Research Article
Evaluation Of Medication Reconciliation Process Among Home Medication, Hospital Admission, Transition Across Different Wards, And Discharge in Mizan Tepi University Teaching Hospital South West Ethiopia-A Prospective Cross-Sectional Study
- Mekuriaw Dereje *
Department of Pharmacy, College of Medicine and Health Science, Mizan-Tepi University, Mizan-Aman, Ethiopia.
*Corresponding Author: Mekuriaw Dereje, Department of Pharmacy, College of Medicine and Health Science, Mizan-Tepi University, Mizan-Aman, Ethiopia.
Citation: Dereje M. (2024). Evaluation Of Medication Reconciliation Process Among Home Medication, Hospital Admission, Transition Across Different Wards, And Discharge in Mizan Tepi University Teaching Hospital South West Ethiopia: A Prospective Cross-Sectional Study. Journal of BioMed Research and Reports, BioRes Scientia Publishers. 4(3):1-11. DOI: 10.59657/2837-4681.brs.24.063
Copyright: © 2024 Mekuriaw Dereje, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 27, 2023 | Accepted: January 23, 2024 | Published: February 05, 2024
Abstract
Background: Medication errors are common to occur most frequently during the prescribing and administering transition of care, contribute to adverse drug events in part through medication discrepancies, and this is due to the absence or under-implementation of medication reconciliation, furthermore, Current evidence conducted across the world is limited only to evaluate medication reconciliation and to classify medication discrepancies at admission, discharge and home medication, missing discrepancies during admission to different ward of the hospital
Objective: This study aimed to evaluate of medication reconciliation process among home medication, hospital admission, transition across different wards, and discharge in Mizan Tepi university teaching hospital South West Ethiopia from July 03 to September 02, 2022.
Methods and Materials: A prospective cross-sectional study was conducted at the medical ward of Mizan Tepi university teaching hospital. from July 03 to September 02, 2022. A total of 59 patients and medical records were included in the study. The data were collected using structured data collection tools developed from different literature and guidelines. The collected data were coded, entered, and analyzed using a Statistical Package for Social Sciences (SPSS, version 23).
Result: Out of 59 study participants, medication discrepancies were detected in 56 of the study group, and from 893 medication patients taking 518 medication discrepancies were identified and 96,149 and 1 unintentional medication discrepancies were identified at transition A, B, and C respectively.
Conclusion: The medication reconciliation process should be implemented in terms of a multidisciplinary approach and also MR process should be incorporated in the hospital as one part of the standard treatment guideline in order to overcome good patient recovery outcomes, and patients should be aware of some home PO medication that should they continue while they are admitted.
Keywords: transition of care; medication reconciliation; medication discrepancies; Ethiopia
Introduction: Background
Medication Errors are common as medications are procured, prescribed, dispensed, administered, and monitored but, they occur most frequently during the prescribing and administering actions [1,2,3) at transition of care, such as hospital admission and discharge, contribute to ADEs in part through medication discrepancies [2,3], that is, unexplained differences in documented medication regimens across different sites of care [2,3,4]. Medication discrepancies are common, occurring in up to 70% of patients at hospital admission or discharge, with almost one-third of these having the potential to cause patient harm (i.e., potential ADEs [PADEs] [2]. ADEs associated with medication discrepancies can be classified by drug class and type of error: omission of pre-admission prescription medication, incorrect addition of medication not part of the patient’s-admission regimen (commission), different dose, different route, and different frequency or different medication (within the same drug class). Each medication error was rated for its potential to cause harm during hospitalization if the error had not been identified and corrected [1,2,3,4,5,6,7,8]. The main problem leading to Medication discrepancies is the absence or under-implementation of medication reconciliation [5]. Medication reconciliation is the “process of identifying the most accurate list of all medications a patient is taking and using this list to provide correct medications for patients anywhere within the health care system [1].
