Research Article
Efficacy of Pectoralis Nerve Block Versus General Anesthesia for Postoperative Analgesic Requirements and Patient Satisfaction After Radical Mastectomy: Romanized Clinical Trial (RCT)
- Amjed Qasim Mohammed 1,3*
- Mohamed Kahloul 2
- Mohammed Abbas Kadhim 4
- Mohammed Sadeq Karam Al-Ghanimi 4
1Faculty of Medicine, Department of Anesthesia, University of Sousse, Tunesia.
2Department of Anesthesia and Intensive Care, Teaching Hospital of Sahloul, University of Medicine ibn Jazzar, Tunisia.
3Department of Anesthesia, College of Health and Medical Technology, Al-Manara University, Iraq.
4Anesthesiologist, Missan Health Directorate, Al-Zahrawi General Teaching Hospital. Iraq.
*Corresponding Author: Amjed Qasim Mohammed, Faculty of Medicine, Department of Anesthesia, University of Sousse, Tunesia.
Citation: Amjed Q. Mohammed, Kahloul M, Mohammed A. Kadhim, M.S.K. Al-Ghanimi. (2024). Efficacy of Pectoralis Nerve Block Versus General Anesthesia for Postoperative Analgesic Requirements and Patient Satisfaction After Radical Mastectomy: Romanized Clinical Trial (RCT), International Journal of Clinical and Surgical Pathology, BioRes Scientia Publishers. 1(1):1-10. DOI: 10.59657/3067-0462.brs.24.005
Copyright: © 2024 Amjed Qasim Mohammed, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 19, 2024 | Accepted: August 02, 2024 | Published: August 09, 2024
Abstract
Introduction: Our objectives for this study are to evaluate the efficiency of postoperative analgesia in radical mastectomy (RM) surgeries at Al-Zahrawi Hospital in Iraq, specifically investigating the results of Pectoral Nerve Blocks (PECs) and General Anesthesia (GA).
Methods: The research was conducted at Al-Zahrawi Hospital, a specialized hospital within Amara Health hospitals in Iraq that offers care for over 1000 patients who have general operations each month. There is a specialist center for breast cancer that provides analgesia treatment and mastectomy operations besides chemotherapy and radiotherapy. Also, there are approximately five patients in this center who are participating in our study monthly, because they are undergoing radical mastectomy. We selected 75 patients and divided them into three groups of 25 patients each group. The first group received general anesthesia, the second group received Pecs Block, and the third group received combined techniques.
Results: The outcomes of this study revealed that there are statistically significant changes between the study groups in favor of PECs block in terms of reducing postoperative analgesic requirements, increasing patient satisfaction, decreasing postoperative complications, and there is no admission to the ICU and decreasing hospital stays.
Conclusion: The research conducted at Al-Zahrawi Hospital in Iraq has produced significant results regarding techniques of pain management for radical mastectomy surgeries by demonstrating the efficacy of Pectoral Nerve Block (Pecs Block) versus General Anesthesia (GA) in postoperative analgesia for radical mastectomy operations. In this study, research was conducted to evaluate and assess the efficacy of two separate practices in mitigating postoperative pain, with the ultimate objective of improving overall patient satisfaction and surgical results.
Keywords: radical mastectomy; postoperative analgesic requirements; general anesthesia; pectoral nerve block; breast cancer
Introduction
Breast cancer is the most frequent cancer in women worldwide, representing 1.38 million new cancer cases diagnosed in 2018, constituting 23% of all cancer cases in women [1]. It is now the most common cancer both in developed and developing countries. Iraq developed national programs for the early detection of breast cancer as proposed by the World Health Organization (WHO) to decrease breast cancer mortality [2]. In common cases, partial or total mastectomy combined with axillary examination is required for the management of breast cancer [3]. Mastectomy can be associated with increased postoperative pain, delayed ambulation, and a significant risk of complications. A systemic opioid is the primary analgesic option after the operation. However, opioid administration is associated with side effects like PONV, respiratory depression, hyperalgesia, and immunosuppression [4]. Acute postoperative pain following breast cancer surgery is often disregarded because the procedure is considered minimally invasive. However, if acute pain management is neglected, most patients will develop chronic post-mastectomy pain which reduces the quality of life [5].
To manage acute pain after breast cancer surgery, regional anesthesia is recommended [6]. As fentanyl is associated with a risk of vomiting and nausea. Therefore, to avoid the risk of postoperative nausea and vomiting, the injection of fentanyl is discouraged. Regional anesthesia such as thoracic epidural block (TEB) and thoracic paravertebral block (TPVB) can provide effective postoperative pain relief after breast cancer surgery [7]. However, as the TEB and the TPVB are deep nerve blocks (level), need multiple injections, more a higher failure rate, and are more economical, therefor in our study we are hesitant to perform these techniques [8]. Pectoral nerves (PECS) block, previously described by Blanco et al, can anesthetize the intercostobrachial, lateral cutaneous branch, medial cutaneous nerve of the arm and forearm, and long thoracic and thoracodorsal nerves, which are analgesic at the lateral mammary area. Therefore, we imagined that the combination of GA and PECS block would offer effective analgesia for Mastectomy. However, there are a few reports of the efficacy of PECS’s block [9].
