Case Report
Endovascular And Open-Surgery Treatment of Iatrogenic A-V Fistula
- T. Samardjiev
- Iva Kostadinova *
Vascular surgery clinic, Heart and Brain Center of Clinical Excellence, Pleven, Bulgaria.
*Corresponding Author: Iva Kostadinova, Vascular surgery clinic, Heart and Brain Center of Clinical Excellence, Pleven, Bulgaria.
Citation: Samardjiev T, Kostadinova I. (2024). Endovascular And Open-Surgery Treatment of Iatrogenic A-V Fistula. Clinical Case Reports and Studies, BioRes Scientia Publishers. 5(4):1-5. DOI: 10.59657/2837-2565.brs.24.119
Copyright: © 2024 Iva Kostadinova, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: March 12, 2024 | Accepted: March 26, 2024 | Published: March 25, 2024
Abstract
Introduction: Arterio-venous (AV) fistulas represent abnormal communications between arteries and veins. AV fistulas can be congenital or acquired, trauma and iatrogenic are in the base of the etiology in acquired fistulas. We present you a case of iatrogenic AV fistula after a completed surgical intervention (microdiscectomy) in the lumbar spine.
Clinical Case: 49-year-old woman was hospitalized in the Vascular surgery clinic at Heart and Brain Center of Clinical Excellence, Pleven with complaints of oedema, cyanosis and tingling sensations in left lower extremity after three completed surgical interventions in the lumbar spine. Computer tomography assisted angiography showed communication between the common iliac artery and common iliac vein on the left side. We assessed that the patient qualified for endovascular treatment – implantation of stent-graft in the common iliac artery. On the first day after surgery, during a control examination with ultrasound in the area of the puncture we found AV communication between common femoral artery and superficial venous varicosity. With thoughts about secondary closing of the communication, the patient was released from the hospital with visible clinical improvement. At the first control exam, we acknowledged that the AV communication still persists, the patient was hospitalized for surgical ligation of the AV fistula. The intervention was done with local anesthesia, without stay in the reanimation ward and with full range of recovery movements. On the second day, she was released with double antiplatelet therapy.
Conclusion: AV fistulas are diseases that lead to lowering the quality of life of the patients. Deep vein thrombosis (DVT) is leading in the differential diagnosis. The accurate diagnosis determinates the method of treatment. With the evolution of endovascular techniques, this type of treatment is becoming a method of choice for AV fistulas.
Keywords: av fistula; dvt; stent-graft; iatrogenic
Introduction
Arterio-venous (AV) fistulas represent abnormal communications between arteries and veins. First described from William Hunter in 1761 year, the said description contains the changes that come from this variation – enlargement of the diameter of the artery proximal to the communication and weakening of the arterial pulse distally. The changes in the vein are characterized with “thrill” and venous pulsations. AV fistulas can be congenital or acquired, trauma and iatrogenic are in the base of the etiology in acquired fistulas. In modern times, the number of iatrogenic AV fistulas show tendency to increase. The natural occurrence of the AV fistulas is relatively benign, as 38% - 81% undergo a spontaneous closure. [1] Iliac AV fistulas are rare (0,4% - 1, 4%), they are usually result of penetrating trauma and microdiscectomy. In the latter case, the left common iliac artery and vein are most commonly affected [2]. 49-year-old woman was hospitalized in the Vascular surgery clinic at Heart and Brain Center of Clinical Excellence, Pleven with established diagnosis of AV fistula between left common iliac artery and left common iliac vein.
Clinical Case
We present you a case of 49-year-old woman with three surgeries in the Neurosurgery ward-microdiscectomy of the lumbar vertebrae, the last surgery was in the month of May 2021. After the last intervention, she develops, oedema, cyanosis and tingling sensations in the lower left extremity. Previously, she had two conservative treatments in another Vascular surgery ward in another hospital, where the established diagnosis was deep vein thrombosis (DVT). The prescribed therapy was a direct oral anticoagulant. After the treatment, the complaints only got worse, dyspnea and tiredness during physical activity, the oedema of the extremity got enlarged to the point where the ankle and knee couldn’t perform full range of movements. Dilated and pulsating veins appeared on the abdomen.
