Research Article
Effect Of Crown-To-Implant Ratio of Short Implants on Peri-Implant Stress: A Finite Element Analysis
1Lectuar Department of Oral and Maxillofacial Surgery, Yerevan State Medical University after M. Heratsi, Armenia.
2Professor Ulster University, Birmingham, Belgium.
3Professor, Head of Dept. of Oral and Maxillofacial Surgery Yerevan State Medical University after M. Heratsi, Armenia.
*Corresponding Author: Gagik Hakobyan DMSC,Professor, Head of Dept. of Oral and Maxillofacial Surgery Yerevan State Medical University after M. Heratsi, Armenia.
Citation: Ghambaryan N, Bollen C, Hakobyan G. (2025). Effect of crown-to-implant ratio of short implants on peri-implant stress: A finite element analysis. Dentistry and Oral Health Care, Biores Scientia Publishers 4(2):1-8. DOI: 10.59657/2993-0863.brs.25.040
Copyright: © 2025 Gagik Hakobyan, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 14, 2024 | Accepted: February 20, 2025 | Published: March 22, 2025
Abstract
Aim: Objective of this study was to evaluate the distribution of bone tension around single implants with different crown/implant ratio (1:1, 1.25:1,1.5:1) according to the von Mises criterion.
Materials and Methods: Stress analysis was performed using In Vesalius 3.0, Rhinoceros 3D 4.0 software. Three 3D models of the mandibular segment of the bone block were developed:
model A, implant (6 mm) connected to a crown (6 mm), C/I - 1:1; model B, implant (6 mm), connected to the crown (7.5), C/I -1.25:1; model C, implant (6 mm) connected to a crown (9 mm), C/I -1.5:1. The applied forces were 100 N (axial). The clinical part of the study included 68 patients with 152 short implants restored using various crown/implant ratios (1:1, 1.25:1, 1.5:1). The results were evaluated: the cumulative frequency of implant engraftment, MBL changes around the implant, follow up for 5 years.
Results: Under axial load, the highest stresses were concentrated at the abutment/implant junctions, the highest stresses were 67.94 MPa C/I -1:1, 68.09 MPa C/I -1.25:1 and 68.24 MPa C/ I -1.5:1, respectively. The results of the current study, indicate the increase in crown height showed little difference in load at the crown/implant interface with crown/implant ratios of 1:1, 1.25:1 and 1.5:1 Short implants cumulative success of implantation after 5 years was 97.8% for group 1, 97.6% for group 2, and 97.3% for group 3. Patients were satisfied with the results of treatment.
Conclusions: Use of shorts implants for prosthetic rehabilitation can be considered favorable and well substantiated.
Keywords: short implant; crown/implant ratio; finite element analysis; von mises
Introduction
Factors that determine the success of implant osseointegration are: implant biocompatibility, implant surface and geometry, implant diameter and length [1-7]. For effective implantation, a sufficient amount of bone tissue is required. To restore the necessary amount of bone tissue, various labor-intensive multi-stage bone-reconstructive operations are used, including autogenous block, distraction method, nerve reposition; these operations are costly, require high professional skills and have a high risk of complications [8-15]. In order to avoid expensive and time-consuming multi-stage implantation-bone-reconstructive operations in such patients, it is advisable to use a one-stage surgical method using narrow diameter implants or short implants (5 to 6 mm) [16-19]. The use of short implants allows, prevents damage to anatomical structures, reduces time and shows high clinical efficiency [20-26].
Optimization of macro- and micro-design of short implants by increasing the implant surface, diameter will help to avoid potential risks and ensure long-term stability [27,28].
The height ratio (C/I) of short implants to the prosthesis structure placed on it can be a risk factor in terms of the distribution of biomechanical stresses associated with overload, and may increase the risk of complications [29]. Therefore, it is important to aim for a low C/I ratio, to avoid overstressing the bone. However, some authors argue that treatment with short implants is possible with a C/I ratio greater than 1:1 [30-32]. Predicting the long-term efficacy of short implants requires assessing the effect of length, diameter, and C/I ratio on biological complications [33-37]. Various in vivo methods have been used to predict the distribution of bone load around the implant, Finite Element Analysis (FEM) is the most successful calculation method, and can non-invasively depict the stress distribution in a structure [39-41]. In the scientific literature there are recommendations for a favorable C/I ratios ratio for natural teeth, but recommendations for C/I ratios by implantology have not been established, which may be helpful to determining the prognosis of dental implants. Objective this study was to evaluate the distribution of bone tension around single implants with different crown/implant ratios (1:1, 1.25:1, 1.5:1) according to the von Mises criterion.