The objectives of our study are to compare post-operative analgesic efficacy, decrease length of hospital stay (LOS), decrease opioid-related adverse effects (nausea, vomiting), and patient satisfaction regarding radical modified mastectomy for patients undergoing general anesthesia, PEC block, or combined technique. In addition to investigating the efficacy of ultrasound- guided PECS block for Mastectomy. So, introduce ultrasound-guided local anesthetic infiltration of the tissue plane between the pec1 and pec2 muscles to anesthetize the pectoral nerves. The technique was subsequently modified with an additional injection to block the upper intercostal nerves which supply the chest and axilla and named the PECs II block. This is naturally done with the patient in the supine position, under U/S, with the administration local anesthetic dose of 0.4 ml.kg-1 0.25% Livobupivacain. As suggested by Blanco, this is a fairly simple technique to learn, provides good analgesia, and avoids the risk of complications associated with PVB and thoracic epidurals (TEB) such as sympathetic blockade, risk of dura puncture, and unintentional bilateral block.
Methods
This study followed a randomized clinical trial design, conducted at Al-Zahrawi Teaching Hospital after obtaining ethical approval from the Ministry of Health's ethical committee in Iraq. The study was conducted over a fourteen-month period, from February 2022 to March 2023. And emitting permits schedule for radical mastectomy surgeries without axillary clearance. The research was conducted at Al-Zahrawi Teaching Hospital, a specialized hospital within Missan Health hospitals that provides care for over 1000 patients undergoing general surgeries each month. The hospital has a dedicated area for breast cancer patients, offering analgesic treatments and mastectomy surgeries, in addition to chemotherapy and radiation therapy. Approximately three to six eligible patients were enrolled in the study each month. Inclusion criteria were adult females aged 20 to 55 years old having an American Society of Anesthesiologists (ASA) physical status I or II.
Exclusion Criteria
All the patients who had undergone multiple regional anesthesia procedures, individuals with contraindications to peripheral nerve blocks, severe cardiopulmonary disease, renal and liver dysfunction multiple organ failure, known or suspected neurologic deficits, mental illness, skin infections at the puncture site, coagulation disorders, allergies to local anesthetics, prolonged use of opioids or non-steroidal anti-inflammatory drugs, refusal of pectoral nerve blocks, and those not followed up for more than 24 hours.
Participant Recruitment: Participants were employed by the Al-Zahrawi Teaching Hospital. Informed consent was obtained from the patients or their legal guardians, ensuring they understood the study's objectives and the use of regional anesthesia. After obtaining ethical approval from the Ministry of Health ethical committee in Iraq were randomly assigned to one of three groups (Group A - General Anesthesia, Group B - PECS Blocks, Group C - Combination of General Anesthesia and PECS Blocks) using sealed opaque envelopes. The blinding process ensured that both the researcher and medical staff in the ward were unaware of the type of anesthesia administered.
Randomization: Computer-generated random numbers were used to allocate patients into the three groups. The random allocation was concealed within sealed envelopes, which were opened after patient enrollment. Data collection occurred postoperatively, with the researcher collecting and recording samples while him still unaware of the type of anesthesia each patient received.
Data Collection: Data collection was executed using private information forms assigned to each study participant, with a unique serial number associated with the type of anesthesia used during surgery. This approach ensured that collected data remained confidential and could be categorized by the anesthesia type without revealing patient identities.
Statistical Analysis
The collected data was revised, coded, and tabulated using the Statistical Package for Social Science (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Data were presented and suitable analysis was done according to the type of data obtained for each parameter.
Descriptive statistics: Mean, Standard deviation (± SD), Standard error (± SE), Median, and range for distributed numerical data. Frequency and percentage of non-numerical data.
Analytical statistics: Chi-Square test was used to examine the relationship between two qualitative variables.
Fisher Exact or Monte Carlo test: was used to examine the relationship between two qualitative variables when the expected count is less than 5 in more than 20% of cells. A paired T-test was used to assess the statistical significance of the difference between the two periods. One Way ANOVA test was used to assess the statistical significance of the difference between more than two study group parametric variables and used “Tukey” for pairwise comparison. ANOVA with repeated measures test was used to assess the statistical significance of the difference between more than two periods of parametric variables and used “Bonferroni” for pairwise comparison. The Kruskal-Wallis test was used to assess the statistical significance of the difference between more than two study group nonparametric variables and used “Dunn's” for pairwise comparison. The Freidman test was used to assess the statistical significance of the difference between more than two periods of non-parametric variables and used “Dunn's” for pairwise comparison.
