Research Article
Estimation of the Economic Burden For COVID-19 Case Management in Addis Ababa, Ethiopia
- Senait Alemayehu Bashah *
Health System and Reproductive Health Research Directorate, Ethiopian Public Health Institute, Ethiopia.
*Corresponding Author: Senait Alemayehu Bashah, Health System and Reproductive Health Research Directorate, Ethiopian Public Health Institute, Ethiopia.
Citation: Senait A. Bashah, Yohannis D, Zeru A, Tadele W, Getachew T. (2024). Estimation of the Economic Burden For COVID-19 Case Management in Addis Ababa, Ethiopia. Scientific Research and Reports, BioRes Scientia Publishers. 1(1):1-10. DOI: 10.59657/2996-8550.brs.24.005
Copyright: © 2024 Senait Alemayehu Bashah, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 30, 2024 | Accepted: February 15, 2024 | Published: February 26, 2024
Abstract
Introduction: The COVID-19 pandemic has increased patient and health-care system demands, resulting in major resource constraints (hospital beds, workforce, intensive care beds, ventilators etc.). Case management for symptomatic COVID-19 patients is an important health-care intervention. Patients infected with COVID-19 were managed based on their severity, using Ethiopian recommendations for critical ARDS care, which included noninvasive measures if intubation and invasive mechanical ventilation failed, as well as additional interventions. This study evaluated the economic burden of COVID-19 case management to assist policymakers with recommendations on how to best use existing resources and panning during COVID-19 case management.
Methods: The study was done ingredients, based top-down micro-costing approach with the partial economic evaluation through a costing study design was applied which elaborates the identification, measurement, and valuation of resources used for COVID -19 case management at the treatment centers and home-based isolation care for the patient (direct and indirect) and health system (variable and capital) cost. We used the human capital approach to estimate the indirect cost. The cost was reported in 2021 United States Dollar (US$) and we used a 3% discount rate. We assessed numerous sources of cost data estimation of unit cost per day per patient and per episode for the mild/ moderate, severe, and critical cases of COVID-19 management.
Result: In a hospital setting, the average societal costs for mild/moderate, severe, noninvasive, and invasive critical management per episode are $951, $3,449, $5,514, and $6,500, respectively, and the indirect (productivity loss) cost due to job absenteeism and premature death were estimated $15, $30 and $56 cost per day per person for home-based isolation, severe and critical patient respectively, from the health system cost 64 % of recourses utilized for the supply (oxygen, personal protection equipment, and drugs) consummation.
Conclusion:These results indicated that the critical case of the disease extremely carries a high cost in this event. It is projected that the high prevalence rate of COVID-19 has been imposing a heavy economic burden on the health system and patients and even in the country.
Keywords: COVID-19; economic burden; cost; mild/moderate; severe; critical
Introduction
The COVID-19 outbreak first emerged in Wuhan, Hubei province, and quickly spread, with initial cases detected in January in countries including Japan, Korea, the United States, France, Germany, and the United Kingdom. From December 2019 to December 2020, the pandemic impacted 235 countries/territories, resulting in 78,422,954 cases and 1,741,204 deaths globally (Case Fatality Rate = 2.22%). The United States of America (USA) recorded the highest number of cases [1]. In Africa, 57 countries/territories have confirmed COVID-19 cases. By December 2020, the continent had reported a total of 2,649,440 cases and 61,971 deaths (CFR=2.34%). South Africa had the highest number of cases (1,473,700) with a CFR of 2.68%, followed by Morocco with 474,966 cases and a CFR of 1.67%. Ethiopia, ranking third after South Africa and Morocco in total cases, reported the highest number of COVID-19 cases in East Africa. Ethiopia recorded its first COVID-19 case on 13 March 2020, just two days before the WHO declared the pandemic. According to the COVID-19 daily situation report in Ethiopia until 01 April 2021, the country had tested 2,365,187 individuals, of whom 208,961 cases (9%) tested positive. Among the confirmed cases, 2,890 individuals (CFR=1.4%) had died, while 159,436 (31.1%) had recovered. The majority of cases (over 90%) were managed in Addis Ababa [2]. (18,468,139 cases) with a Case Fatality Rate (CFR) of 1.77%, followed by India (10,187,850 cases) with a CFR of 1.45% [3].