Material and Methods
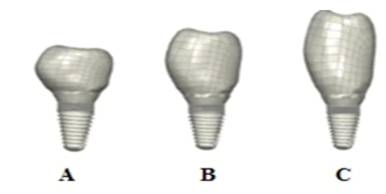
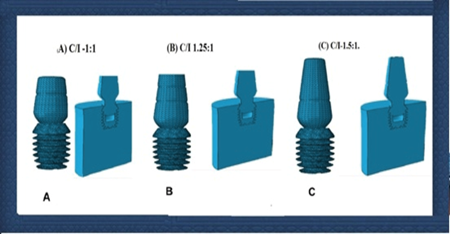
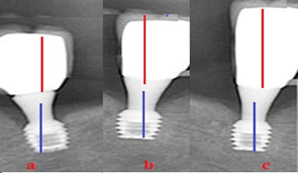
The experimental part of the study included modeling use FEM method. Stress analysis was performed using In Vesalius 3.0, Rhinoceros 3D 4.0 software. Three 3D models of the mandibular segment of the bone block were developed: (Figure 1, 2).
Figure 1: Models A, B and C resulting in a C/I ratio of 1/1, 1.25/1 and 1.5/1
Figure 2: Three-dimensional (3D) finite element modeling
model A, a short implant (6 mm) connected to a crown (6 mm), C/I - 1:1; model B, a short implant (6 mm), connected to the crown (7.5), C/I -1.25:1; model C, a short implant (6 mm) connected to a crown (9 mm), C/I -1.5:1.
The abutment and implant body were treated as a single unit, which prevented the potential effect of micromotion between the components. images of implants and abutments were reconstructed using CT pro 2.0 software (Metrics, Belgium). The bone model represented a mandibular bone block in the region of the second molar of quality type II bone in the center of the trabecular bone surrounding 1 mm of cortical bone. The surrounding bone around each implant was modeled as a cylinder 15 mm in diameter and 18 mm high. Bone block information was obtained using a CT database of implants and abutment geometries. After wards, modeling solids geometries have been exported to FEA pre- and post-processing software (FEMAP 11.2, Siemens PLM) to get the grids tetrahedral parabolic solid elements. 3D computer-aided design software (Solid Works 2010; USA) and Rhinoceros 4.0 CAD were used to calculate the Mises stress distribution. CAD software was used to define the mesh control of the 3D models. The color changes from yellow to blue, where blue represents the maximum stress value expressed in megapascals (MPa). The stress analysis was performed under the following conditions: the model contained an implant preloaded to 35 N, an abutment, and a cemented crown. An axial force of 100 N was applied to the occlusal surface of the crown. Bone density was modeled by changing the elastic modulus of tissue with elastic moduli of 13,7 GPa, the titanium implant component alloy with an elastic modulus of 112 GPa, and the superstructure feldspathic Ceramic of the model was designed as a restoration with an elastic modulus of 82,8 GPa.20. All materials modeled in this study are presented in Table 1.
Table 1: Mechanical properties of the simulated materials
| Simulated materials | Young Modulus (GA) | Poisson ratio (ν) |
| Trabecular bone tissue | 1.37 | 0.3 |
| Cortical bone tissue | 13.7 | 0.3 |
| Titanium (implant) | 112 | 0.35 |
| Cement | 22.4 | 0.35 |
| Feldspathic Ceramic | 87.8 | 0.35 |
68 patients with severe vertical bone atrophy in the masticatory region and the need for restoration with fixed implants prostheses were included in the clinical part of the study. The patients had 152 ultraviolet functionalization (UV) short implants (length 5-6 mm, diameters 4,5-5mm) and restored with different C/I crown/implant ratios (1:1, 1.25:1, and 1.5:1). The mean C/I ratio was 1.37. To clinical assessment the effect of C/I ratios of short implants and MBL there were formations of 3 groups. Group 1 included 48 short implants subjected to ultraviolet functionalization (UV) with a C/I ratio of 1:1. Group 2 included 51 short implants subjected to ultraviolet functionalization (UV) with a C/I ratio of 1,25:1. Group 3 included 53 short implants subjected to ultraviolet functionalization (UV) with a C/I ratio of 1.5:1. The results were evaluated: failures of the prosthesis and implant, any complications, implants marginal bone loss (MBL) the follow up for 5 years.