Probability of Results: A p value is considered significant if lessthan 0.05 at confidence interval 95%.
Results
A comparative analysis was conducted among three distinct groups, each receiving various treatment modalities: general anesthesia (GA), pectoralis muscle plane block (PECS block), and a combined approach involving both GA and PECS block. The sample size for each group consisted of 25 female participants. The average age was comparable among the three groups: general anesthesia (GA) group (47.40 ± 8.11 years), pectoralis nerve block (PECS block) group (46.44 ± 9.42 years), and GA with PECS block group (48.28 ± 8.70 years). The obtained p- value exceeded the threshold of 0.05, indicating a lack of statistically significant variation in age across the different groups. The average weight was comparable among the three groups: general anesthesia (GA) group (80.52 ± 7.93 kg), pectoral nerves (PECS) block group (82.04 ± 5.33 kg), and GA with PECS block group (77.92 ± 7.29 kg). The obtained p-value of 0.112 indicates that there is no statistically significant difference in weight between the groups. The average height exhibited minimal variation among the three groups: general anesthesia (GA) group had a mean height of 158.0 ± 4.68 cm, the PECS block group had a mean height of 160.8 ± 3.38 cm, and the GA with PECS block group had a mean height of 159.5 ± 4.24 cm. The obtained p-value indicated that there was no statistically significant variation in height between the different group (Table 1).
Table 1: Comparison between the three studied groups regarding to personal data.
| GA (n=25) | PECS block (n=25) | GA with PECS block (n=25) | Test | P Value | |
| Age (years) | |||||
| Mean ± SD | 47.40 ± 8.11 | 46.44 ± 9.42 | 48.28 ± 8.70 | F= 0.276 | 0.760 |
| Min - Max | 25.0 – 58.0 | 26.0 – 59.0 | 32.0 – 60.0 | ||
| Weight(kg) | |||||
| Mean ± SD | 80.52 ± 7.93 | 82.04 ± 5.33 | 77.92 ± 7.29 | F= 2.255 | 0.112 |
| Min - Max | 67.0 – 100.0 | 70.0 – 91.0 | 68.0 – 90.0 | ||
| Height(cm) | |||||
| Mean ± SD | 158.0 ± 4.68 | 160.8 ± 3.38 | 159.5 ± 4.24 | F= 2.706 | 0.074 |
| Min - Max | 150.0 – 168.0 | 154.0 – 167.0 | 154.0 – 170.0 | ||
SD.: Standard deviation, Min.: Minimum, Max.: maximum, F: One Way ANOVA test, P value comparing between the three studied groups.
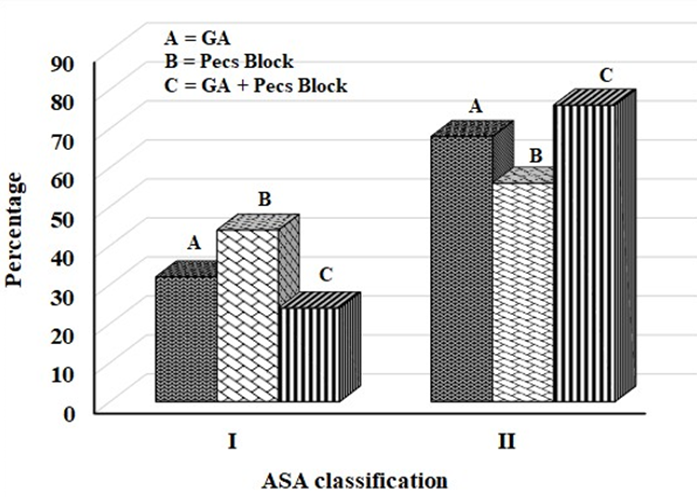
According to the data existing in the table, it can be observed that all the patient population, involving 25 patients in each group, underwent a radical mastectomy procedure. This suggests that there was an absence of difference in the nature of the procedure among the three cohorts. The ASA (American Society of Anesthesiologists) classification was employed for the evaluation of patients' physical condition prior to surgical procedures. The results indicated that there was no statistically significant difference detected among the three groups under analysis in terms of ASA. Table 2 and Figure 1.
Table 2: Comparison between the three studied groups regarding to ASA classification.
| GA (n=25) | PECS block (n=25) | GA with PECS block (n=25) | Test | P Value | ||||
| No | % | No | % | No | % | |||
| Type of operative | ||||||||
| Mastectomy | 25 | 100.0 | 25 | 100.0 | 25 | 100.0 | - | - |
| ASA classification | ||||||||
| I | 8 | 32.0 | 11 | 44.0 | 6 | 24.0 | ◻2=2.280 | 0.320 |
| II | 17 | 68.0 | 14 | 56.0 | 19 | 76.0 | ||
◻2: Chi–Square, P value comparing between the three studied groups.