The classification of COVID-19 severity is based on the following definitions:1) Critical COVID-19 is described as being critical for conditions such as acute respiratory distress syndrome (ARDS), sepsis, septic shock, or other circumstances that typically necessitate life-sustaining interventions like mechanical ventilation.2) Severe COVID-19 is classified as having an oxygen saturation level below 90% while on room air, coupled with indicators of severe respiratory distress.3) Non-severe COVID-19 refers to cases without critical or severe symptoms and includes Asymptomatic, mild, and moderate presentations.[4,5]. The global spread of the coronavirus (COVID-19) is posing unforeseen challenges to healthcare infrastructures worldwide. Among these challenges is a scarcity of essential supplies like diagnostic tests, ventilators, and personal protective equipment (PPE) [1]. Research indicates a correlation between healthcare resource availability and COVID-19 mortality rates [6]. Furthermore, patients with severe COVID-19 often necessitate expensive treatments such as mechanical ventilation and extracorporeal membrane oxygenation, potentially leading to a significant rise in healthcare expenses. In Africa, only a limited number of countries are engaged in estimating the costs of COVID-19 treatment, and the results have shown considerable variation [7]. For instance, a study in Kenya in 2020 estimated the unit cost per day for COVID-19 treatment at home-based isolation care, mild to moderate, severe, and critical cases to be USD 18.89, USD 63.68, USD 124.53, and USD 599.51, respectively. This study highlighted the economic burden faced by patients and the healthcare system during COVID-19 treatment [8]. In Iran, another study found that the average medical cost for treating a critical COVID-19 patient was estimated at USD 3755, illustrating the significant economic strain posed by high rates of COVID-19 cases on the country's healthcare system [9].
Ethiopia, being a low-income country with a Gross Domestic Product (GDP) per capita of US$953 in 2019 [10]. and a per capita health expenditure of about US$33 in 2016/17 [19].The pandemic places a substantial strain on the country's economy, impacting economic growth, and leading to increased costs related to illness management, inpatient and outpatient care, healthcare system resources, and productivity loss [11].Regarding the Economic Burden of COVID 19 in Ethiopia, the number of specialist health workforce in Ethiopia, they are 0.54 per 1000,000 people hospital beds: 0.3 per 1,000 people [12]. In the context of the economic burden of COVID-19 in Ethiopia, the availability of specialist health workers is limited, with only 0.54 per 100,000 people, and hospital beds are scarce at 0.3 per 1,000 people. The median number of skilled health workers in emerging regions is reported to be below 8 per 15,000 inhabitants. Additionally, 68% of children lack access to basic healthcare services [14].Despite the dedication of healthcare staff involved in COVID-19 management, a significant portion of facilities lack experienced clinical staff for critical procedures like invasive mechanical ventilation/intubation. The COVID-19 pandemic has induced a substantial impact on the health system, supply chain disruptions, personal incomes, and overall healthcare infrastructure. This global health crisis has resulted in economic repercussions worldwide, including in Ethiopia, causing job losses, business closures, disrupted trade, and severe setbacks to the tourism sector [15]. Consequently, the objective of this study is to assess the economic implications of COVID-19 treatment in Addis Ababa, Ethiopia. By providing recommendations and insights, this study aims to aid policymakers in making informed decisions and resource allocations for COVID-19 treatment. This research seeks to contribute valuable information to the existing literature, address the gaps in cost data, and enhance the understanding of the effectiveness of interventions in combatting the pandemic.
Methods
Study design and setting
This study was carried out in Addis Ababa, Ethiopia, the capital city of the country, covering an area of 540 square kilometers and hosting a significant COVID-19 intervention response in the nation [16]. To gather data based on the caseload, primary data was collected from Eka Kotbe Hospital, the initial COVID-19 treatment facility in Ethiopia, and from four health centers catering to cases ranging from mild to severe COVID-19. The data collection was conducted from July 1 to September 30, 2021, involving enrolled cases from January 1 to May 31, 2021. A sample of 210 COVID-19 patients aged 18 and above was randomly chosen from those receiving care at home-based isolation, health centers, and hospitals. In this economic evaluation study, a costing study design was employed. The top-down micro-costing ingredient-based methodology was utilized to calculate the average daily cost of managing patients with home-based isolation care, mild to moderate cases, severe cases, and critically ill COVID-19 patients[2]. This costing strategy involves considering overall expenditures at a central level for the allocation of costs to each intervention.
Cost data sources and collection procedure
The data collection instruments primarily consisted of a questionnaire adapted from the WHO's 2017 methodology used in tuberculosis costing investigations [17]. Cost items were categorized into variable and capital costs. Variable costs (such as personnel salaries, medications, tests, oxygen, and medical supplies like PPE) are expenses that are recurrent and lasting less than a year, while capital costs (including buildings, furniture, medical equipment, vehicles, and computers) are expected to endure beyond one year [18]. The costing was conducted from both healthcare provider and patient perspectives and comprised three steps: first, identifying all resources based on the severity of COVID-19 cases; second, measuring each cost item based on unit cost; and finally, valuing each input using suitable unit prices according to the severity of the patients[19]. To discern the types of resource inputs, we consulted the Ethiopia COVID-19 clinical management guidelines, referenced published articles, sought expert opinions, and utilized the WHO COVID-19 Essential Supplies Forecasting Tool [20]. The healthcare provider costs were estimated using an ingredients-based approach, encompassing costs of facilities, capital, personnel, and supplies such as oxygen, medical supplies (including PPE), medications, and tests based on the severity of the patient (refer to Table 1). Data were collected from hospital records and interviews with patients and experts, including ICU coordinators, laboratory technologists, pharmacists, ICU and other nurses, internists, radiologists, physicians, and administrative staff involved in the COVID-19 response, following informed consent.