Statistical Analysis
Statistical analysis was performed using SPSS. P values <0>
Results
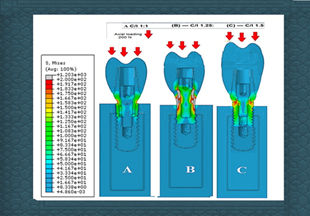
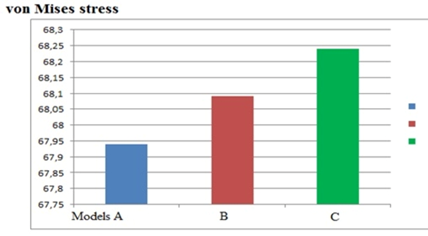
Under axial load, the highest stresses were concentrated at the abutment/implant junctions, the highest stresses were 67.94 MPa C/I -1:1, 68.09 MPa C/I -1.25:1 and 68.24 MPa C/ I -1.5:1, respectively (Figure 3).
Figure 3: von Mises stress distribution on implant/crown set — axial loading. (A) C/I -1:1 (B) C/I 1.25:1 (C) C/I-1.5:1 in type II bone with 100N axial load.
The increase in crown height showed little difference in load at the crown/implant interface with crown/implant ratios of 1:1, 1.25:1, and 1.5:1 respectively (Figure 4).
Figure 4: Model C showed little difference in load at the with crown/implant 1.5/1 ratios
During implant placement and in the follow up period, no serious biological or prosthetic complications were recorded. Аfter 1 years in Group 1 mean MBL 0.86±0.4 mm, after 3 years MBL was 0,98±0.2 mm, after 5 years MBL was 1.05±0.3 mm. After 1 years in Group 2 mean MBL 0.97±0.3 mm, after 3 years MBL was 1,07±0.4 mm, after 3 years MBL was 1.12 ±0.6 mm. Аfter 1 years in Group 3 mean MBL 1,08 ±0.6 mm, after 3 years MBL was 1,19±0.2 mm, after 5 years MBL was 1.27±0.3 mm (table 2).
Table 2: 3 GRUPS Implants marginal bone loss (MBL) after 1,3,5 year
| Group | mean MBL After 1 years | mean MBL After 3 years | mean MBL After 5 years | p-value⁎ |
| Group 1 | 0.86±0.4 mm, | 0,98±0.2 mm, | 1.05±0.3 mm. | <0> |
| Group 2 | 0.97±0.3 mm | 1,07±0.4 mm, | 1.12 ±0.6 mm | <0> |
| Group 3 | 1,08 ±0.6 mm | 1,19±0.2 mm | 1.27±0.3 mm. | <0> |
In CT observations in patients with different C/I ratio after 5 years of functional load, there were no significant differences in peri-implant marginal bone tissue (Figure 5).
Figure 5: CT in three models after 5 years functional load, no significant differences in the peri-implant marginal bone tissue were noted
He use of short implants for fixed-denture restoration in patients with edentulous and severe vertical bone atrophy in the posterior regions of the mandible has shown good results. Short implants cumulative success of implantation after 5 years was 97.8% for group 1, 97.6% for group 2, and 97.3% for group 3. Patients were satisfied with the results of treatment.
Discussion
Dental implants are widely used for prosthetic rehabilitation in patients with various forms of adentia.42 In recent years, short implants have become a predictable alternative for patients with vertical bone resorption (≤ 8 mm in length) [43-45]. Brown-to-implant ratio (C/I) is an important factor in successful oral restoration with short implants. Analysis of the occlusal load force at the bone-implant interface is important for the success or failure of an implant. One of the factors contributing to bone resorption around the implant body is overload which can lead to bone resorption and complications [46]. Various in vivo methods are used to assess bone stress around an implant. FEM is widely used to study biomechanics in various industries including mechanical engineering, civil engineering and aircraft industry [47]. Computerized Finite Element Analysis (FEM) is widely used in implantology to study the nature of the load on the bone around the implant and to predict the success of implantation in the clinical setting [48-50]. The results of Finite Element Analysis (FEM) by some authors indicate that the C/I ratio is not so important for the effective functioning of short implants and does not affect the loss of alveolar bone around the implant [51-53]. Tawil G et al in his research has shown that short implants are clinically successful regardless of the crown C/I ratio [54]. Schulte et al. compared the survival of single implants with different C/I crown-to-implant ratios and compared it to the crown-root ratio for natural teeth. The implant survival rate was 98.2% suggesting that the guideline used for natural teeth should not be applied to implant-supported restorations [55]. FEA computerized in vitro study, in which it is impossible to fully reproduce the clinical condition and should be supplemented with clinical assessment.