Current evidence conducted across the world is limited only to evaluate medication reconciliation and to classify medication discrepancies at admission, discharge, and home medication, missing discrepancies during admission to different wards of the hospital and there is limited literature conducted specifically to evaluate medication reconciliation and to classify medication discrepancies in Africa including our country Ethiopia, there is no recommendation published by the Ministry of Health on the importance of an adequate collection of the medication history and MR, as well as a standardized procedure for the implementation and evaluation of this process, has not yet been suggested and there are no studies conducted in a local care setting, MTUTH and this study was conducted to fill the gap of inter-hospital discrepancies as global level and to evaluate medication reconciliation and to classify medication discrepancies in MTUTH, Ethiopia. Although traditional medicine plays an important role in Ethiopian society, knowledge about the extent and characteristics of traditional healing practices and practitioners is limited and has frequently been ignored in the national health system [8]
Methods
Study design and setting
A hospital-based prospective cross-sectional study from July 03 to September 02, 2022, at MTUTH a Teaching Hospital in Mizan Aman town, in Bench Sheko zone, South West region of Ethiopia. It is located 581 km away from Addis Ababa the capital and it is established in 1986 E.C. Adult patients coming to MTUTH have three fates that are a patient admitted to ED can weather transit to the medical ward or admitted to ICU then transit to the medical ward or patient can directly be admitted to the medical ward if treated as an inpatient.
Eligibility criteria
Inclusion Criteria
All chronic patients who were admitted to the medical ward during the study period who were previously diagnosed with any chronic disease and had a minimum of one regular home medication before admission (diagnosis was confirmed from patients’ medical record) having an intended length of stay of more than 24 h and age > 18 and above.
Exclusion Criteria
- Patients were excluded from the study if they
- Did not take any chronic medicine before hospital admission,
- Were discharged or transferred to another ward/hospital after admission
- Died during hospitalization.
- Was discontinued his or her admission by themself.
- Was isolated due to infectious diseases or compromised immunity.
- Cognitively disabled with no caregiver,
- Were discharged without prescription medication, or discharged with verbal prescription.
- Sample Size and Sampling Technique
Sampling technique
A convincing (sampling technique based on the availability of study participants at the time of data collection) sampling technique was used. Because home medication and related information is collected from the patient itself this sampling technique is best to conduct this study.
Data Collection Tools and Procedures
Two sets of data collection tools: the medical data extraction format and a structured questionnaire were used to collect data by chart review and patient/caregiver interview respectively. medical data extraction format was prepared in the English language, extracted from previous studies and WHO guidelines [ 5,8,9,10,11,12,13] and it was aimed to answer admission diagnosis, documented intentional medication discrepancies, comorbidity, and discharge diagnosis. The questionnaire was prepared in English and extracted from previous studies and WHO guidelines [3, 5,8,9,10,11,12,13], which was used to collect data through the patient interview, and it was aimed to answer patients’ sociodemographic data, home medication, medication patient taking at the transition of care and discharge medication, which was to collect data through patient interview. The data collection was implemented by the researcher in collaboration with the pharmacist in the medical ward.
Data Quality Control
A standardized data abstraction format was prepared in the English language based on previous literature reviews, related studies, and other standard protocols. The abstraction format was pre-tested before commencing the actual data collection and then the necessary adjustment was performed. Before data entry and analysis, data were cleared, categorized, compiled, coded, and verified to ensure completeness and accuracy.
Operational definition and definition of terms
- Medication reconciliation is the “process of identifying the most accurate list of all medications a patient is taking [1-13]
- Medication discrepancies are defined as unexplained changes to patients’ medication among regimens across different care sites [1-13]
- Omission; canceling of a pre-admission prescription medication [9,10,11,12,13].
- Commission; medication without clear indication.
- different dose; dose varying from pre-admission prescription medication dose [9,10,11,12,13].
- different route; route varying from pre-admission prescription medication route [9,10,11,12,13]
- different frequency; frequency varying from pre-admission prescription medication frequency [9,10,11,12,13].
- different medication; medication varying from pre-admission prescription medication (even within the same drug class) [9,10,11,12,13].