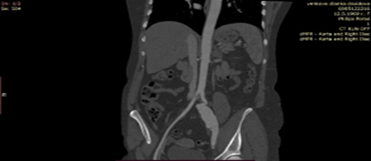
During the physical exam we acknowledged intense swelling of the lower left extremity, cyanosis, varicose superficial veins and weakened peripheral pulse. On the abdomen, on left, there was a developed collateral network of the superficial veins with thrill on palpation. After a Doppler ultrasound, we saw unobstructed deep veins, raised venous pressure and pulsations. Without data for past DVT. On the CT angiography we found: 1. On the level of the left common iliac artery was a communication with the left common iliac vein. 2. the left common iliac vein was contrasted in the arterial phase and was dilated 37/25mm. 3. The size of the communication in axillary view was 6.8mm. 4. Multiple contrasted and tortuous veins on the abdomen [Figure 1, 2].
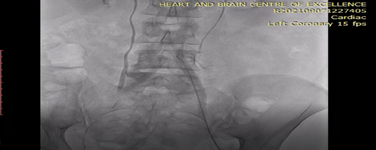
After the completed diagnostics, we laid down the possible options for treatment – endovascular treatment with implantation of arterial stent graft to isolate the AV fistula, another was surgical treatment with retroperitoneal access and ligation of the AV fistula. The advantages and disadvantages of the said methods are described in [Table 1, 2]. The doctor team decided the endovascular treatment. For the procedure we used local anesthesia with 1% Lidocaine solution. With a retrograde puncture access to the left common femoral artery where we set up the guide to the left external iliac artery where a 6fr. Short arterial introducer was put. With a control angiography the definite position of the communication was confirmed. Under an X-ray control, a hydrophilic guide was put in the abdominal aorta and after that a stent graft Advanta 7x59mm was placed. Post dilatation was done with a balloon 8x40mm. We received an optimal angiographic result after the procedure. The interventional equipment was removed and a compressive dressing was applied for 12 hours. [Figure 3,4,5].
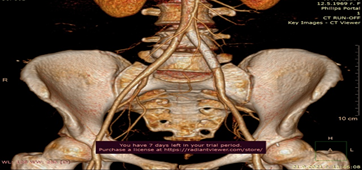
On the first post-operative day, during ultrasound control exam in the area of the puncture, we found AV communication between left common femoral artery and a superficial venous varicosity. With thoughts about secondary closing of the communication, the patient was released from the hospital with visible clinical improvement – reduced oedema, no thrill on palpation on the superficial varicosities of the abdomen. There was existing pulse of the foot arteries. Ten days after de hospitalization, the patient came in for a control exam, she stated that the complaints have reduced but the swelling was still present accompanied by buzzing in the inguinal region. We came to a decision for surgical ligation of the AV communication. The intervention was done under local anesthesia, on the first post-operative day the patient had full range of motions. After a control CT angiography, the following things were found: 1. The implanted stent in left common iliac artery was unobstructed 2. Multiple contrasted and tortuous veins on the abdomen that do not fill during the arterial phase of contrasting. [Figure 6,7]. The patient was discharged on the second post-operative day with double antiaggregant therapy, with recommendations of passing to monotherapy in the third month after discharge.
Figure 1: Multiple contrasted and tortuous veins on the abdomen.
Table 1: Endovascular treatment.
| Advantages | Disadvantages |
| micro invasive procedure; | Expensive equipment; |
| low blood loss; | Expensive implant; |
| without stay in reanimation ward; | non-reimbursed implant; |
| short intervention; | In need of qualified personnel; |
| short recovery period; | |
| Local anesthesia; |
Figure 2: A-V communication between left common iliac vein and artery
Table 2: Surgical treatment
| Advantages | Disadvantages |
| 1.Low-cost intervention; | 1.large blood loss; |
| 2.No X-ray radiation; | 2. necessity for general anaesthesia; |
| 3.large surgical access; | |
| 4.stay in reanimation ward is necessary; | |
| 5.prolonged recovery period; |
Figure 3: Selective angiography of the A-V fistula.