Long-term in vivo and in vitro studies are needed to objectively assess the effect of C/I ratio of short implants success. In this study, we performed a biomechanical test on short implant implants using 3D finite element analysis to elucidate the distribution of bone stresses around implants with crowns of different heights (crown/implant ratio 1:1, 1.25:1 and 1.5:1, respectively) according to the von Mises stress distribution. The area of bone around the implant was used to compare stress distribution across models. The crown/implant ratio (C/I) is an important factor in the successful restoration of the oral cavity with short implants. FEA is a computerized in vitro study in which it is impossible to fully reproduce the clinical condition. In this study, we performed a biomechanical test on short implants using 3D finite element analysis to elucidate the distribution of bone stresses around implants with crowns of different heights (crown/implant ratios 1:1, 1.25:1 and 1.5:1 respectively) according to the von Mises stress distribution. The bone area around the implant was used to compare stress distribution between models. Maximum underlying stress criteria have been used to evaluate cortical and trabecular bone (brittle materials), these criteria make it possible to distinguish between tensile and compressive stresses. The unit of measurement in this study was the megapascal (MPa). The results of the current study, are consistent with the results of our previous study results and indicate the increase in crown height showed little difference in load at the crown/implant interface with crown/implant ratios of 1:1, 1.25:1 and 1.5:1 respectively [56-59].
Conclusion
Study showed that short implanters are clinically successful regardless the C/I ratio. Use of shorts implants for prosthetic rehabilitation can be considered favorable and well substantiated.
Declarations
Competing Interest
The author declares that he has no competing Interest. None of the authors have relevant financial relations with a commercial interest.
Funding
The work was not funded.
Ethical Approval and Consent to participate
The study was reviewed and approved by University Ethical Committee (Approval number N12, Date 17.11.2021) and in accordance with those of the World Medical Association and the Helsinki Declaration.
Consent for publication
Patients were informed verbally and in writing about the study and gave written informed consent.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
- Cooper LF. (2000). A role for surface topography in creating and maintaining bone at titanium endosseous implants. J Prosthet Dent, 84:522-534.
Publisher | Google Scholor - Winkler S, Morris HF, Ochi S. (2000). Implant survival to 36 months as related to length and diameter. Ann Periodontol, 5:22-31.
Publisher | Google Scholor - Lee JH, Frias V, Lee KW, Wright RF. (2005). Effect of implant size and shape on implant success rates: a literature review. J Prosthet Dent, 94:377-381.
Publisher | Google Scholor - Renouard F, Nisand D. (2006). Impact of implant length and diameter on survival rates. Clin Oral Implants Res, 17:35-51.
Publisher | Google Scholor - Kotsovilis S, Fourmousis I, Karoussis IK, Bamia C. (2009). A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J Periodontol, 80:1700-1718.
Publisher | Google Scholor - Anitua E, Tapia R, Luzuriaga F, Orive G. (2010). Influence of implant length, diameter, and geometry on stress distribution: A finite element analysis. Int J Periodontics Restorative Dent, 30:88-95.
Publisher | Google Scholor - Kitamura E, Stegaroiu R, Nomura S, Miyakawa O. (2004). Biomechanical aspects of marginal bone resorption around osseointegrated implants: considerations based on a three-dimensional finite element analysis. Clin Oral Impl Res, 15:401-409
Publisher | Google Scholor - Dam VV, Trinh HA, Rokaya D, Trinh DH. (2002). Bone Augmentation for Implant Placement: Recent Advances. Int J Dent, 8900940.
Publisher | Google Scholor - Kumar, V.V., Ebenezer, S., Thor, A. (2021). Bone Augmentation Procedures in Implantology. In: Bonanthaya, K., Panneerselvam, E., Manuel, S., Kumar, V.V., Rai, A. ((eds) Oral and Maxillofacial Surgery for the Clinician. Springer, Singapore.