Results
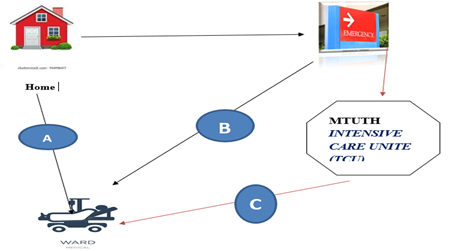
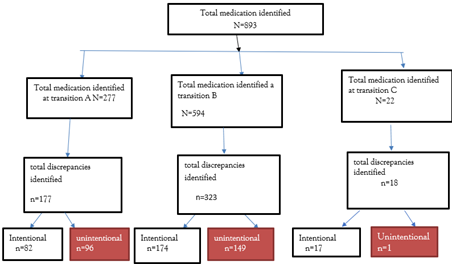
This stud encompasses three transitions as shown in Figure 1 below, the first transition is for thus patient transiting from home to the direct medical ward, the second transition is for the patient transiting from home to the emergency department and then to the medical ward whereas the third transition was for patient transiting from home to emergency department then to ICU and at the end to medical ward.
Figure 1: Medication Discrpacies Across Multiple Transition of Cares
A stand for a transition from home to a direct medical ward.
B stands for transition from home to emergency department then to medical ward.
C stands for a transition from home to the emergency department then to ICU and at the end to the medical ward.
Illustrative examples to clarify categories of medication discrepancies
Omission: Asthmatic patient taking inhaled beclomethasone before admission, Missing preadmission beclomethasone intentionally or unintentionally during admission.
Commission: patient is without any sign of infection or has no diagnosis with any of infectious disease but taking ceftriaxone intentionally or unintentionally.
Different dose: hypertensive patient taking enalapril 5mg before admission, now taking 10mg of the same drug during admission or discharge intentionally or unintentionally.
Different route: a patient taking frusemide po at home now taking IV during admission intentionally or unintentionally.
Different frequency: a patient taking frusemide OD at home now taking BID during admission or discharge intentionally or unintentionally.
Different medication: Asthmatic patient taking inhaled beclomethasone before admission, changing preadmission inhaled beclomethasone to IV hydrocortisone at admission intentionally or unintentionally.
Description of the included population and study medication sample
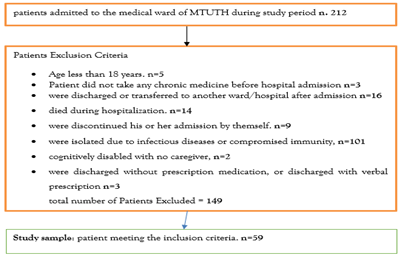
During the study period, 212 patients were admitted to the medical ward of MTUTH. Among those patients, 59 subjects met the inclusion criteria and were enrolled in the study (Fig. 2).
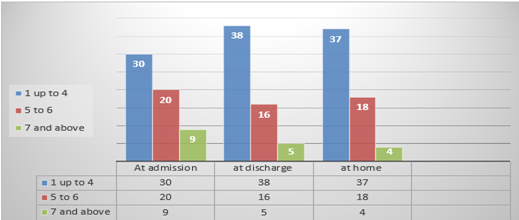
28.8 % of the patient age falls under the age categories of 60-64, 61% were male, 45.8% of the patient were delivered to the hospital with the help of another while being conscious and 62.7% transit from home to the emergency department then to the medical ward and more than half of the study participant stays in the hospital less than a week with mean and Std. Deviation of 18.08 days and 26.385 days respectively. Around 47.5 % of the study group have one comorbidity whereas 27.1 % of the patient discharge diagnosis was grouped under endocrine and metabolic diseases followed by circulatory and respiratory system 25.4 % and 18.6 % respectively (Table 1) and as shown in figure 3 more than half of the patient takes four and less medication at admission, discharge, and home medication.