Figure 1: Column chart for comparison between the three studied groups regarding to ASA classification.
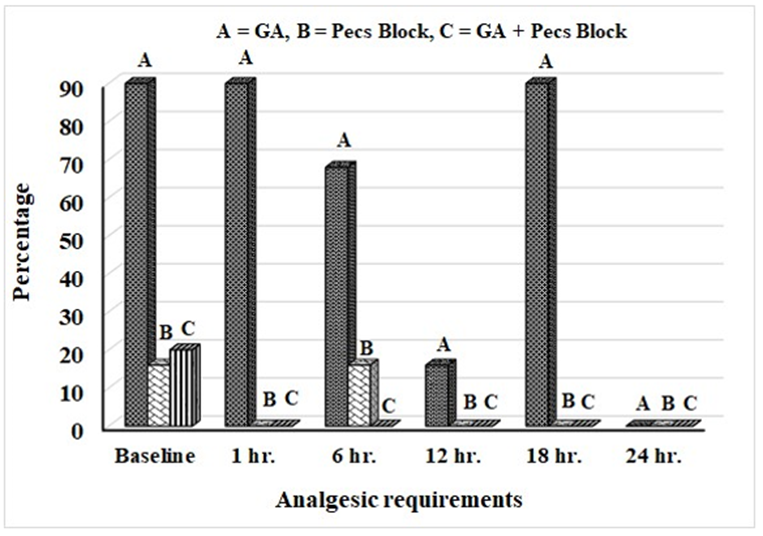
According to the table 3 the PECS block and GA with PECS block groups had higher rates of patients not requiring analgesic medication after surgery (84.0% and 80%, respectively), compared to only 4% of the GA group (p lessthan 0.001). After one hour, 96% of GA patients needed Paracetamol after 18 hours. None of the pectoral nerves (PECS) block or GA plus PECS block patients needed analgesics. The observed difference was statistically significant at p lessthan 0.05. After 6 hours, 68% of GA patients needed analgesics (Ketrolac). A total of 16% of patients in the pectoral nerves (PECS) block group needed analgesics (Ketrolac), while none in the GA with PECS block group needed any. This shows that the general anesthesia (GA) group needed more analgesics than the pectoral nerves (PECS) block group and the combined GA with PECS block group. The statistical significance threshold (p lessthan 0.05) suggests that the observed outcomes are unlikely to be random. After 12 hours, the group given general anesthesia (GA) had more patients needing analgesics than the other two. After 24 hours, no experimental group had significant differences in analgesic demands. Table 3 and Figure 2 follow.
Table 3: Comparison between the three studied groups regarding to analgesic requirements.
| Type of analgesic requirements postoperative | GA (n = 25) | ECS block (n=25) | GA with PECS block (n=25) | ◻2 | P1 | P2 | P3 | P4 | |||
| No | % | No | % | No | % | ||||||
| Baseline | |||||||||||
| Non | 1 | 4.0 | 21 | 84.0 | 20 | 80.0 | 75.624 | MC lessthan 0.001* | MC lessthan 0.001* | MC lessthan 0.001* | FE 1.000 |
| Tramadol | 24 | 96.0 | 0 | 0.0 | 0 | 0.0 | |||||
| Paracetamol | 0 | 0.0 | 4 | 16.0 | 5 | 20.0 | |||||
| 1 hour | |||||||||||
| Non | 1 | 4.0 | 25 | 100.0 | 25 | 100.0 | 70.588 | lessthan 0.001* | lessthan 0.001* | lessthan 0.001* | – |
| Paracetamol | 24 | 96.0 | 0 | 0.0 | 0 | 0.0 | |||||
| 6 hours | |||||||||||
| Non | 8 | 32.0 | 21 | 84.0 | 25 | 100.0 | 46.554 | MC lessthan 0.001* | MC lessthan 0.001* | lessthan 0.001* | FE 0.110 |
| Tramadol | 0 | 0.0 | 4 | 16.0 | 0 | 0.0 | |||||
| Ketorolac | 17 | 68.0 | 0 | 0.0 | 0 | 0.0 | |||||
| 12 hours | |||||||||||
| Non | 21 | 84.0 | 25 | 100.0 | 25 | 100.0 | 6.088 | MC 0.031* | 0.037* | 0.037* | – |
| Tramadol | 4 | 16.0 | 0 | 0.0 | 0 | 0.0 | |||||
| 18 hours | |||||||||||
| Non | 1 | 4.0 | 25 | 100.0 | 25 | 100.0 | 70.588 | lessthan 0.001* | lessthan 0.001* | lessthan 0.001* | – |
| Paracetamol | 24 | 96.0 | 0 | 0.0 | 0 | 0.0 | |||||
| 24 hours | |||||||||||
| Non | 25 | 100.0 | 25 | 100.0 | 25 | 100.0 | – | – | – | – | – |
◻2: Chi–Square, MC: Monte Carlo, FE: Fisher exact, P1: Comparing the three studied groups, P2: Comparing GA and PECS block, P3: Comparing GA and GA with PECS block, P4: Comparing PECS block and GA with PECS block, *: Significant when p lessthan 0.05.