Publisher | Google Scholor - Kim YK, Ku JK. (2020). Ridge augmentation in implant dentistry. J Korean Assoc Oral Maxillofac Surg, 46(3):211-217.
Publisher | Google Scholor - Anitua E, Alkhraisat MH, Orive G. (2013). Novel technique for the treatment of the severely atrophied posterior mandible. Int J Oral Maxillofac Implants, 28(5):1338-46
Publisher | Google Scholor - Len Tolstunov. (2022). Essential Techniques of Alveolar Bone Augmentation in Implant Dentistry: A Surgical Manual.
Publisher | Google Scholor - Schaaf, H., Lendeckel, S., Howaldt, H. P., & Streckbein, P. (2010). Donor site morbidity after bone harvesting from the anterior iliac crest. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 109(1):52-58.
Publisher | Google Scholor - Li J, Wang HL. (2008). Common implant-related advanced bone grafting complications: classification, etiology, and management. Implant Dent, 17(4):389-401.
Publisher | Google Scholor - David Reininger, Carlos Cobo-Vázquez, Marta Monteserín-Matesanz, Juan López-Quiles. (2016). Complications in the use of the mandibular body, ramus and symphysis as donor sites in bone graft surgery. A systematic review Med Oral Patol Oral Cir Bucal, 21(2):241-249.
Publisher | Google Scholor - M. Saad, A. Assaf, E. Gerges. (2016). The Use of Narrow Diameter Implants in the Molar Area. International Journal of Dentistry.
Publisher | Google Scholor - Grant BT, Pancko FX, Kraut RA. (2009). Outcomes of placing short dental implants in the posterior mandible: a retrospective study of 124 cases. J Oral Maxillofac Surg, 67:713-717.
Publisher | Google Scholor - Jain N, Gulati M, Garg M, Pathak C. (2016). Short Implants: New Horizon in Implant Dentistry. J Clin Diagn Res, 10(9):ZE14-ZE17.
Publisher | Google Scholor - Antiua E, Escuer V, Alkhraisat MH. (2022). Short Narrow Dental Implants versus Long Narrow Dental Implants in Fixed Prostheses: A Prospective Clinical Study. Dent J (Basel), 10(3):39.
Publisher | Google Scholor - Romeo E, Bivio A, Mosca D, Scanferla M, Ghisolfi M, Storelli S. (2010). The use of short dental implants in clinical practice: literature review. Minerva Stomatol, 59(1-2):23-31.
Publisher | Google Scholor - Nedir, R.; Bischof, M.; Briaux, J.-M.; Beyer, S.; Szmukler-Moncler, S.; Bernard, J.-P. (2004). A 7-year life table analysis from a prospective study on ITI implants with special emphasis on the use of short implants. Clin. Oral Implants Res, 15:150-157.
Publisher | Google Scholor - Karthikeyan I, Desai SR, Singh R. (2012). Short implants: A systematic review. J Indian Soc Periodontol, 16(3):302-312.
Publisher | Google Scholor - Panos Papaspyridakos, Andre De Souza, Konstantinos Vazouras, Hadi Gholami, Sarah Pagni, Hans-Peter Weber. (2018). Survival rates of short dental implants (≤6 mm) compared with implants longer than 6 mm in posterior jaw areas: A meta-analysis Clin Oral Impl Res, 29(16):8-20.
Publisher | Google Scholor - Alysson-Henrique-Neves Ramos, G. M., Cornacchia, E. N., Mauricio-Greco Cosso, L. N. D., & Souza, E. G. Z. (2020). Extra short 4mm implants used to rehabilitation of atrophic posterior mandible. A serial case reports. Journal of Clinical and Experimental Dentistry, 12(5):519.
Publisher | Google Scholor - Anitua, E., Piñas, L., & Orive, G. Retrospective study of short and extra‐ short implants placed in posterior regions: influence of crown to implant ratio on marginal bone loss. Clinical implant dentistry and related research, 17(1):102-110.
Publisher | Google Scholor - Gürlek, Ö., Kaval, M. E., Buduneli, N. U. R. C. A. N., & Nizam, N. E. J. A. T. (2019). Extra‐ short implants in the prosthetic rehabilitation of the posterior maxilla. Australian dental journal, 64(4):353-358.