Figure 2: Flow chart of the inclusion and exclusion criteria of study patients
Table 1: Characteristics of the study samples (n = 59)
| Variables | Frequency | Percent | |
| Age | 18-24 | 7 | 11.9 |
| 25-34 | 3 | 5.1 | |
| 35-44 | 10 | 16.9 | |
| 45-54 | 9 | 15.3 | |
| 55-59 | 10 | 16.9 | |
| 60-64 | 17 | 28.8 | |
| >65 | 3 | 5.1 | |
| Total | 59 | 100.0 | |
| Sex | Female | 23 | 39.0 |
| Male | 36 | 61.0 | |
| Total | 59 | 100.0 | |
| route of hospital delivery | By oneself | 8 | 13.6 |
| With the help of another while being conscious | 27 | 45.8 | |
| With the help of another while being unconscious | 14 | 23.7 | |
| By ambulance or any automobile as emergency | 10 | 16.9 | |
| Total | 59 | 100.0 | |
| transition of patient | home to direct medical ward | 21 | 35.6 |
| home to the emergency department then to the medical ward | 37 | 62.7 | |
| home to the emergency department then to ICU and then to the medical ward | 1 | 1.7 | |
| Total | 50 | 100.0 | |
Figure 3: Number of medications at admission, discharge, and home.
Medication discrepancies
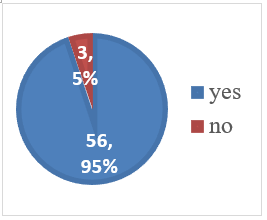
Prevalence of Medication discrepancies: Among 59 study groups, Medication discrepancies were identified in 56(94.9%) of the study participants. Figure 5 summarizes the prevalence of medication discrepancies.
Figure 4: Prevalence of Medication discrepancies
Overview of total medication and categorizing medication discrepancies
A total of 893 Medication was taken among 59 study participants of these 518 medication discrepancies were identified over the three transitions, 177, 323,18 respectively. From this 96, 149 and 1 discrepancies were unintentional discrepancies over the respective transitions (Figure 4).
Figure 5: Flow chart describing the overview of total medication and categorizing medication discrepancies.
Medication discrepancies at transition 5A
Among 59 study group 21(36.6%) were transited from home to direct medical ward (Table 2) and the total number of homes, admission and discharge were 82 ,103 and 89 respectively and minimum medication patient taking in this transition were 2 were as maximum was 7. Among all 274 Medication patient taking 177 discrepancies were identified in this transition, of this 93 discrepancies were identified at the time of hospital admission and 85 discrepancies were identified at hospital discharge(Figure 5), ‘medication Omission’ and ‘different dose’ was the most frequent type Intentional discrepancy identified at admission and discharge respectively whereas ‘medication Omission’ was the was the most frequent type unintentional discrepancy identified at both admission and discharge.
Medication discrepancies identified between home and admission medication(5A1)
93 discrepancies were identified at the time of hospital admission to medical ward, and of these, 46(49.46%) of the discrepancies were Intentional and the remaining 47(50.54 %) were unintentional discrepancies. From 46(49.46%) Intentional discrepancies identified ‘medication Omission’ was the most frequent intentional discrepancy identified which account around (12,26%) followed by ‘different routes’ and ‘different medications’ (10,21.7%) and (8,8.73%) respectively. Of thus unintentional discrepancies [(47,50.54%)], ‘medication Omission’ was the most frequent discrepancy identified which account around (17,36.17%) followed by ‘different dose’ and ‘different routes’ (9,19.15%) and (8,17%) (Table 2).
Table 3: classification of discrepancies across transition of 5A1
| Classification of discrepancies | Reason | Total | |
| Intentional (fre, %) | unintentional (fre, %) | ||
| Omission | (12,26) | (17,36.17) | 29 |
| Commission | (4,15.23) | (6,12.77) | 10 |
| different medications | (8,8.73) | 0 | 8 |
| different routes | (10,21.7) | (8,17) | 18 |
| different frequency | (6,13.45) | (7,14.9) | 13 |
| different dose | (6,13.45) | (9,19.15) | 15 |
| Total discrepancies across transition of 5A1 | (46,49.46) | (47,50.54) | 93(100) |
Medication discrepancies identified between home and discharge medication (5A2)
85 discrepancies were identified at the time of hospital discharge of these, of the discrepancies 36(42.35%) were Intentional and the remaining 49(56.65 %) were unintentional discrepancies. From 36(42.35%) Intentional discrepancies identified ‘different dose’ was the most frequent intentional discrepancy identified which account around (15,41.66%) followed by ‘medications Omission’ and ‘different medications’ (9,25%) and (6,16.66%) respectively. Of thus unintentional discrepancies [(48,56.65%)], ‘medication Omission’ was the most frequent discrepancy identified which account around (17, 34.69%) followed by ‘different dose’ and ‘different frequency’ (13,26.53%) and (11,22.45%) (Table 3).
