Review Article
Do we Properly Select Patients with High Risk of Preterm Delivery for Antenatal Corticosteroids Administration?
- Katarzyna Zając *
- Katarzyna Sobczuk
- Agata Pliszka
- Marta Karolczyk
- Jarosław Kalinka
Department of Perinatology, Medical University of Lodz, Poland.
*Corresponding Author: Katarzyna Zając, Department of Perinatology, Medical University of Lodz, Poland.
Citation: Zając K, Sobczuk K, Pliszka A, Karolczyk M, Kalinka J. (2024). Do we Properly Select Patients with High Risk of Preterm Delivery for Antenatal Corticosteroids Administration, Journal of Women Health Care and Gynecology, BioRes Scientia Publishers, 3(1):1-6, DOI: 10.59657/2993-0871.brs.24.024
Copyright: © 2024 Katarzyna Zając, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 07, 2023 | Accepted: December 27, 2023 | Published: January 03, 2024
Abstract
Background: Preterm delivery is still one of the main causes of neonatal morbidity and mortality. Timely implementation of antenatal corticosteroids (ACS) for patients at high-risk of preterm delivery reduces the risk of prematurity complications. The greatest benefits are observed within 7-14 days from the ACS administration. However, implementation of corticosteroids to a patient who does not deliver within this period could be associated with numerous negative consequences for the mother and fetus. The aim of the study was to estimate whether pregnant women were properly qualified for ACS treatment, defined as the proportion of women which delivered prematurely within 7 and 14 days from administration.
Methods: A retrospective study conducted at the Department of Perinatology of Medical University of Lodz Poland. The study analysed 146 cases of ACS administration among patients in the period from January 2021 to July 2022. Data was reviewed in terms of comorbidities, obstetric history, indications for ACS, administration of tocolytics, cervical pessary or cerclage application, vaginal progesterone intake and time from administration of steroids to delivery as well as selected neonatal outcomes.
Results: Only 31,5% of patients delivered within 7 days and 35,6% within 14 days from ACS administration. The main indication for ACS administration was risk of premature delivery (uterine contractions) (47,2%), short cervical length (25,3%) and preterm premature rupture of membranes (13%). Although, if we analyse the group that delivered within 14 days from corticosteroids treatment it includes: 18 out of 19 women diagnosed with pPROM (94,7%), 21 out of 69 patients with risk of premature delivery (30%), and 5 out of 37 patients where indication was short cervical length (13%).
Conclusions: The majority of patients after ACS intake do not deliver in the optimal period from the administration of treatment. Before implementing ACS, it is necessary to select patients with a real risk of premature delivery.
Keywords: antenatal corticosteroids; premature delivery; indications for ACS
Introduction
Preterm delivery (PTD) is still one of the main causes of neonatal morbidity and mortality around the world. Timely implementation of antenatal corticosteroids (ACS) for patients at high-risk of preterm delivery reduces the chance of prematurity complications for new-born [1]. The greatest benefits of antenatal corticosteroids are observed within 7 days from the drug administration [2]. However, implementation of corticosteroids to a patient who does not deliver within this period could be associated with numerous consequences for the mother and fetus. From the fetus perspective most important long-term complications of antenatal corticosteroids intake may be reduced brain development, higher blood pressure in adolescence, as well as some mental and behavioural disorders [3, 4]. That is why proper identification of PTD symptoms and proper implementation of antenatal corticosteroids is crucial for future proper development of a child. The aim of the study was to estimate whether pregnant women were properly qualified for ACS treatment, defined as the proportion of women that delivered prematurely within 7(optimal time) to 14 (suboptimal time) days from administration.
Materials and Methods
This study analyses the medical history of 146 patients who underwent antenatal corticosteroids treatment between January 2021 and July 2022 in the Department of Perinatology of Medical University of Lodz (Poland). Electronic and paper documentation of mothers and new-borns were used to obtain data. In case of maternal status age, gestational age, parity, comorbidity and history of previous and current pregnancies was analysed. Antenatal corticosteroids administration was reviewed in terms of week of implementation, number of doses and courses of corticosteroids. Time between steroids administration and delivery was assessed as well as early neonatal outcomes (birth weight, APGAR score). Each parameter was calculated and analysed from data collected from the hospital register. Data was collected and reviewed using Microsoft Excel Office.
Results
Age of analysed mothers ranged between 17 and 44 years with an average of 30-31 years old. Exact age distribution is presented in Table 1.