Table 1: Sources of the COVID-19 case management costing data and resources in puts
| Capital cost; Any recourses that have a useful life of more than one year | ||
| Cost Items | Resources in put cost | Sources |
| Building costs | Room were ICU, HDU emergency, Donning, General wared, sterilization. Laboratory pharmacy, store etc. | Consulting local expert estimates per square km [21] |
| Medical equipment’s and furniture’s &beds | Beds & Ventilators: ICU and Ward beds, Invasive monitoring and None invasive CPAP Machine, Mechanical Venti, Defibrillator | Purchase prices list from hospital supply chain and Ethiopia Pharmaceuticals Supply Agency (EPSA) |
| Medical devices ECG machine, Glucometer, pulse oximeter, Clinical Chemistry analyzer, Defibrillator, Ultrasound with different probes, Portable and non-portable monitor | ||
| Respiratory support accessories &other’s capital: High flow machine, oxygen cylinder, Suction machine, oxygen concentrators, laryngoscope, Ambu-bags. Ambulances, Furniture’s and computers | ||
| Variable cost used with duration of less than a year | ||
| Direct non-medical Patient cost | (Food and transport) cost | Food cost [22],and |
| Indirect patient cost | Productivity loss and death due to COVID-19 | Interview patient, review card |
| Personal cost | Nurses Critical care, general and severe wared nurses, coordinator nurses, ICU coordinator etc. Physicians, residents, internists, intensivists, anesthesiologists, ICU coordinator etc. Allied health professionals: Nutritionist, psychologists, Bio medical engineers, infection prevention, Radiologist’s lab technologist, Pharmacists Supportive staff: Cleaner, ambulance drivers, oxygen handlers etc. | Interview head of facility & review payrolls; list of salary scales and risk payment |
| Drugs, Medical supply, Oxygen and investigation | ||
| Investigations/Diagnostics Drugs &complication managements Medical supp & PPE Oxygen | Chemistry, Complete blood count, Electrolytes, Blood glucose, ECG, X-ray, COVID test etc. Vaso constrictive agents (adrenalin & noradrenalin), Antibiotics/antimicrobials, corticosteroids (dexamethasone), and anticoagulation, Iv fluid (NS, RL), glucose 40%, Anlages and opioids etc. PPE (Cover all, N95 mask, Face mask, Plastic apron, None sterile and surgical glove, goggles, Apron etc.) Medical supply (CPAP mask, Urine bags, Catheters, NG tube, Nasal Cannula& IV Cannula, Suction catheters, oropharyngeal air way, endotracheal tube etc.) Moderate or low flow, None invasive ventilator & Machinal invasive Ventilator oxygen support | Patient cared& expert opinion Purchase prices list from hospital supply chain and Ethiopia Pharmaceuticals Supply Agency (EPSA) Bio medical engineers’ experts |
Cost data analyses
The cost analysis was completed on excel 2021 spreadsheet[23]. and SPSS version 25. The economic burden of COVID -19 estimate based on the patients and their household using cost of illness design[2].The gross wage is the unit of value before COVID-19 illness, income and productivity loss or the indirect cost of the patients were assessed based on the human capital approach (HCA) it was widely used to estimate the productivity loss cost [25,26]. Patient direct non-medical costs encompass expenses related to accessing COVID-19 services, including transportation, nutritional needs, healthcare visits, and accommodation costs. These costs were quantified through face-to-face interviews to determine round trips and the number of visits. Hospital patient food costs were estimated based on those for multi-drug-resistant tuberculosis (MDR TB) patients [22]. Personnel cost were estimated based staff-to-patient ratios on the opinions of government experts working at appropriate staffing levels of care for COVID-19 managements[4]. In this study, excluding overtime hours and annual leave, we assumed that staff worked an average of 2090 hours per year. The daily work hours of each staff member at a health center or hospital were multiplied by the likelihood of caring for patients and the staff-to-patient ratios for mild/moderate, severe, and critical cases to calculate the staff time per patient per day. For allied personnel without a staff-to-patient ratio, this was estimated based on the hours dedicated per case. Subsequently, the staff's daily cost per patient was estimated by multiplying the staff time per patient by the daily staff salary rate and then by the length of stay based on the severity of the cases.