Publisher | Google Scholor - Silva R, Villalón P, Cáceres F. (2020). Effect of macro-design in the primary stability of short and extra-short implants using resonance frequency analysis. An ex vivo study. J Oral Biol Craniofac Res, 10(4):603-607.
Publisher | Google Scholor - Ravida A, Barootchi S, Askar H, Suarez-Lopez Del Amo F, Tavelli L, Wang HL. (2019). Long-term effectiveness of extra-short (≤6 mm) dental implants: a systematic review. Int J Oral Maxillofac Implants, 34:68-84.
Publisher | Google Scholor - Blanes RJ. (2009). To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin Oral Impl Res, 20:67-72.
Publisher | Google Scholor - Francesco G Mangano,Irene Frezzato,Alberto Frezzato,Giovanni Veronesi,Carmen Mortellaro,Carlo Mangano.(2016). The Effect of Crown-to-Implant Ratio on the Clinical Performance of Extra-Short Locking-Taper Implants. The Journal of craniofacial surgery, 27(3).
Publisher | Google Scholor - Schulte J, Flores AM, Weed M. (2007). Crown-to-implant ratios of single tooth implant supported restorations. J Prosthet Dent, 98:1-5.
Publisher | Google Scholor - Birdi H, Schulte J, Kovacs A, Weed M, Chuang SK. (2010). Crown-to-implant ratios of short-length implants. J Oral Implantol, 36(6):425-33.
Publisher | Google Scholor - Bulaqi HA, Mashhadi MM, Safari H, Samandari MM, Geramipanah F. (2015). Effect of increased crown height on stress distribution in short dental implant components and their surrounding bone: a finite element analysis. J Prosthet Dent, 113:548–557.
Publisher | Google Scholor - Andrea Torres-Alemany. (2020). Lucía Fernández-Estevan,* Rubén Agustín-Panadero, José María Montiel-Company, Carlos Labaig-Rueda, and José Félix Mañes-Ferrer.Clinical Behavior of Short Dental Implants: Systematic Review and Meta-Analysis. J Clin Med, 9(10):3271.
Publisher | Google Scholor - Tang, C., Du, Q., Luo, J. et al. (2022). Simultaneous placement of short implants (≤ 8 mm) versus standard length implants (≥ 10 mm) after sinus floor elevation in atrophic posterior maxillae: a systematic review and meta-analysis. Int J Implant, 8:45.
Publisher | Google Scholor - Chaware, Sachin Haribhau; Thakare, Vrushali; Chaudhary, Ritu; Jankar, Ajit; Thakkar, Smruti; Borse, Sidesh. (2021). The rehabilitation of posterior atrophic maxilla by using the graftless option of short implant versus conventional long implant with sinus graft.A systematic review and meta-analysis of randomized controlled clinical trial. The Journal of Indian Prosthodontic Society, 21(1):28-44.
Publisher | Google Scholor - Pinar Ercal1 & Aysegul Erten Taysi1 & Demet Cagil Ayvalioglu2 & Meltem Mert Eren3 & Soner Sismanoglu. (2021). Impact of peri-implant bone resorption, prosthetic materials, and crown to implant ratio on the stress distribution of short implants: a finite element analysis. Medical & Biological Engineering & Computing, 59:813-824.
Publisher | Google Scholor - Reddy MS, Sundram R, Eid Abdemagyd HA. (2019). Application of Finite Element Model in Implant Dentistry: A Systematic Review. J Pharm Bioallied Sci, 11(Suppl 2): S85-S91.
Publisher | Google Scholor - Reddy, M Sesha,Sundram, Rajasekar,Eid Abdemagyd (2019). Hossam Abdelatty. Application of Finite Element Model in Implant Dentistry.A Systematic Review. Journal of Pharmacy and Bioallied Sciences, 11(2):85-91.
Publisher | Google Scholor - Nour M.T. Ajaj AL-Kordy1 Mohannad H. (2020). AL-Saadi.Finite Element Study of Stress Distribution with Tooth-Supported Mandibular Overdenture Retained by Ball Attachments or Resilient Telescopic Crowns. European Journal of Dentistry.
Publisher | Google Scholor - Aldiéris Alves Pesqueira, et.al. (2014). Use of Stress Analysis Methods to Evaluate the Biomechanics of Oral Rehabilitation with Implants. J Oral Implantol, 40(2):217-228.