Figure 2: Column chart for comparison between the three studied groups regarding to analgesic requirements.
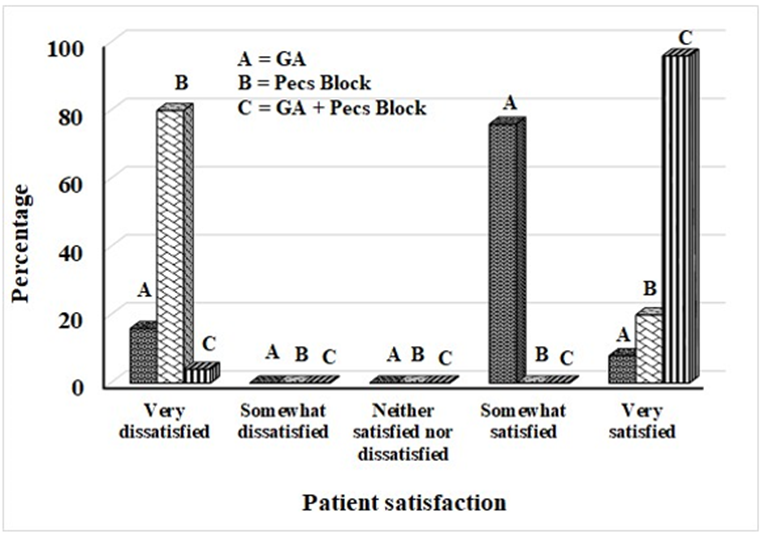
According to the type of analgesic requirements postoperative at baseline, the results showed that the PECS block group and the GA with PECS block group had a significantly higher percentage of patients who did not require any analgesic medication (84.0% and 80%, respectively) compared to 4% of the GA group (p lessthan 0.001). After 1 hour, and after 18 hours 96% of patients in the GA group required analgesic medication (Paracetamol), while none of the patients in the PECS block group and the GA with PECS block group required any analgesic medication. This difference was statistically significant (p lessthan 0.05). After 6 hours, 68% of patients in the GA group required analgesic medication (Ketorolac), while only 16% of patients in the PECS block group required analgesic medication (Ketorolac), and none of the patients in the GA with PECS block group required any analgesic medication. This mean that require to analgesic medication was significant increase in the GA group than the PECS block group and the GA with PECS block group. (P lessthan 0.05). After 12 hours, the GA group had a higher percentage of patients requiring analgesics compared to the other two groups. However, after 24 hours, there were no significant differences in analgesic requirements between any pair of groups. Based on Table 4 and Figure 3, the GA with PECS block group had the highest percentage of patients who reported being very satisfied, followed by the GA group and the PECS block group. This suggests that the GA with PECS block group may be associated with higher patient satisfaction.
Table 4: Comparison between the three studied groups regarding to patient satisfaction.
| GA (n=25) | PECS Block (n=25) | GA with PECS Block (n=25) | Test | P1 | P2 | P3 | P4 | ||||
| No | % | No | % | No | % | ||||||
| Patient Satisfaction | |||||||||||
| Very Dissatisfied | 4 | 16.0 | 20 | 80.0 | 1 | 4.0 | ◻2= 90.588 | lessthan 0.001* | MC lessthan 0.001* | MC lessthan 0.001* | lessthan 0.001* |
| Somewhat Dissatisfied | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||||
| Neither Satisfied or Dissatisfied | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||||
| Somewhat Satisfied | 19 | 76.0 | 0 | 0.0 | 0 | 0.0 | |||||
| Very Satisfied | 2 | 8.0 | 5 | 20.0 | 24 | 96.0 | |||||
◻2: Chi–Square, MC: Monte Carlo, P1: Comparing the three studied groups, P2: Comparing GA and PECS block, P3: Comparing GA and GA with PECS block, P4: Comparing PECS block and GA with PECS block, *: Significant when p lessthan 0.05.
Figure 3: Column chart for comparison between the three studied groups regarding to patient satisfaction.
