002). ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 166:111-117.
Publisher | Google Scholor - Zwinkels Maremka, Takken Tim, Ruyten Thys, Visser-Meily Anne, Verschuren Olaf. (2017). Body mass index and Fitness in Hjgh-Functioning Cildren and adolescents with Cerebral Palsy; What Happened over a decade? Research in Developmental Disabilities. 71:70-76.
Publisher | Google Scholor - Takken Tim, Bongers Bart C, Van Brussel Marco, Haapala Eero A, Hulzebos Erik H.J. (2017). Cardiopulmonary Exercice Testing in Pediatrics. An Amer Thor Society. 14(1):123-128.
Publisher | Google Scholor