Supply costs, including drugs, investigations, medical supplies, and personal protective equipment, were evaluated based on the average unit cost per patient per day and multiplied by the quantity of tests/drugs provided per day per severity. Oxygen costs were determined in consultation with patient experts, considering oxygen therapy requirements ranging from 6 to 15 liters per minute for moderate flow treatments using various masks. The average consumption per patient ranged from 40 liters (2.5 cylinders) to 6 cylinders per day, depending on the oxygen therapy method. Capital resources such as furniture, medical equipment, and ambulance costs were annuitized over their useful life-years. Furniture and medical equipment were considered to have useful lives of 5 and 10 years, respectively, while ambulances were estimated to last 10 years with a 3% discount rate on the initial unit price. Additionally, consumer price index adjustments were made to account for annual inflation rates [25].
All unit costs per patient per day were multiplied by the average duration per severity level to calculate the total unit cost per patient for COVID-19 treatment, stratified by facility and severity. The valuation process involved two costing steps: measuring the quantities of resources utilized with their respective unit prices, followed by valuing the resources in Ethiopian Birr and converting to USD at a rate of 41.5 given the prevailing exchange rate. Prices were adjusted for inflation using the consumer price index from the base year 2021, and all costs were reported in 2021 US Dollars. The average length of stay for mild/moderate and severe cases in health centers was 14 and 16 days, respectively. Additionally, this duration might be slightly longer in hospitals, with lengths of stay estimated at 18, 19, and 21 days for mild/moderate, severe, and critical cases. Ultimately, unit costs were determined based on disease severity and multiplied by the average length of stay per facility [26].
Result
Demographic Characteristics
Out of 210 study participants, most were male (65.2%) and 73 (34.8%) were female as shown in Error! Reference source not found. analyzing the age distribution of the respondents, it was found that 66 (31.4%) participants were aged 18 to 35, 96 (45.7%) were in the 36 to 55 age group, and 56 (22.8%) were 56 years old or older. In terms of marital status, 123 (58.6%) participants were married, 40 (19%) were single, and the remaining 21 (10.1%) were divorced or widowed. Regarding educational achievements, 17 (8.1%) respondents had post-graduate qualifications, 18 (8.6%) held bachelor's degrees, and 60 (28.6%) had completed a diploma. Additionally, 11 (5.2%) had not attended school, while 40 (19%) had basic literacy skills. Looking at the occupational status of participants, 75 (35.7%) were retired, 29 (13.8%) were government employees, 27 (12.9%) were self-employed, and 47 (22.4%) were day laborers.
Table 2: Study participants’ demographic characteristics
| Variable Description | HBIC | HC | Hospital | Total | |||||||
| N | % | N | % | N | % | N | % | ||||
| Sex | Female | 15 | 39.5 | 31 | 30.1 | 27 | 39.1 | 73 | 34.8 | ||
| Male | 23 | 60.5 | 72 | 69.9 | 42 | 60.9 | 137 | 65.2 | |||
| Age | 18-25 | 8 | 21.1 | 10 | 9.7 | 2 | 2.9 | 20 | 9.5 | ||
| 26-35 | 10 | 26.3 | 17 | 16.5 | 19 | 27.5 | 46 | 21.9 | |||
| 36-45 | 14 | 36.8 | 22 | 21.4 | 21 | 30.4 | 57 | 27.1 | |||
| 46-55 | 4 | 10.5 | 19 | 18.4 | 16 | 23.2 | 39 | 18.6 | |||
| 56-65 | 2 | 5.3 | 27 | 26.2 | 8 | 11.6 | 37 | 17.6 | |||
| 66+ | 0 | 0.0 | 8 | 7.8 | 3 | 4.3 | 11 | 5.2 | |||
| Marital Status | Divorces | 2 | 5.3 | 5 | 4.9 | 2 | 2.9 | 9 | 4.3 | ||
| Married | 23 | 60.5 | 75 | 72.8 | 25 | 36.2 | 123 | 58.6 | |||
| Single | 9 | 23.7 | 17 | 16.5 | 14 | 20.3 | 40 | 19.0 | |||
| Widowed | 4 | 10.5 | 4 | 3.9 | 4 | 5.8 | 12 | 5.7 | |||
| Education Level | Post grad. | 2 | 5.3 | 9 | 8.7 | 7 | 10.1 | 17 | 8.1 | ||
| Bachelor | 5 | 13.2 | 15 | 14.6 | 23 | 33.3 | 18 | 8.6 | |||
| Diploma | 2 | 5.3 | 25 | 24.3 | 5 | 7.2 | 18 | 8.6 | |||
| Certificate up to Level II | 15 | 43 | 33 | 32 | 10 | 14.4 | 48 | 20 | |||
| Read and write | 1 | 2.6 | 16 | 15.5 | 0 | 0.0 | 40 | 19.0 | |||