Table 4: classification of discrepancies across transition of 5A2
| Classification of discrepancies | Reason | Total | |
| Intentional(fre,%) | unintentional(fre,%) | ||
| Omission | (9,25) | (17,34.69) | 26 |
| Commission | (4,11.1) | 0 | 4 |
| different medications | (6,16.66) | (4,8.17) | 10 |
| different routes | 0 | (4,8.17) | 4 |
| different frequency | (2,5.55) | (11,22.45) | 13 |
| different dose | (15,41.66) | (13,26.53) | 28 |
| Total discrepancies across transition of 5A2 | (36,42.35) | (49,56.65) | 85(100) |
Medication discrepancies at transition 5B
Among 59 study group 37(62.7%) were transited from home to emergency department then to medical ward and the total number of homes, admission at ED, admission at medical ward and discharge were 139,150,166 and 139 respectively. Minimum and maximum medication patient taking in all transition were 1 and 8 respectively. Among all 594 Medication patient taking 323 discrepancies were identified in this transition, of these 94 discrepancies were identified at the time of hospital admission to ED ,121 discrepancies were identified at the time of hospital admission to medical ward and 108 discrepancies were identified at hospital discharge.
Medication discrepancies identified between home and admission at ED
94 discrepancies were identified at the time of hospital admission to ED and of these, 51(54.26%) of the discrepancies were Intentional and the remaining 43(45.74 %) were unintentional discrepancies. From 51(54.26%) Intentional discrepancies identified ‘different routes’ was the most frequent intentional discrepancy identified which account around 14(27.45%) followed by ‘different dose’ and ‘medications Omission’ ((12,23.53%) and (11,21.57%) respectively. Of thus unintentional discrepancies [(43(45.74 %)], ‘medication Omission’ was the most frequent discrepancy identified which account around (19,44.19%) followed by ‘different routes’ and ‘different dose’ (8,18.6%) and (7,16.28%) (Table 4).
Table 5: Classification of discrepancies across transition of 5B1
| Classification of discrepancies | Reason | Total | |
| Intentional(fre,%) | unintentional(fre,%) | ||
| Omission | (11,21.57) | (19,44.19) | 30 |
| Commission | (4,7.84) | (3,6.8) | 7 |
| different medications | (6,11.75) | (2,4.65) | 8 |
| different routes | 14(27.45) | (8,18.6) | 22 |
| different frequency | (4,7.84) | (4,9.3) | 8 |
| different dose | (12,23.53) | (7,16.28) | 19 |
| Total discrepancies across transition of 5B1 | (51,54.26) | (43,45.74) | 94(100) |
Medication discrepancies identified between home and admission at medical ward 121 discrepancies were identified at the time of hospital admission to medical ward and, of these, 52(42.98%) of the discrepancies were Intentional and the remaining 69(57.02%) were unintentional discrepancies. From 52(42.98%) Intentional discrepancies identified ‘different routes’ was the most frequent intentional discrepancy identified which account around (13,25%) followed by ‘medications Commission’ and medications Omission (11,21.15%) and (10,19.23%) respectively. Of thus unintentional discrepancies (69,57.02%), ‘medication Omission’ was the most frequent discrepancy identified which account around (33,47.83%) followed by ‘different dose’ and ‘different frequency’ (15,21.74%) and (12,17.4%) respectively (table 5).