Discussion
The surgical intervention known as mastectomy entails the extraction of breast tissue, and the effective management of pain following the procedure is of utmost importance in ensuring patient well-being and recuperation [10]. Regional anesthetic approaches, such as the pectoral nerve block (PECS block), have garnered significant interest as a potential approach to enhance postoperative pain management in individuals undergoing mastectomy, as highlighted by Karvandian et al. [11]. The PECS block is a form of localized anesthetic that effectively inhibits the neural pathways responsible for innervating the pectoralis major and pectoralis minor muscles. This technique can be employed to administer analgesia during surgical interventions or other operations that involve the aforementioned musculature. The experimental group in this study was administered general anesthesia, a form of anesthesia that induces a state of unconsciousness [12]. The administration of general anesthesia normally entails the utilization of a pharmacological amalgamation of sedative agents, analgesic substances, and neuromuscular blocking agents. The PECS block has the potential to mitigate systolic blood pressure (SBP) by the inhibition of stress hormone release and the induction of vasodilation, resulting in the widening of blood vessels. In the study conducted by Naghibi et al. [13], the group that had general anesthesia was also administered a PECS block.
The research encompassed a comparative analysis of three distinct cohorts that underwent varying treatment approaches: general anesthesia (GA) in isolation, the Pecs block as a standalone intervention, and the combined strategy using both GA and the Pecs block. Each group was comprised of 25 female participants. The study revealed that the mean age was comparable across the three groups, and no statistically significant disparity was detected. This finding indicates that age did not exert a substantial influence on the comparison of outcomes between the groups. Likewise, the average weight and average height exhibited identical values among the groups, with no statistically significant disparities seen.
According to the study cited in the provided information, it was seen that all 25 patients in each of the three groups underwent mastectomy, implying that there was uniformity in the surgical procedure across the groups. The ASA classification, a widely utilized tool for assessing patients' physical status before surgical procedures, was also utilized by the researchers [11]. The findings indicated that there was no statistically significant difference in ASA classification among the three groups. Previous research has investigated the influence of anesthetic strategies on the categorization and evaluation of risk in surgical procedures for breast cancer [11].
The present study investigated the impact of various anesthetic procedures on the provision of postoperative analgesia in individuals undergoing mastectomy. The findings revealed that a total of 25 patients in each group were administered midazolam as a premedication. Furthermore, there was no statistically significant disparity observed in the allocation of midazolam dosages among the three groups. This implies that the distribution of patients administered with 2 mg, 2.5 mg, and 3 mg of midazolam was comparable among the three groups. [14] conducted a study to examine the impact of the combination of Pecs block and general anesthesia on patients undergoing mastectomy. The findings of the study are consistent with our own data, suggesting that there was no statistically significant variation in the administration of midazolam doses among the different groups. [13] Examined the postoperative pain scores and morphine requirements of patients following elective lower abdomen surgery, comparing the effects of spinal anesthesia with general anesthesia. The researchers noted that the utilization of spinal anesthesia was correlated with decreased pain scores and diminished morphine needs in comparison to the use of general anesthesia. In a similar vein, the study conducted by De Cassai et al. [15] investigated the impact of a pectoral nerve block on the experience of postoperative pain subsequent to breast surgery. The findings of their investigation demonstrated that the group receiving a pectoral nerve block had significantly reduced levels of pain in comparison to the group receiving general anesthesia. Moreover, there was a substantial and statistically significant disparity in the number of analgesic requests made by the two groups.
Gerbershagen et al., [16] conducted a comprehensive prospective cohort research to assess postoperative pain in a substantial sample of over 50,000 patients belonging to 179 distinct surgery groups. The research underscored significant disparities in pain intensity among various surgical procedures. Although the precise numerical ranking of pain levels may not have held therapeutic importance, its purpose was to enable comparisons among different surgery groups. The study conducted by Chu et al. [12] aimed to examine the effects of a paravertebral block on the level of postoperative pain experienced by patients who underwent breast surgery. The findings of their research indicate that individuals who had a paravertebral block exhibited notably lower pain scores and decreased usage of opioids in comparison to those who solely underwent general anesthesia. Furthermore, the study conducted by Widmeyer et al. [17] investigated an innovative methodology for enhancing postoperative pain control and mitigating narcotic usage subsequent to hip arthroscopy. The study revealed that individuals who had a combined approach of general anesthesia and peripheral nerve block exhibited notably reduced pain scores in comparison to those who alone got general anesthesia. Zhang et al. [10] did a comprehensive review and meta-analysis that specifically examined the analgesic effectiveness and safety of the erector spinae plane block in the context of breast cancer surgery. The results of this study shown that the erector spinae plane block had a significant correlation with reduced pain levels in comparison to the utilization of general anesthesia in isolation.