| Not attended Sch. | 13 | 34.2 | 5 | 4.9 | 0 | 0.0 | 11 | 5.2 | |||
| Occupation | Unemployment | 2 | 5.3 | 4 | 3.9 | 4 | 5.8 | 6 | 2.9 | ||
| Daily labor | 0 | 0 | 24 | 23.3 | 2 | 2.9 | 47 | 22.4 | |||
| Government | 10 | 26.3 | 9 | 8.7 | 13 | 18.8 | 29 | 13.8 | |||
| House wife | 17 | 44.7 | 14 | 13.6 | 3 | 4.3 | 15 | 7.1 | |||
| Retiree | 0 | 0 | 44 | 42.7 | 2 | 2.9 | 75 | 35.7 | |||
| Self Emp | 9 | 23.7 | 8 | 7.8 | 21 | 30.4 | 27 | 12.9 | |||
| Total | 38 | 100 | 103 | 100 | 69 | 100 | 210 | 100 | |||
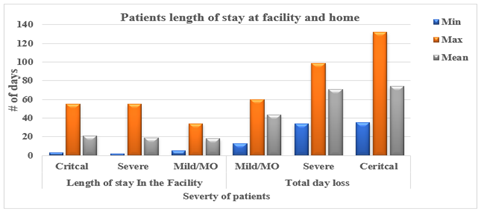
Looking at the total days lost in healthcare facilities and at home, as shown in Figure 2, hospitals recorded the highest number of days (Mean = 70.43 days) for the overall period, including both home care and hospital stays. In contrast, the average duration was shorter for home-based care. Moreover, the mean duration of hospital stays was notably longer (Mean = 19.25 days) compared to health centers (Mean = 13.83 days. For critical COVID-19 survivor patients, the total days lost ranged from 74 to 132 days, as illustrated in Figure 2, reflecting the variability in the length of recovery period from a minimum to maximum.
Figure 1: At the facility and total loss of days during COVID-19 treatment by severity from minimum to maximum.
The patient (direct nonmedical and indirect or productivity loss) cost estimated for COVID-19 case management were from USD16.8 to 82.52 per day per patient and USD235.91 to USD 1733.13 per patient per episode for HBIC and hospital critical care respectively as described based on table 3.
Table 3: Estimation of COVID-19 treatment cost by the level of severity and treatment setting per patient in (2021 USD) patient perspective
| Patient Cost | HBIC | Health Center | Hospital | |||
| Mild /moderate | Severe | Mild Moderate | Severe | Critical | ||
| Patient (Non-medical- Direct) Cost | 2 | 16 | 22 | 27 | 27 | 27 |
| Indirect (productivity loss) cost | 15 | 8 | 8 | 30 | 57 | 56 |
| Cost per Patient /day in USD | 17 | 24 | 30 | 57 | 83 | 83 |
| Cost per Patient per day in ETB | 699 | 1,003 | 1,233 | 2,363 | 3,458 | 3,458 |
| Cost per Patient /episode ETB | 9,790 | 14,037 | 19,721 | 42,527 | 65,706 | 71,925 |
| Cost per Patient/ episode USD | 236 | 338 | 475 | 1,025 | 1,583 | 1,733 |
ETB: Ethiopian birr, USD: united states dollar
Based on the health care perspective which is revealed by Error! Reference source not found.. The average cost of the health system per episode based were 1,416ETB (USD34) to 197,852 ETB (USD 4,768) for home-based isolation care to critical noninvasive patient respectively. The average patient daily cost per health system perspective were USD2 for HBIC to 277 for invasive management. The supply cost was the peak cost from USD2 for HBIC to USD 151 for critical invasive management and seconded by the personal cost USD 4,18 for mild/moderate to USD 51 for critical case per patient per day besides the building cost were the least cost when compere to other cost in this study based on the table 4 displayed.
Table 4: Cost for COVID-19 treatment by ingredient, level of severity and treatment setting per patient in (2021 USD) health care perspective
| HBIC | Health Center | Hospital | |||||
| Ingredient’s cost | Mild /Moderate | Severe | Mild Moderate | Severe | Critical NIV | Critical IV | |
| supply cost | 2 | 12 | 48 | 14 | 86 | 111 | 151 |
| Personals | 4 | 11 | 5 | 25 | 51 | 51 | |
| Equipment | 4 | 7 | 4 | 12 | 17 | 17 | |
| Building | 2 | 3 | 2 | 5 | 8 | 8 | |
| Per day in ETB | 101 | 920 | 2,865 | 1,099 | 5,297 | 7,768 | 9,422 |
| Per day in USD | 2 | 22 | 69 | 26 | 128 | 187 | 27 |
| Per episode in ETB | 1,416 | 12,887 | 5,845 | 19,780 | 100,644 | 163,125 | 197,853 |
| Per episode in USD | 34 | 311 | 1,105 | 477 | 2,425 | 3,931 | 4,768 |
ETB: Ethiopian birr, COVID-19: coronavirus disease, IV: invasive, NIV: noninvasive
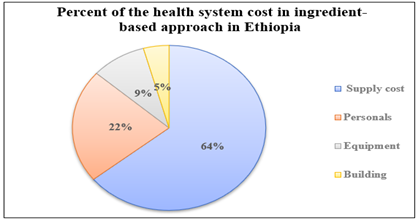
The significant health care cost of COVID-19 case management was supply cost and seconded by personal cost, which accounts for 64% and 22% respectively, followed by equipment cost (9%), and building cost (5%), (Figure 3).