Table 6: classification of discrepancies across transition of 5B2
| Classification of discrepancies | Reason | Total | |
| Intentional(fre,%) | unintentional(fre,%) | ||
| Omission | (10,19.23) | (33,47.83) | 43 |
| Commission | (11,21.15) | (1,1.45) | 12 |
| different medications | (7,13.46) | (2,2.9) | 9 |
| different routes | (13,25) | (6,8.7) | 19 |
| different frequency | (6,11.4) | (12,17.4) | 18 |
| different dose | (5,9.62) | (15,21.74) | 20 |
| Total discrepancies across transition of 5B2 | (52,42.98) | (69,57.02) | 121(100) |
Medication discrepancies identified between home and discharge medication
108 discrepancies were identified at the time of hospital discharge of these, 71(65.74%) were Intentional and the remaining 37(34.26%) were unintentional discrepancies. From 71(65.74%) Intentional discrepancies identified ‘different routes’ was the most frequent intentional discrepancy identified which account around (21,29.58 %) followed by ‘different dose’ and ‘medication Omission’ (19,26.76%) and (12,16.9 %) respectively. Of thus unintentional discrepancies [(37(34.26%)] , ‘medication Omission’ was the most frequent discrepancy identified which account around (21,56.76 % ) followed by ‘different frequency’ and different dose (7,19.92%) and (6,16.22%) ( Table 6 ).
Table 7: classification of discrepancies across transition of 5B3
| Classification of discrepancies | Reason | Total | |
| Intentional (fre, %) | Unintentionall (fre, %) | ||
| Omission | (12,16.9) | (21,56.76) | 33 |
| Commission | (8,11.27) | (0,0) | 8 |
| different medications | (7,9.86) | (1,2.7) | 8 |
| different routes | (21,29.58) | (2,5.4) | 23 |
| different frequency | (4,6.63) | (7,19.92) | 11 |
| different dose | (19,26.76) | (6,16.22) | 25 |
| Total discrepancies across transition of 5B3 | (71,65.74) | (37,34.26) | 108(100) |
Medication discrepancies at transition 5C
Among 59 study group 1(1.7%) were transited from home to emergency department then to ICU and then to medical ward and the total number of homes, admission at ED, ICU admission at medical ward and discharge were 2 ,7 ,5,3 and 2 respectively. Among all 22 Medication patient across respective transition 18 discrepancies were identified. 9 discrepancies were identified during admission to ED and all was intentional, where us 4 of the discrepancies were identified during admission to ICU and MW all of the discrepancies were intentional and 5 of the discrepancies were identified during discharge, of thus 4 of the discrepancies were intentional and one unintentional ‘Medication Omission’ were identified (table 7).
Table 8: classification of discrepancies across transition of 5C
| Classification of medication discrepancies | Medication discrepancies at transition 5C1(home and ED) | Medication discrepancies at transition 5C2(ED and ICU) | Medication discrepancies at transition 5C3(ICU and MW) | Medication discrepancies at transition 5C4(MW and discharge) | ||||
| Intentional (fre, %) | Unintentional (fre,%) | Intentional (fre,%) | Unintentional (fre,%) | Intentional (fre,%) | Unintentional (fre,%) | Intentional(fre,%) | Unintentional (fre,%) | |
| Omission | (1,11.1) | 0 | -2,100 | 0 | (1,50) | 0 | (2,50) | -1,100 |
| Commission | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Different medications | (7,77.8) | 0 | 0 | 0 | 0 | 0 | (1,25) | 0 |
| different routes | (1,11) | 0 | 0 | 0 | 0 | 0 | (1,25) | 0 |
| different frequency | (1,11) | 0 | 0 | 0 | (1,50) | 0 | 0 | 0 |
| Different dose | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | -9,100 | 0 | 2 | 0 | -2,100 | 0 | -4,100 | -1,100 |
Discussion
Assessing and classifying medication discrepancies is always recommended as a cornerstone for the implementation of MR best practices and it has an incalculable role for measuring the impact of MR interventions on patient safety [8]. The current study was conducted in one of the Ethiopian hospitals MTUTH which is located in the Bench Sheko zone. The study was classified into three main classes as the main nature of the hospital mainly transit patients in the hospital. The first probability of the patient being admitted is direct to the medical ward, the second option is admitted to the hospital as an emergency then transferred to the medical ward or ICU, and at the end to the medical ward as option three. The reconciliation process of home medications was evaluated at hospital admission, inter-hospital transition, and discharge to identify all medication discrepancies and to classify them according to the kind of change registered and the intentionality.
