Case Report
EEG-based 3 Hz Intermittent Theta Burst Stimulation in a Middle-aged Female Resulted in Remission from Obsessive Compulsive Disorder
- Aswin K. Mudunuru *
Non-Invasive Brain Stimulation, Asha Neuromodulation Clinics, Hyderabad, India.
*Corresponding Author: Aswin K. Mudunuru, Non-Invasive Brain Stimulation, Asha Neuromodulation Clinics, Hyderabad, India.
Citation: Aswin K. Mudunuru. (2024). EEG-based 3 Hz Intermittent Theta Burst Stimulation in a Middle-aged Female Resulted in Remission from Obsessive Compulsive Disorder. Clinical Case Reports and Studies, BioRes Scientia Publishers. 6(2):1-7. DOI: 10.59657/2837-2565.brs.24.143
Copyright: © 2024 Aswin K. Mudunuru, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 23, 2024 | Accepted: June 20, 2024 | Published: June 28, 2024
Abstract
Obsessive Compulsive Disorder (OCD) is a chronic psychiatric illness associated with distress and emotional trauma. Non-Invasive Brain Stimulation (NIBS) is one of the adjuvant treatments for OCD along with pharmacotherapy. Repetitive transcranial magnetic stimulation (rTMS) is one of the NIBS methods that can be administered using planar figure of eight coil or an angular double cone coil or even a H coil. Treatment of OCD could be quite challenging in a few cases where all the standard available techniques fail to bring a desirable clinical response. In such cases, options like customization of treatment protocols or augmentation with intermittent theta burst stimulation (iTBS) or behavioral therapies could be explored. The present case report belongs to a middle-aged female patient diagnosed with OCD, on regular treatment for about 20 years. She presented with an exacerbation of obsessions and the consultant decided to start rTMS for her using deep rTMS with H7 coil. Interestingly, she fails to respond to the rTMS after about 45 sessions. EEG-based customization of treatment protocol was planned for her. Accordingly, 32-lead EEG has been obtained and frequency analysis of the prefrontal EEG has been performed. The standard iTBS protocol consisting of a train frequency of 5 Hz has been modified to 3 Hz. The pharmacotherapy has been maintained as usual. The patient dramatically responds to the new treatment in just about six sessions of iTBS. Her YBOCS dropped to 6 from the initial 38. The patient is followed up periodically after the customized treatment and has been found to be stable at 15 months follow-up also. Her YBOCS is still maintained at 6 and she is in remission.
Keywords: obsessive compulsive disorder; non-invasive brain stimulation; intermittent theta burst stimulation
Introduction
Obsessive compulsive disorder (OCD) is a chronic illness with waxing and waning course [1]. When the thoughts or actions are repetitive, irrational, involuntary, ego dystonic and which leads to distress, they must be clinically addressed and are termed as OCD. With its profuse and often bizarre clinical presentation, OCD is a severe debilitating mental disorder. Repetitive Transcranial Magnetic Stimulation (rTMS) in known to alleviate the symptoms of OCD given along with drugs and/or therapies [2]. The H7 coil is designed to produce deeper and broader neuronal stimulation in the dorsomedial prefrontal cortex and anterior cingulate cortex which is known to produce good clinical outcome [3]. The high frequency stimulation (HFS) at 20 Hz, the intermittent theta burst stimulation (iTBS) at 5 Hz – 50 Hz, low frequency stimulation (LFS) at 1 Hz are a few treatment protocols that can be safely employed in OCD. Despite these multiple non-invasive brain stimulation methods available, treatment of OCD remains a challenge in a few patients. We present in this case report, one such challenging case and an unusually unique response shown by this patient to a customized iTBS treatment protocol.
Case Presentation
Our patient was a 54-year-old female suffering from OCD for 22 years, and on regular treatment with SSRIs. She is suffering from miscellaneous obsessions (fear of saying certain thing's, fear of not saying just the right thing), somatic obsessions (concern with illness, salivation), inferiority complex (compared with others, like financial status and knowledge), feelings of guilt, lack of self-worth, doubt, and anxiety. She has a strong family history of psychiatric illnesses – her mother having OCD and maternal cousin ended his life with Schizophrenia. AV is also a known case of Bronchial Asthma since long with on and off treatment. She is not hypertensive, dysthyroid, or diabetic. She was on regular treatment with Fluvoxamine and Venlafaxine since about 20 years. She had a recent flare up of symptoms disabling her professional life for which she sought the medical advice. She was then advised to take deep rTMS sessions with H7 coil. A total of 45 dTMS sessions were given, 30 in the first cycle and 15 as maintenance sessions. Each session consisted of 50 20 Hz 2s 100% RMT trains with an interval of 20s, delivering 2000 pulses [4]. However, there was no significant reduction in YBOCS, and she relapsed within a month.
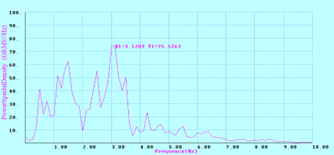
Eventually, it was planned to start intermittent theta burst stimulation for her with customization of frequency. The 32-channel Electroencephalogram (EEG) was obtained. Frequency analysis of bilateral prefrontal EEG using Fast Fourier Transform (FFT) graphs depicted a peak frequency around 3 Hz in the overall prefrontal region, in line with some previous studies [5]. A sample of the FFT graph is shown in Figure 1. The 3 Hz band was found to dominate all over the frontal areas. A customization was then made in the protocol replacing the 5 Hz train frequency with 3 Hz. Burst frequency was maintained at 50 Hz. The modified sessions began after a gap of 2 weeks (15 days). Each EEG-iTBS session now consisted of 600 pulses, which was given prior to the regular high frequency stimulation as a priming session. Just six such sessions were given. From session 3 onwards, patient reported a 50 percent fall in the severity of obsessions and the associated emotional pain. By 6th session, she complained a great relief in the symptoms and her emotional pain on VAS scored 2 from the previous 8. Her YBOCS reduced to 6 and she was extremely happy for the change.