There was no statistically significant difference observed between the mean pain score at 1 hour after surgery and the mean pain score at baseline in the group that had general anesthesia with pectoral nerve block. Nevertheless, the sensation of discomfort ceased throughout the alternate time intervals, and this alteration was deemed to possess statistical significance (p lessthan 0.05). These findings indicate that the PECS block shown efficacy in the initial postoperative period for pain reduction; however, its analgesic impact was not sustained beyond a duration of one hour. The findings indicate that the PECS block has the potential to be an effective method for immediate postoperative pain management. Sun et al [18] did a meta-analysis that shares similarities with the present study, as it encompassed the identical set of 13 randomized controlled trials (RCTs) involving a total of 940 patients. It also led to a reduction in opioid consumption during the surgical procedure itself, as well as a delay in the time at which the first request for analgesic medication was made. These findings provide more evidence to support the effectiveness of Pecs block in managing pain during breast cancer surgery. In their study, Yu et al. [19] examined the impact of Pecs II block on the recurrence of breast cancer following surgical intervention. A total of 526 patients diagnosed with breast cancer were randomly assigned to two distinct groups: one receiving general anesthesia alone, and the other receiving general anesthesia in combination with a Pecs II block. The findings of their study demonstrated a considerable reduction in remifentanil use during surgery as a result of the implementation of the Pecs II block. Nevertheless, the Pecs II block did not demonstrate any statistically significant impact on the overall survival (OS), recurrence-free survival (RFS), and distant recurrence-free survival (DRFS) of breast cancer patients following surgical resection. This finding indicates that the administration of Pecs II block did not have a significant effect on the long-term prognosis of individuals with breast cancer. However, it does provide potential benefits in terms of lowering opioid usage during surgical procedures.
The findings of the study indicated that the group receiving general anesthesia with pectoralis nerve blocks (PECS) demonstrated superior results in relation to postoperative nausea and vomiting (PONV), patient satisfaction, and time of discharge. The occurrence of postoperative nausea and vomiting (PONV) was shown to be notably reduced in the group that received general anesthesia (GA) with pectoral nerves (PECS) block, in comparison to the group that just received general anesthesia. In addition, it was seen that the group receiving general anesthesia with patient-controlled epidural analgesia (GA with PECS) exhibited a greater level of patient satisfaction. This was evidenced by a higher proportion of patients within this group expressing a state of being highly content with their pain management. Furthermore, it was shown that patients who received the GA with PECS block intervention experienced a reduced duration of stay in the post anesthesia care unit (PACU). In order to provide additional substantiation for these findings, an examination of the research conducted by Clairoux et al. [20] is warranted.
Conclusion
The present study aimed to examine the effects of regional anesthetic, specifically paravertebral blocks, on postoperative outcomes in patients undergoing breast cancer surgery. The findings indicated that individuals who got paravertebral blocks exhibited a reduced duration of hospital stay prior to being deemed ready for discharge, a lower occurrence of postoperative nausea and vomiting (PONV), and shorter stays in the post-anesthesia care unit (PACU) in comparison to those who received general anesthesia (GA). The results of this study are consistent with previous research indicating that the utilization of regional anesthetic methods, such as the pectoral nerves (PECS) block, may present certain benefits in comparison to general anesthesia alone. The results of this study indicate that the choice of anesthetic procedure may not significantly influence patient satisfaction. Nevertheless, it is crucial to acknowledge that the aforementioned investigation is a solitary study encompassing a comparatively limited number of participants. Additional investigation is required to validate these findings and gain a more comprehensive understanding of the variables that influence patient contentment with anesthesia.
Declarations
Funding
These authors declare that above-submitted work was not funded by any governmental or private funding source nor sup- ported by any financial projects.
Acknowledgments
A. M. M. and MS. designed the study and performed the experiments. In addition, both authors analyzed the data and write the manuscript.
Institutional Review Board Statement
The authors acknowledge University of Sousee/Faculty of Medicine ibn El Jazzar/Tunisia/Al-Manara University/College of Health and Medical Technology/Iraq.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Dewi I, Widianti AT, Fatmawati A, Wulandari S, Sarirudi TI. (2023). The Predictors Need for Complementary Interventions Using Mobile Application Technology in Women with Breast Cancer. Journal NERS. 18(2).
Publisher | Google Scholor - Deutschmann C, Singer CF, Gschwantler-Kaulich D, Pfeiler G, Leser C, et al. (2023). Residual Fibro Glandular Breast Tissue After Mastectomy is Associated with An Increased Risk of a Local Recurrence or A New Primary Breast Cancer. BMC Cancer. 23(1):1-10.
Publisher | Google Scholor - Mahiou K, Jankowski C, Vincent L, Costaz H, Padeano M-M, et al. (2024). Impact of Breast Surgical Procedure on Survival in BRCA Mutated Patients with Invasive Breast Cancer: Mastectomy Versus Conservative Treatment. Journal of Gynecology Obstetrics and Human Reproduction. 53(5):102760.
Publisher | Google Scholor - Erden S, Yurtseven Ş, Demir SG, Arslan S, Arslan UE, et al. (2022). Effects of Transcutaneous Electrical Nerve Stimulation on Mastectomy Pain, Patient Satisfaction, and Patient Outcomes. Journal of Peri Anesthesia Nursing. 37(4):485-492.