Publisher | Google Scholor - Albrektsson T, Donos N, Working Group 1. (2012). Implant survival and complications. The third EAO consensus conference 2012. Clin Oral Implants Res, 23(6):63- 65.
Publisher | Google Scholor - Esfahrood ZR, Ahmadi L, Karami E, Asghari S. (2017). Short dental implants in the posterior maxilla: a review of the literature. J Korean Assoc Oral Maxillofac Surg, 43(2):70-76.
Publisher | Google Scholor - Da Rosa T, de Souza P, Binhame Albini Martini M, Reis A-AL. (2018). Do short implants have similar survival rates compared to standard implants in posterior single crown? a systematic review and meta-analysis. Clin Implant Dent Relat Res, 20(5): 890-901.
Publisher | Google Scholor - Ravidà A, Wang IC, Barootchi S, et al. (2019). Meta-analysis of randomized clinical trials comparing clinical and patient-reported outcomes between extra-short (≤6 mm) and longer (≥10 mm) implants. J Clin Periodontol, 46(1):118-142.
Publisher | Google Scholor - Sadowsky SJ. Occlusal overload with dental implants: a review. Int J Implant Dent, 5(1):29.
Publisher | Google Scholor - Liu, W.K., Li, S. & Park, H.S. Eighty Years of the Finite Element Method: Birth, Evolution, and Future. Arch Compu tat Methods Eng, 29:4431-4453.
Publisher | Google Scholor - Moraes SL, Verri FR, Santiago Jr JF, Almeida DA, de Mello CC, Pellizzer EP. (2013). A 3-D finite element study of the influence of crown-implant ratio on stress distribution. Braz Dent J, 24:635-641.
Publisher | Google Scholor - Faria Almeida DA, Pellizzer EP, Verri FR, Santiago Jr JF, Carvalho PS. (2014). Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol, 85:261-269.
Publisher | Google Scholor - Araki H, Nakano T, Ono S, Yatani H. (2020). Three-dimensional finite element analysis of extra short implants focusing on implant designs and materials. Int J Implant Dent, 29;6(1):5.52.
Publisher | Google Scholor - Zupancic Cepic L, Frank M, Reisinger A, Pahr D, Zechner W, Schedle A. (2022). Biomechanical finite element analysis of short-implant-supported, 3-unit, fixed CAD/CAM prostheses in the posterior mandible. Int J Implant Dent, 8(1):8.
Publisher | Google Scholor - Blanes RJ, Bernard JP, Blanes ZM, Belser UC. (2007). A 10-year prospective study of ITI dental implants placed in the posterior region. II: Influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin Oral Implants Res, 18(6):707-714.
Publisher | Google Scholor - Tawil G, Aboujaoude N, Younan R. (2006). Influence of prosthetic parameters on the survival and complication rates of short implants. Int J Oral Maxillofac Implants, 21:275-82.
Publisher | Google Scholor - Schulte J, Flores AM, Weed M. (2007). Crown-to-implant ratios of single tooth implant supported restorations. J Prosthet Dent, 98:1-5.
Publisher | Google Scholor - Hakobyan G, Jilavyan A, Khachatryan G, Mathevosyan D, Tunyan G, Ghambaryan N. (2022). Evaluation of the survival rate of short implants placed in the posterior atrophic mandible: 5-year clinical study. Quintessence Int, 53(8):690-696.
Publisher | Google Scholor - Ghambaryan, N., Jilavyan, A., Burnazyan, S. et al. (2023). Clinical Outcome of Immediate Loading UV-Photofunctionalized Implants in Patients with Completely Edentulous Mandible, Placed with Guided Surgery. J. Maxillofac. Oral Surg, 1:64-75
Publisher | Google Scholor - Ghambaryan N. (2024). Impact of Dental Implant Surface UV-photofunctionalization on Osseointegration and Antibacterial Properties: Systematic Review. Bulletin of Stomatology and Maxillofacial Surgery, 20(2):152-160.
Publisher | Google Scholor - Ghambaryan, N., Yessayan, L. & Hakobyan, G. (2024). Long-term effectiveness of UV functionalised short (≤ 6 mm) dental implants placed in the posterior segments of the atrophied maxilla: controlled case series. Odontology, 112:1316-1325.
Publisher | Google Scholor