In the first transition, 274 Medication patient taking were identified and,177(64.6%) discrepancies were identified in this transition, of these 93 (33.94%) discrepancies were identified at the time of hospital admission of this 47(17.15 %) of the discrepancies were unintentional and 85(31.02%) discrepancies were identified at hospital discharge of this 48(17.52%) of the discrepancies were unintentional. The available literature showed almost similar percentages of unintentional discrepancies for hospital admission, ranging from 6.2 to 26.6% at admission (1,2,3,4), and the current studies showed slightly higher percentages of unintentional discrepancies for hospital discharge ranging from 7.5% to 9.67 % at discharge (1,2,3,4).
In the second transition, 594 Medication patient taking were identified and,323(54.37%) discrepancies were identified in this transition, of these 215(36.2) [94(15.82%) were identified at the time of hospital admission to ED and 121(20.37%) discrepancies were identified at the time of hospital admission to medical ward)], of this 112(18.86%) [43(7.24%) were unintentional discrepancies at ED and 69(11.62% t were identified at the time of hospital admission to medical ward) were unintentional discrepancies]. 108(18.18%) discrepancies were identified at the time of hospital discharge of these 37(6.23%) were unintentional discrepancies. The available literature showed almost similar percentages of unintentional discrepancies for hospital admission, ranging from 6.2 to 26.6% at admission (1,2,3,4) and the current studies showed higher percentages of unintentional discrepancies for hospital discharge ranging from 7.5% to 9.67 % at discharge [1,2,3,4]. These differences may be explained by different study settings and different selections that each study group made in the medications considered for the analyses due to an increase in inter-hospital transition. In agreement with the available literature (1,2,3,4) the prevalence of unintentional discrepancies at hospital discharge was greater than that of hospital admission. The early detection and correction of discrepancies at admission can reduce the likelihood of these errors being repeated at inter-hospital admission and patient discharge. Therefore, discrepancies in patients’ hospital admission should be a priority in MR programs to increase patient safety strategies and avoid possible ADEs due to unintentional medication changes.
Regarding the type of discrepancy, medication omission was the frequent type of discrepancy identified during the first transition, at a rate of 26% and 36.17 % at admission and at discharge, respectively. And in the second transition also medication omission” was the frequent type of discrepancy identified during the first transition, at a rate of 44.19%, 47.83 %, and 56.76% at admission to ED, and MW at discharge, respectively. Which is a similar finding to the available literature.
According to this study, 27.1% of the patient discrepancies are on endocrine and metabolic-related discharge diagnosis which is followed by circulatory system-related diseases which account for around 25.1 % unlike available literature the respiratory system-R (19.5%) [8], and thus difference may be due to difference in the study setting and study periods.
This study has some limitations. The study period was too short, despite the sample of admitted patients being larger, small meet inclusion criteria, in addition, the analysis does not distinguish undocumented intentional medication changes that were classified as unintentional discrepancies and also medication is counted as individual list what if the patient transit from different ward with the same drugs.
Conclusion
In conclusion, this finding showed that transitions of care are key moments for patient safety in terms of unintentional medication discrepancies and that a more structured MR process is needed to avoid errors and related ADEs. Both at admission and at discharge, almost half of the patients had at least one unintentional medication discrepancy, and these were more likely to occur in patients with a higher number of prescriptions, with longer hospitalization times, and in patients’ transit across multiple settings of the hospital. The MR process should be implemented in terms of a multidisciplinary approach and also MR process should be incorporated in the hospital as one part of the standard treatment guideline in order to overcome good patient recovery outcomes, and Patients should be aware of some home PO medication that should they continue while they are admitted and patients/caregivers should be involved and informed of every medication change and followed to ensure correct medication knowledge and management during and after hospitalization.
Abbreviations
ADEs: Adverse Drug Events
PADEs: Potential Adverse Drug Events
BPMH: Best Possible Medication History
MTUTH: Mizan Tepi University Teaching Hospital
ED: Emergency Department
MW-Medical Ward
MR: Medication Reconciliation
SMR: Shared Medication Record
PRN: As Needed
PO: Per Mouth
OD: Once Per Day
BID: Twice Per Day
Acknowledgement
We would like to acknowledge MTUTH pharmacists for their cooperation and support during the data collection period Patients and/or patient caregivers included in this study are also appreciated for their valuable cooperation and patience during data collection interviews.