Publisher | Google Scholor - Rahman MT, Akter N, Alamgir Jalil Pramanik MSIM, Rahman MA, Saimun Nahar MSP. (2022). Postoperative Pain Management is Improved by Anesthesia-Based Pain Management. Sch J App Med Sci. 10:1604-1608.
Publisher | Google Scholor - Zhao J, Cai S, Zhang L, Rao Y, Kang X, (2022). Progress, Challenges, and Prospects of Research on the Effect of Gene Polymorphisms on Adverse Reactions to Opioids. Pain and Therapy. 11(2):395-409.
Publisher | Google Scholor - Wallace AB, Song S, Yeh P, Kim EA. (2023). The Effect of Pectoral Nerve Blocks on Opioid Use and Postoperative Pain in Masculinizing Mastectomy: A Randomized Controlled Trial. Plastic and Reconstructive Surgery.
Publisher | Google Scholor - Eskandr A, Mahmoud K, Kasemy Z, Mohamed K, Elhennawy T. (2022). A Comparative Study Between Ultrasound-Guided Thoracic Paravertebral Block, Pectoral Nerves Block, and Erector Spinae Block for Pain Management in Cancer Breast Surgeries. A Randomized Controlled Study. Spanish Journal of Anesthesiology and Resuscitation. 69(10):617-624.
Publisher | Google Scholor - Zhao Y, Jin W, Pan P, Feng S, Fu D, et al. (2022). Ultrasound-Guided Transversus Thoracic Muscle Plane-Pectoral Nerve Block for Postoperative Analgesia After Modified Radical Mastectomy: A Comparison with the Thoracic Paravertebral Nerve Block. Perioperative Medicine. 11(1):1-11.
Publisher | Google Scholor - Zhang Y, Liu T, Zhou Y, Yu Y, Chen G. (2021). Analgesic Efficacy and Safety of Erector Spinae Plane Block in Breast Cancer Surgery: A Systematic Review and Meta-Analysis. BMC Anesthesiology. 21(1):1-12.
Publisher | Google Scholor - Karvandian K, Zebardast J, Borra NZ. (2018). Risk Assessment and Anesthesia Classification in BREAST Cancer Surgery. Archives of Breast Cancer. 168-1672.
Publisher | Google Scholor - Chu L, Zhang X, Lu Y, Xie G, Song S, et al. (2019). Improved Analgesic Effect of Paravertebral Blocks Before and After Video-Assisted Thoracic Surgery: A Prospective, Double-Blinded, Randomized Controlled Trial. Pain Research and Management.
Publisher | Google Scholor - Naghibi K, Saryazdi H, Kashefi P, Rohani F. (2013). The Comparison of Spinal Anesthesia with General Anesthesia on the Postoperative Pain Scores and Analgesic Requirements After Elective Lower Abdominal Surgery: A Randomized, Double-Blinded Study. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences. 18(7):543.
Publisher | Google Scholor - Zhou X, Luo Y, Sun J. (2018). Modifying Efficacy of Pectoral Nerve Block Combined with General Anesthesia in Patients Undergoing Radical Mastectomy. Chinese Journal of Anesthesiology. 12:978-980.
Publisher | Google Scholor - De Cassai A, Bonanno C, Sandei L, Finozzi F, Carron M, et al. (2019). PECS II Block is Associated with Lower Incidence of Chronic Pain After Breast Surgery. The Korean Journal of Pain. 32(4):286- 291.
Publisher | Google Scholor - Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, et al. (2013). Pain Intensity on the First Day After Surgery: A Prospective Cohort Study Comparing 179 Surgical Procedures. Anesthesiology. 118(4):934-944.
Publisher | Google Scholor - Widmeyer JR, Satalich J, Protzuk O, Hampton H, Torre M, et al. (2023). A Novel Approach to Improving Post-Operative Pain and Minimizing Opioid Consumption After a Hip Arthroscopy. Orthopedic Reviews. 15.
Publisher | Google Scholor - Sun Q, Liu S, Wu H, Kang W, Dong S, et al. (2020). Clinical Analgesic Efficacy of Pectoral nerve Block in Patients Undergoing Breast Cancer Surgery: A Systematic Review and Meta-Analysis. Medicine. 99(14).
Publisher | Google Scholor - Yu L, Cui X, Song P, Li C, Zhao H, et al. (2022). Perioperative Pectoral Nerve Block Type II and Postoperative Recurrence in Breast Cancer: A Randomized Controlled Trial. BMC Surgery. 22(1):447.
Publisher | Google Scholor - Clairoux A, Soucy-Proulx M, Pretto F, Courgeon V, Caron-Goudreau M, et al. (2022). Interpandemic Regional Anesthesia as Practice: A Historical Cohort Study in Patients Undergoing Breast Cancer Surgery. Canadian Journal of Anesthesia. 69(4):485-493.
Publisher | Google Scholor