Figure 2: Percent of health system cost in ingredient-based approach in Ethiopia.
Furthermore, the economic burden of the disease from the societal (patient and health system) perspective average cost per episode at the hospital innervation were $951, $3449, $5514, and $6500 for Mild /moderate, severe, invasive, and noninvasive management respectively per episode for hospital management of COVID -19 table 5 besides $38 mild/moderate and $93 severe case cost were utilized for COVID-19 case management at health center level
Table 5: Cost per episode for COVID-19 treatment, based on severity of cases Societal (Patient and health system) perspective (2021 USD)
| Health facility | Severity | Cost per Day | Cost per patient per episode | |||
| Mean | Mean | SD | Min | Max | ||
| Health Center | Mild /Moderate | 38 | 546 | 109 | 437 | 655 |
| Severe | 93 | 1442 | 288 | 1154 | 1731 | |
| Hospital | Mild Moderate | 56 | 951 | 190 | 761 | 1142 |
| Severe | 184 | 3449 | 689 | 2759 | 4139 | |
| Critical noninvasive | 270 | 5514 | 1102 | 4411 | 6616 | |
| Critical invasive | 309 | 6500 | 1300 | 5200 | 7800 | |
Cost was in 2021 USD; Min: Minimum: Max: Maximum.
Discussion
This study is groundbreaking given the absence of published data on the perspective of patient and healthcare system costs for managing COVID-19 cases in Ethiopia. The primary objective of this research was to assess the economic impact of COVID-19 case management in hospital settings, health centers, and home-based isolation care. By employing relevant cost appraisal methods, the study aimed to furnish policymakers with essential cost insights. Results indicated that managing COVID-19 incurred significant costs that escalated with the severity of cases, ranging from mild/moderate to critical conditions. Among the demographic characteristics of the COVID-19 patient participants, males were notably more affected and experienced more severe cases during the study period. Previous studies have consistently shown that males are more susceptible to and have higher mortality rates from COVID-19[16]. Notably, hospitalization rates in critical cases tend to be higher in men compared to women [27]. Observations from the study revealed a higher mortality rate among patients admitted to critical care units, particularly those requiring invasive mechanical ventilation. This aligns with prior research indicating a high fatality rate of COVID-19 patients in intensive care or critical wards[16].
The study also highlighted the impact of family size on the burden of COVID-19 treatment, where larger families demonstrated a higher likelihood of contracting the disease. This coincides with existing research on the contagious nature of COVID-19, showing an increased risk of infection in individuals from larger households[16]. The cost of COVID-19 treatment varied based on case severity and facility level, reflecting the differing resource requirements—such as capital, personnel, and operational costs—based on the severity of care and facility setting. The study indicated that costs per patient per day surged with the level of care provided, correlating with an elevated necessity for resources in managing COVID-19 cases from mild/moderate to critical conditions. Notably, critical cases, particularly those requiring invasive mechanical ventilation, demonstrated the highest costs, followed by severe cases and home-based isolation care[9]. In our research, we found that the primary expense in managing COVID-19 cases was attributed to supply costs, with personnel costs ranking second. Equipment and building costs followed in terms of expenditure. This discovery closely mirrored a prior study conducted in South Africa, which indicated that consumables and personnel costs accounted for the highest expenses in COVID-19 case management, while equipment costs represented a smaller proportion, ranging from 1% to 3% of the total costs[28].
The average facility length stays from14 day’s mild the moderate health center to 21 days for critical care those are admitted to the hospital. The pandemic has intensified demands on the burden of the health care system and resulted in critical shortages of resources ICU and ward beds, oxygen, ventilators, health professional, particularly in low-income countries like Ethiopia. The dally cost for home based isolation care cost, mailed/ moderate and hospital critical case cost were less than from South Africa [29].The cost difference may be in this study we are not included the risk communication and contact tracing cost and may be the country currency rate also difference the unit cost. In this finding the daily cost for patient for severe case was relatively comparable from the last study done in Myanmar[30]. This study reveals that among the consumable costs, the most significant expenses were related to oxygen, followed by medical personal protective equipment (PPE) costs. Our findings indicate that the unit cost for home-based isolation care is approximately half that of managing mild/moderate COVID-19 cases in health centers. Consistent with a previous study, our research highlights an escalation in the costs of COVID-19 management corresponding to the severity of the disease [28].