Funding
This work was not funded by anyone.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the institutional review board of Mizan Tepi University, college of Medicine and Health. Letter of permission was presented to the managements of MTUTH who allowed us to use patients’ medical records. Informed consent was obtained from all subjects and/or their legal guardian(s) and the aim and purpose of the study is clearly seated before data collection started. Patients’ information such as name and address of the patients was not recorded during data collection to maintain confidentiality of the patients. This study did not involve human experiments or human tissue and this is explained to all subjects. All findings in this paper were performed in accordance with relevant guidelines and regulations (such as the Declaration of Helsinki).
Consent for publication
Not applicable to this work.
Competing interests
The author declared no potential competing of interest concerning the research, authorship, and/or publication of this article.
Data availability
All the datasets used/or analyzed during the current study are available from the corresponding author upon reasonable request.
Conflict of interest
I declare that no conflict of interest
Authors’ Contributions
M.D is solely responsible for all work submitted whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
References
- Mueller SK, Sponsler KC, Kripalani S, Schnipper J. (2012). Hospitalbased medication reconciliation practices: a systematic review. Arch Intern Med., 172:1057-1069
Publisher | Google Scholor - Gleason KM, McDaniel MR, Feinglass J, Baker DW, Lindquist L, Liss D, et al. (20210). Results of the medications at transitions and clinical handofs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 25:441-447.
Publisher | Google Scholor - und JK, Sletvold O, Mellingsæter TC, Hukari R, Hole T, Uggen PE, et al. (2017). Discrepancies in drug histories at admission to gastrointestinal surgery, internal medicine and geriatric hospital wards in Central Norway: a cross-sectional study. BMJ Open, 7:e013427.
Publisher | Google Scholor - Coleman EA, Smith JD, Raha D, Min S. (2005). Posthospital medication discrepancies: prevalence and contributing factors. Arch Intern Med., 165:1842.
Publisher | Google Scholor - World Health Organization. (2014). Action on patient safety (WHO High 5 s) medication reconciliation implementation guide: Assuming medication accuracy at transitions in care: medication reconciliation 2014.
Publisher | Google Scholor - Cristina C, Teresa Dalla Z. (2018). Evaluation of the medication reconciliation process and classification of discrepancies at hospital admission and discharge in Italy. International Journal of Clinical Pharmacy.
Publisher | Google Scholor - Kwan JL, Lo L, Sampson M, Shojania KG. (2013). Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med., 158:397
Publisher | Google Scholor - Dei Tos M, Canova C, Dalla Zuanna T. (2020). Evaluation of the medication reconciliation process and classification of discrepancies at hospital admission and discharge in Italy. Int J Clin Pharm, 42(4)
Publisher | Google Scholor - Joint Commission, Quick Safety Issue 26: Transitions of care: managing medications 2016.
Publisher | Google Scholor - Abu Farha R, Yousef A, Gharaibeh L, Alkhalaileh W, Mukattash T, Alefishat E. (2021). Medication discrepancies among hospitalized patients with hypertension: assessment of prevalence and risk factors. BMC Health Serv Res., 14:21(1):1338
Publisher | Google Scholor - Andersen, T.S.; Gemmer, M.N.; Sejberg, H.R.C.; Jørgensen, L.M.; Kallemose, T.; et al. (2022). Medicines Reconciliation in the Emergency Department: Important Prescribing Discrepancies between the Shared Medication Record and Patients’ Actual Use of Medication. Pharmaceuticals, 15:142.
Publisher | Google Scholor - Alanazi AS, Awwad S, Khan TM, Asdaq SMB, Mohzari Y, et al. (2022). Medication reconciliation on discharge in a tertiary care Riyadh Hospital: An observational study. PLoS One, 17(3):e0265042.
Publisher | Google Scholor - JOUR, Khansa, Sara, Mukhtar, Amnah, Abduljawad, Merryland, Aseeri, Mohammed; (2016). Impact of Medication Reconciliation upon Discharge on Reducing Medication Errors. Journal of Pharmacovigilance.
Publisher | Google Scholor