Table 1: Patients Age Distribution.
| Age in years | Number of Patient (Percent) |
| <=19 | 4 (2,7%) |
| 20-25 | 11 (7,5%) |
| 26-30 | 41 (28,1%) |
| 31-35 | 61 (41,8%) |
| 35-40 | 25 (17,1) |
| >40 | 4 (2,7) |
Paritary status of mothers who were qualified to antenatal corticosteroids presented accordingly - 51 (34,9%) primigravidas and 95 (65,1%) multigravidas. Analysed group includes 7 twin pregnancies. In the study group 20 of the patients had a history of preterm delivery. Among patients several other comorbidities were found as presented in Table 2.
Table 2: Comorbidities within Study Group.
| Comorbidity | Number of women (Percentage) | Number of women with comorbidity that delivered within 7 days from ACS | Number of women with comorbidity that delivered within 7-14 days from ACS | Number of women with comorbidity that delivered prematurely |
| History of preterm delivery | 20 (13,7%) | 3 | 0 | 4 |
| Diabetes | 22 (15,1%) | 2 | 0 | 5 |
| Obesity (Defined as BMI>=30) | 24 (16,4%) | 8 | 0 | 13 |
| Hypertension | 23 (15,8%) | 11 | 1 | 18 |
| Nicotinism | 9 (6,2%) | 2 | 1 | 6 |
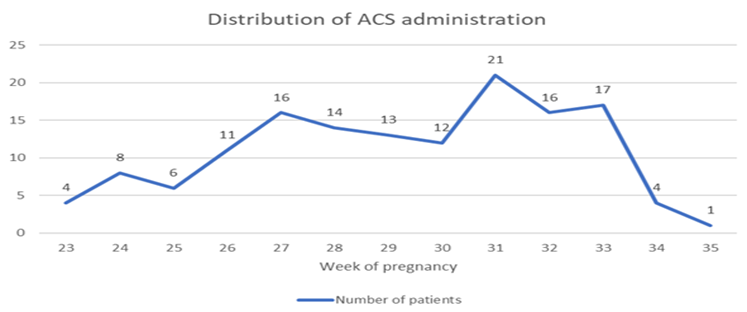
Patients received antenatal corticosteroids between 23th and 34th week of pregnancy. One of the patients after consultation with the neonatology team received treatment in the 35th week of pregnancy. In the analysed group 3 patients received two full courses of antenatal corticosteroids. In 15 cases full courses of antenatal corticosteroids were given before patients were transferred to our department and in 2 cases ACS were continued in our department after the first dose received outside. Distribution of ACS administration among patients in particular weeks of pregnancy is presented in the Graph 1. Three of patients that received multiple courses were excluded.
Graph 1: Distribution of gestational age at ACS administration.
Course of ACS (two doses of Betamethasone 12 mg i.m) was completed in 133 cases. 10 patients received only one course because of premature delivery, and 1 patient was discharged from hospital after 1st dose on her request. Data of 2 patients who received steroids outside our hospital are ambiguous. Outside antenatal corticosteroids other treatments were provided to prevent premature delivery and are presented in Table 3.
Tabel 3: Treatments Implemented to Prevent Preterm Delivery
| Treatments implemented to prevent preterm delivery | Number of patients (Percentage) |
| Atosiban | 57 (39,0%) |
| Progesterone supplementation | 96 (65,8%) |
| Magnesium sulfate | 62 (42,5%) |
| Cervical pessary | 33 (22,6%) |
| Cervical cerclage | 6 (4,1%) |
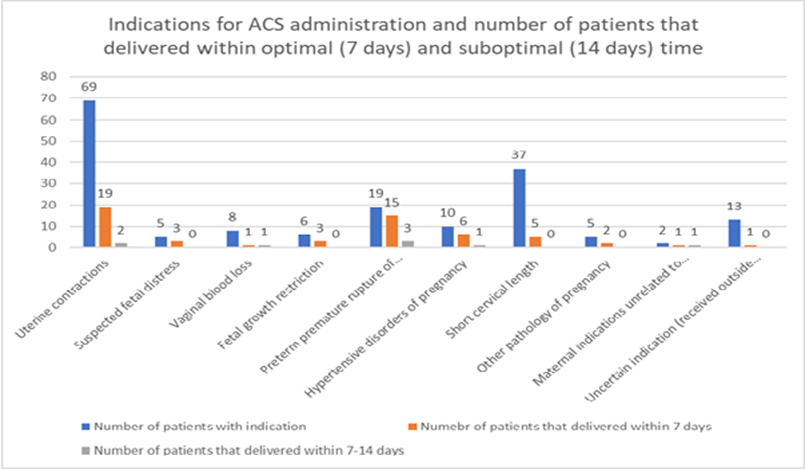
The main indications for antenatal corticosteroids treatment was high risk of preterm delivery (defined as uterine contractions) (n = 69; 47,2%), short cervical length (n=37; 25,3%) and preterm premature rupture of membranes (n=19; 13%). Other indications are presented in Table 4. Some patients presented several indications for ACS administration.