This study displayed the average daily cost in home-based isolation care, mild to moderate case and severe care management of the COVID -19 at hospital level were similar from previous study in Kenya but in this study the critical case daily cost was less than the previous Kenya study [8]. This may be the currency year of the exchange rate is different at the time of the study and dissimilar in health care worker salary rate per country. In this study finding to dally cost for COVID-19 milled/moderate, severe, and critical (noninvasive and invasive) case managed at hospital level was comparable with the last study of South Africa [28]. The study highlighted the significant economic burden imposed by COVID-19 case management in Ethiopia, a country with a per capita health expenditure of only USD 33[31]. It underscores the importance of promoting COVID-19 vaccination to reduce infection rates and disease severity, thereby mitigating financial strain. Establishing social security measures like social income insurance or disability benefits can help offset productivity losses and alleviate the substantial impact on household incomes.
Limitation and further research suggestions
Regarding limitations and future research recommendations, this study employed a costing model to estimate the economic burden of COVID-19 treatment, facing several constraints. Notably, the absence of published studies on societal cost analyses of COVID-19 treatment in Ethiopia hampers result comparisons. Additionally, certain cost items may fluctuate rapidly (e.g., PPE, reagents, drugs) or be based on estimated values, similar to those based on the Ethiopia Pharmaceutical Supply Agency (EPSA) data. Contact tracing costs and variations in costs related to COVID-19 risk factors were not assessed due to constraints in available resource data, though conditions like diabetes and cancer are recognized as risk factors for severe COVID-19 cases.
Conclusion
This study provides significant evidence for policy maker and planner related to COVID-19 and other similar outbreak These results indicated that the critical case of the disease extremely carries a high cost in this event. It is projected that the high prevalence rate of COVID-19 has been imposing a heavy economic burden on the health system and patients and even in the country. Thus, high awareness needs to prevent to minimize the amount of cost because worsening COVID-19 burdens could add to the rising loss of life, resources, and productivity.
Abbreviation
CFD: Case Fatality Rate; ECG: Electrocardiography; CPAP: continuous positive airway pressure; EPSA: Ethiopia Pharmaceuticals Supply Agency; ETB: Ethiopian Birr; HDU; High Dependency Unit; PPE: HBIC: Home Based Isolation Care Personal; Protective Equipment; NG: Nasogastric; ICU: Intensive Care Unit; IV: Intravenous; USD: Untied Studs Dollar
Declarations
Acknowledgments
The author would like to thank you personnel’s who are working on critical care in Eka kotbe hospital COVID -19 treatment center for their valuable support during data collection time.
Funding
There is no fund for this work
Availability of data and materials
All data supporting results will be available on official request to the corresponding author.
Ethical approval
The Ethiopian public health institute's, Institutional Review Board approved this study.
Consent for publication
Not applicable.
Competing interests
None
References
- Ju J, Wei SJ, Savira F, et al. No 主観的健康感を中心とした在宅高齢者における 健康関連指標に関する共分散構造分析. J Chem Inf Model 2020(e) ; 43:7728.
Publisher | Google Scholor - Barendregt JJ, van Oortmarssen GJ, Vos T, et al. (2003). A generic model for the assessment of disease epidemiology: The computational basis of DisMod II. Popul Health Metr, 1:1-8.
Publisher | Google Scholor - World Health Organization. (2020). Coronavirus Disease (COVID-19) Situation Reports Updates 27 September 2020. World Health Organ Tech Rep Ser, 1-23.
Publisher | Google Scholor - FMOH E. (2020). Covid19 Management Handbook. FMOH, Ethiop First Ed April, 7-9.
Publisher | Google Scholor - (2019). WHO Coronavirus Disease (COVID-19) Dashboard.
Publisher | Google Scholor - (2020). Handbook of COVID-19 prevention and treatment. Zhejiang: First Affiliated Hospital of Zhejiang University School of Medicine.
Publisher | Google Scholor - Ismaila H, Asamani JA, Lokossou VK, et al. The cost of clinical management of SARS-COV-2 (COVID-19) infection by level of disease severity in Ghana: a protocol-based cost of illness analysis. BMC Health Serv Res 2021(e)ko ; 21: 1–10.
Publisher | Google Scholor - Barasa E, Kairu A, Ng Ang A W, et al. (2020). Examining unit costs for COVID-19 case management in Kenya. BMJ Glob Heal 6.