Figure 1: The Fast Fourier Transform graph showing peak frequency around 3 Hz with maximal power spectral density. This is a representative graph from Fp2-F8 montage.
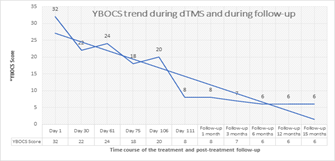
Although a greater number of sessions was planned, she could not attend the clinic due to workplace commitments. The patient has been followed up during 1, 3, 6, 12, and 15 months after the 6 iTBS sessions were completed [Figure 2]. She is doing comfortably well at her work and her current YBOCS is 6. Currently, she is on Fluoxamine 100 mg, Venlafaxine 37.5 mg, and Risperidone 3 mg + Trihexyphenidryl 2 mg and Clonazepam 0.25 mg daily.
Figure 2: The trend in YBOCS scores observed during dTMS and during the follow-up period up to 15 months
Discussion
The prefrontal quantitative EEG in OCD patients has been studied in detail by many authors in the past [5]. The authors in the present case scenario, wanted to explore the patient’s EEG and customize the treatment frequencies according to the predominant EEG frequency as obtained from quantitative analysis of the EEG. The standard iTBS treatment has a combination of train frequency of 5 Hz and burst frequency of 50 Hz. After the patient’s EEG has been analyzed, the 5 Hz train frequency was modified to 3 Hz. The burst frequency was maintained as 50 Hz. According to the new customized protocol, the patient received 540 pulses per session. 20 trains of 3 Hz frequency, ~3s duration and consisting of 9 triplet bursts were given with an interval of 8s at an intensity of 80%. We believe that this 3 Hz stimulation could somehow fall ‘in phase’ with the existing neuronal firing giving a maximal response from the neurons in the regions of dorsomedial prefrontal cortex and anterior cingulate cortex. The dramatic response shown by the patient in just six sessions and maintenance of remission thereafter for 15 months has really surprised the authors. WE propose that an elaborate neurophysiological and neuroimaging studies performed before administering the rTMS and the further customization of treatment in non-responders would improve the clinical outcomes in OCD patients.
Conclusion
The prefrontal quantitative EEG in OCD patients has been studied in detail by many authors in the past [5]. The authors in the present case scenario, wanted to explore the patient’s EEG and customize the treatment frequencies according to the predominant EEG frequency as obtained from quantitative analysis of the EEG. The standard iTBS treatment has a combination of train frequency of 5 Hz and burst frequency of 50 Hz. After the patient’s EEG has been analyzed, the 5 Hz train frequency was modified to 3 Hz. The burst frequency was maintained as 50 Hz. According to the new customized protocol, the patient received 540 pulses per session. 20 trains of 3 Hz frequency, ~3s duration and consisting of 9 triplet bursts were given with an interval of 8s at an intensity of 80%. We believe that this 3 Hz stimulation could somehow fall ‘in phase’ with the existing neuronal firing giving a maximal response from the neurons in the regions of dorsomedial prefrontal cortex and anterior cingulate cortex. The dramatic response shown by the patient in just six sessions and maintenance of remission thereafter for 15 months has really surprised the authors. WE propose that an elaborate neurophysiological and neuroimaging studies performed before administering the rTMS and the further customization of treatment in non-responders would improve the clinical outcomes in OCD patients.
References
- Chandran N, Parmar A, Deb KS. (2017). A Rare Presentation of a Case of Obsessive-compulsive Disorder Comorbid with Bipolar Affective Disorder. Indian J Psychol Med., 39(6):794-796.
Publisher | Google Scholor - Lusicic A, Schruers KR, Pallanti S, Castle DJ. (2018). Transcranial magnetic stimulation in the treatment of obsessive-compulsive disorder: current perspectives. Neuropsychiatr Dis Treat., 14:1721-1736.
Publisher | Google Scholor - Carmi L, Alyagon U, Barnea-Ygael N, Zohar J, Dar R, Zangen A. (2018). Clinical and electrophysiological outcomes of deep TMS over the medial prefrontal and anterior cingulate cortices in OCD patients. Brain Stimul. 11(1):158-165.
Publisher | Google Scholor - Carmi L, Tendler A, Bystritsky A, Hollander E, Blumberger DM. et al. Efficacy and Safety of Deep Transcranial Magnetic Stimulation for Obsessive-Compulsive Disorder: A Prospective Multicenter Randomized Double-Blind Placebo-Controlled Trial. Am J Psychiatry, 176(11):931-938.
Publisher | Google Scholor - Michael A. Kuskowski, Stephen M. Malone, Suck Won Kim, Maurice W. Dysken, Amy J. Okaya, et al. (1993). Quantitative EEG in obsessive-compulsive disorder. Biological Psychiatry, 33(6):423-430.
Publisher | Google Scholor