Table 4: Indications for ACS administration.
| Indications for ACS administration | Number of patients (percentage) |
| Uterine contractions | 69 (47,3%) |
| Suspected fetal distress | 5 (3,4%) |
| Vaginal bleeding | 8 (5,5%) |
| Fetal growth restriction (FGR) | 6 (4,1%) |
| Preterm premature rupture of membranes | 19 (13,0%) |
| Hypertensive disorders of pregnancy | 10 (6,8%) |
| Short cervical length | 37 (25,3%) |
| Other pathology of pregnancy (ex. cholestasis of pregnancy, twin pregnancy) | 5 (3,4%) |
| Maternal indications unrelated to pregnancy | 2 (1,4%) |
| Not known indication (received outside our department) | 13 (8,9%) |
In the analyzed group 46 (31,5 %) of patients delivered prematurely within 7 days from the antenatal corticosteroids course and 52 (35,6%) delivered within 14 days. Group that delivered within 14 days from corticosteroids treatment includes: 18 out of 19 women diagnosed with pPROM (94,7%), 21 out of 69 patients with risk of premature delivery (30%), and 5 out of 37 patients where indication was short cervical length (13%). A comparison of indications for ACS administration and delivery within 7 and 14 days from treatment is presented in Graph 2.
Graph 2: Treatments implemented to prevent preterm delivery.
In further analysis of deliveries 72 out of 146 (49,3%) patients gave birth prematurely (before 37 weeks of pregnancy) and 48 (32,9%) delivered after 37 weeks. Among analyzed births 77 (52,7%) were delivered via cesarean section, 37 (25,3%) vaginally and 4 (2,7%) by forceps delivery. Data of deliveries of 26 (17,8%) women who were discharged from the hospital after receiving treatment are unknown. All newborns that were delivered in our hospital (including 7 twins) were assessed using Apgar score after 1st and 10th minute of life. 75 of the newborns were born in general good condition and received Apgar score >7 after 1st minute. Apgar score between 7-4 was given to 49 of infants. Only 3 newborns received Apgar score after 1st minute less than 4 points. Exam after 10th minute presented accordingly, 106 newborns received Apgar score >7 points, 19 of them received 4-7 points and none of the newborns was assessed after 10 min as in general bad condition (Apgar less than 4 points).
Discussion
Preterm delivery is still to this day one of the main problems of modern obstetrics since it’s associated with a high amount of neonatal morbidity and mortality. As study showed - timely administration of antenatal corticosteroids treatment can reduce many complications of prematurity, such as respiratory distress syndrome, intracranial haemorrhage, necrotizing enterocolitis and perinatal death and others [1]. Greatest benefits of ACS treatment are shown within 7 days after full course administration. However even a single dose of corticosteroids may improve neonatal outcomes [2]. On the other hand, implementation of antenatal corticosteroids to a patient who does not deliver within an optimal period from treatment is associated with many negative consequences for new-born such as neurodevelopmental issues, mental and behavioural disorders, reduced brain growth and higher diastolic pressure and type 2 diabetes in adolescence and many more [3,4].
In our analysis optimal timing of ACS (within 7 days from administration) was reported in 46 cases (31,5 %). 6 (4,1%) women gave birth in suboptimal time from corticosteroids administration (7-14 days). In total we received results of 52 (35,6%) cases of delivery within 14 days from ACS intake. In comparison, in study done by HI Levin [5]. ACS was given in optimal time (up to 7 days before birth) in 238 cases (40,4%) and study done by Jolande 143 [6] (41%) delivered within 7 days from the complete course. A study conducted in Germany showed that only 25/120 women (20.8%) delivered within the optimal time window of 1–7 days after antenatal steroid application. 5/120 women (4.2%) only received one dose of antenatal steroids before birth and 3/120 (2.5%) gave birth within 8 to 14 days after antenatal steroids. Most women gave birth more than 14 days after steroid application (72.5%, 87/120) [7]. In comparison, Smith et al. study resulted in 401 (31.8%) and 569 women (45.1%) that received ACS within ≤ 7 days and ≤ 14 days before birth, respectively, and 203 (16.1%) ultimately gave birth at term [8]. The most common indications for antenatal corticosteroids in our study were high risk of preterm delivery (uterine contractions) (n= 69, 47,2%), short cervical length (n=37, 25,3%) and preterm premature rupture of membranes (n=19, 13%). This result differs from analyzed group obtain by HI Levin [5] where results of most common indications present as follows: hypertensive disorders of pregnancy (n=145, 24,6%), uterine contractions (n=132, 22,4%) and preterm premature rupture of membranes (n=130, 22,1%). Preeclampsia as an indication with the highest results of preterm delivery within optimal time from administration was also presented in Humbeck’s study [7].