Figure 4: Implantation of stent-graft in AIC sin.
Figure 5: Angiography: covered A-V fistula
Figure 6: Unobstructed stent in common iliac artery.
Figure 7: Unobstructed stent in common iliac Iliac
Discussion
AV fistulas are rare (0, 4% - 1, 4%). Usual symptoms are: dyspnea, tachycardia, lower extremity edema, low levels of haemoglobin, heart murmur and developed collateral network of the superficial veins on the abdomen.[4] When such communication is present, right to left shunt is formed which results in higher volume of blood in the inferior vena cava, right atrium and right ventricle. The increased load for prolonged periods results in pulmonary hypertension, hypertrophy of the right ventricle leading to right sided heart failure with systemic venous congestion. The diferential diagnosis contains: deep vein thrombosis, pulmonary embolism, primary pulmonary hypertension, congenital AV fistula. Carefully taken anamnesis, physical exam and combination of Doppler ultrasound with minimal invasive imaging method of the blood vessels (CT angiography, MRI) are essential for establishing correct diagnosis and choosing the method of treatment. The traditional surgery includes: ligation, patch angioplasty, interposition of prosthesis, excision followed by termino-terminal anastomosis [5]. Options for endovascular treatment are embolization, implantation of venous or arterial stentgraft or combination of both. Globally the method of choice is the endovascular surgical treatment because of the significantly lower blood loss and intervention time and the quick recovery of the patients [6].
Conclusion
AV fistulas are diseases that lead to lowering the quality of life of the patients. Unrecognizing them or late treatment rise the risk of developing heart failure or arterial or venous insufficiency. With the evolution of endovascular techniques, this type of treatment is becoming a method of choice for AV fistulas. The tehniques that can be used are transcathetric embolization, implantation of stentgraft or both combined [3].
References
- Rutherford Vascular Surgery 8th Edition, Ch.86:1268;
Publisher | Google Scholor - Rutherford Vascular Surgery 8th Edition, Ch.86:1271;
Publisher | Google Scholor - Parodi JC. (1996). Endovascular repair of aortic aneurysms, arteriovenous fistulas and false aneurysms. World J Surg, 20:655-663.
Publisher | Google Scholor - Guo-Qing Yang et all. Iatrogenic arteriovenous fistula of the iliac artery after lumbar discectomy surgery: a systematic review of the last 18 years.
Publisher | Google Scholor - Papadoulas S, Konstantinou D, Kourea HP, Kritikos N, Haftouras N, et al. (2022). Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg, 24:189-195.
Publisher | Google Scholor - Schonholz CJ, et al. (2007). Stent-graft treatment of trauma to the supra-aortic arteries. J Cardiovasc Surg, 48:537-549.
Publisher | Google Scholor - Ocal, O., Peynircioglu, B., Eldem, G., Akpinar, E., Onur, et al. (2017) Iliac Arteriovenous Fistulas after Lumbar Spinal Surgery. Turkish Journal of Emergency Medicine, 17:109-111.
Publisher | Google Scholor - Mohamed A. Khoudir, Ghassan M. Aweja, Abdulkarim M. Katebi, Ahmed Farag, et al. Case Report: Post Lumbar Discectomy Acute Iliac Arteriovenous Fistula. Endovascular Management and Literature Review.
Publisher | Google Scholor - Osman Ocal a, Bora Peynircioglu a , Gonca Eldem a , Erhan Akpinar a , Mehmet Ruhi Onur et al. Iliac arteriovenous fistulas after lumbar spinal surgery.
Publisher | Google Scholor