Publisher | Google Scholor - Ghaffari Darab M, Keshavarz K, Sadeghi E, et al. (2021). The economic burden of coronavirus disease 2019 (COVID-19): evidence from Iran. BMC Health Serv Res, 21:1-7.
Publisher | Google Scholor - Polsky D, Glick HA, Willke R, et al. (1997). Confidence intervals for cost-effectiveness ratios: A comparison of four methods. Health Econ, 6:243-252.
Publisher | Google Scholor - Rice DP, Hodgson TA, Kopstein AN. (1985). The economic costs of illness: A replication and update. Health Care Financ Rev 7:61-80.
Publisher | Google Scholor - Barnum H, Kutzin J. (1993). Public hospitals in developing countries: resource use, cost, financing. Public Hosp Dev Ctries Resour use.
Publisher | Google Scholor - Olyaeemanesh A, Woldemichael A, Takian A, et al. (2019). Availability and inequality in accessibility of health centre-based primary healthcare in Ethiopia. PLoS One, 14:1-16.
Publisher | Google Scholor - Ethiopia A and U. (2020). Multidimensional Child Deprivation in Ethiopia. UNON Publ Serv Sect Nairobi.
Publisher | Google Scholor - Demiessie H. (2020). The Effect of Covid-19 Pandemic on Macroeconomic Stability in Ethiopia.
Publisher | Google Scholor - Alene KA, Gelaw YA, Fetene DM, et al. (2021). COVID-19 in Ethiopia: A geospatial analysis of vulnerability to infection, case severity and death. BMJ Open, 11:1-11.
Publisher | Google Scholor - Cunnama L, Garcia Baena I, Gomez G, et al. (2020). Costing guidelines for tuberculosis interventions.
Publisher | Google Scholor - Hailu A, Lindtjørn B, Deressa W, et al. (2018). Cost-effectiveness of a combined intervention of long-lasting insecticidal nets and indoor residual spraying compared with each intervention alone for malaria prevention in ethiopia. Cost Eff Resour Alloc, 16:1-17.
Publisher | Google Scholor - Rezapour A, Souresrafil A, Peighambari MM, et al. (2021). Economic evaluation of programs against COVID-19: A systematic review. International Journal of Surgery, 85:10-18.
Publisher | Google Scholor - WHO. (2021). World Health Organization COVID-19 Essential Supplies Forecasting Tool COVID-19 ESFT, 1-14.
Publisher | Google Scholor - Yigezu A, Alemayehu S, Hamusse SD, et al. (2020). Cost-effectiveness of facility-based, stand-alone and mobile-based voluntary counseling and testing for HIV in Addis Ababa, Ethiopia. Cost Eff Resour Alloc, 18:1-12.
Publisher | Google Scholor - Alemayehu S, Yigezu A, Hailemariam D, et al. (2020). Cost-effectiveness of treating multidrug-resistant tuberculosis in treatment initiative centers and treatment follow-up centers in Ethiopia. PLoS One, 15.
Publisher | Google Scholor - Neyeloff JL, Fuchs SC, Moreira LB. (2012). Meta-analyses and Forest plots using a microsoft excel spreadsheet: Step-by-step guide focusing on descriptive data analysis. BMC Res Notes, 5.
Publisher | Google Scholor - Power T. (2021). Methods for the Economic Evaluation of Health Care Interventions for Priority Setting in the Health System. WHO CHOICE, 10:673-677.
Publisher | Google Scholor - Drummond MF, O’Brien B, Stoddart GL, et al. (1998). Methods for the Economic Evaluation of Health Care Programmes, Second Edition. Am J Prev Med, 14:243.
Publisher | Google Scholor - Cleary SM, Wilkinson T, Tamandjou Tchuem CR, et al. (2021). Cost‐effectiveness of intensive care for hospitalized COVID-19 patients: experience from South Africa. BMC Health Serv Res, 21.
Publisher | Google Scholor - Oksuz E, Malhan S, Gonen MS, et al. (2021). COVID-19 healthcare cost and length of hospital stay in Turkey: retrospective analysis from the first peak of the pandemic. Health Econ Rev, 11:1-122.
Publisher | Google Scholor - Edoka I, Fraser H, Jamieson L, et al. (2021). Inpatient Care Costs of COVID-19 in South Africa’s Public Healthcare System. Int J Heal Policy Manag, 1-8.
Publisher | Google Scholor - Torres-Rueda S, Sweeney S, Bozzani F, et al. (2020). The health sector cost of different policy responses to COVID-19 in low- And middle- income countries. MedRxiv, 20180299-20180299.
Publisher | Google Scholor - Thant PW, Htet KT, Win WY, et al. (2021). Cost estimates of COVID-19 clinical management in Myanmar. BMC Health Serv Res, 1-10.
Publisher | Google Scholor - Republic FD. Ministry of Health.
Publisher | Google Scholor