If we compare group of indications for antenatal corticosteroids and patients who actually delivered within 7 and 14 days from administration the most reliable (outside of planned premature delivery) were: preterm premature rupture of membranes (7 days: 15 out of 19; 78,9%; 14 days: 18 out of 19 patients; 94,7%), hypertensive disorders of pregnancy (7 days: 6 out of 10; 60 %; 14 days: 7 out of 10; 70%) and suspected fetal distress (7 days: 3 out of 5; 60%; 14 days: 3 out of 5; 60%). Other indications showed efficacy in equal or less than 50% of cases. Outcomes of this comparison in a study done by HI Levin [5] presented only one induction with efficiency higher than 50% - hypertensive disorder in pregnancy (62,1%), the second most efficient indication was preterm premature rupture of membranes (46,2%). Study conducted by Smith [8] showed the proportion of women who received ACS within 7 days before birth was highest for women with preeclampsia (50.4%), and was lowest for women with an incidental finding of a short cervix (8.4%). On the other hand, in a study done by the Jolande [6] group of women with multiple indications was excluded and delivered within 7 days in 58
Conclusion
Our observational data indicate that most pregnant women do not give birth within optimal time from administration of antenatal steroids.
Before implementing antenatal corticosteroids, it is necessary to select patients with a real risk of premature delivery.
To better determinant patients’ group with risk of PTD within 7 days from ACS administration it is worth using additional tools for selection.
References
- McGoldrick E, Stewart F, Parker R, et al. (2020). Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev, 12.
Publisher | Google Scholor - George Daskalakis, Vasilios Pergialiotis, Magnus Domellöf, Harald Ehrhardt, Gian Carlo Di Renzo, Esin Koç, Ariadne Malamitsi-Puchner, Marian Kacerovsky, Neena Modi, Andrew Shennan, Diogo Ayres-de-Campos, Elko Gliozheni, Kristiina Rull, Thorsten Braun, Artur Beke, Katarzyna Kosińska-Kaczyńska, Ana Luisa Areia, Simona Vladareanu, Tanja Premru Sršen, Thomas Schmitz & Bo Jacobsson (2023) European guidelines on perinatal care: corticosteroids for women at risk of preterm birth. The Journal of Maternal-Fetal & Neonatal Medicine.
Publisher | Google Scholor - Melamed N, Asztalos E, Murphy K, et al. (2019). Neurodevelopmental disorders among term infants exposed to antenatal corticosteroids during pregnancy: a population-based study. BMJ Open, 9(9):031197
Publisher | Google Scholor - Asztalos E. (2012). Antenatal corticosteroids: a risk factor for the development of chronic disease. J Nutr Metab, 930591.
Publisher | Google Scholor - Levin HI, Ananth CV, Benjamin-Boamah C, et al. (2016). Clinical indication and timing of antenatal corticosteroid administration at a single Centre. BJOG, 123(3):409-414.
Publisher | Google Scholor - Jolande Y Vis 1, Femke F Wilms, Rosanna A Kuin, Janine M Reuvers, Monique C Stam, Desiree A P M Pattinaja, Ben Willem J Mol. (2011). Time to delivery after the first course of antenatal corticosteroids: a cohort study. Am J Perinatol, 28(9):683-688.
Publisher | Google Scholor - Humbeck, C., Jonassen, S., Bringewatt, A. et al. (2022). Timing of antenatal steroid administration for imminent preterm birth: results of a prospective observational study in Germany. Arch Gynecol Obstet.
Publisher | Google Scholor - Smith, J., Murphy, K.E., McDonald, S.D. et al. (2022). Timing of antenatal corticosteroids in relation to clinical indication. Arch Gynecol Obstet, 306:997-1005
Publisher | Google Scholor - Moeun Son, , Emily S. Miller. (2017). Predicting preterm birth: Cervical length and fetal fibronectin. Semin Perinatol. 41(8):445-451.
Publisher | Google Scholor - Çekmez et al. (2017). Use of cervicovaginal PAMG-1 protein as a predictor of delivery within seven days in pregnancies at risk of premature birth. BMC Pregnancy and Childbirth, 17:246.
Publisher | Google Scholor - Nikolova T, Bayev O, Nikolova N, et al. (2014). Evaluation of a novel placental alpha microglobulin-1 (PAMG-1) test to predict spontaneous preterm delivery. J Perinat Med, 42(4):473-477.
Publisher | Google Scholor - Lee SMi, Romero R, Park JW, et al. (2012). The clinical significance of a positive Amnisure test in women with preterm labor and intact membranes. J Matern Fetal Neonatal Med, 25(9):1690-1698.
Publisher | Google Scholor