Research Article
Direct Anterior Versus Posterior Approach for Total Hip Arthroplasty: Systematic Review with Meta-analysis
- Bianca Gabriella de Oliveira 1*
- Fernando Cesar Padula Silva 2
- Mateus Dias Ribeiro 2
- Renan Rodrigues Rezende 2
- Gustavo da Silva Bataglia 2
- Melissa Alves Aires Marques 3
1.Medical student at the University of Salvador-UNIFACS, Salvador, BA, Brazil.
2.Resident in Orthopedics and Traumatology Mario Gatti Municipal Hospital, Brazil.
3.Medical student at the University of Iguaçu, Itaperuna, RJ, Brazil.
*Corresponding Author: Bianca Gabriella de Oliveira, Medical student at the University of Salvador-UNIFACS, Salvador, BA, Brazil.
Citation: Bianca G. Oliveira, F.C.P. Silva, Mateus D. Ribeiro, Renan R. Rezende, Gustavo S. Bataglia, et al. (2024). Direct Anterior Versus Posterior Approach for Total Hip Arthroplasty: Systematic Review with Meta-analysis. Journal of Clinical Rheumatology and Arthritis, BioRes Scientia Publishers. 2(1):1-7. DOI: 10.59657/2993-6977.brs.24.011
Copyright: © 2024 Bianca Gabriella De Oliveira, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 26, 2024 | Accepted: March 14, 2024 | Published: March 21, 2024
Abstract
Objectives: To evaluate the efficacy of the direct anterior approach (DAA) versus the posterior approach (AP) for total hip arthroplasty.
Materials and methods: Systematic review with meta-analysis performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria. A search was carried out in the databases (PubMed, OVID Medline, EMBASE) from the start date of the database until February 1, 2024.
Results : 689 patients were included, 352 underwent the procedure via the posterior approach and 337 via the direct anterior approach. The direct anterior approach (DAA) was related to better functional recovery with a slightly better Harris Hip Score (HHS) when compared to the posterior approach (AP). There were no significant differences in the pain scales between the groups.
Conclusion : The DAA has better early functional results, as well as shorter hospital stays, fewer complaints of pain and soft tissue injury, but it requires more operative time and blood loss than the PA, with the orthopaedic surgeon needing a prolonged curve to avoid possible complications.
Keywords: total hip arthroplasty; femoral head; orthopaedic procedures
Introduction
The orthopaedic implant known as total hip arthroplasty (THA) originated in 1981 in Germany by Glück, who presented the use of ivory as a possibility for replacing the femoral heads of patients with hip joint involvement due to tuberculosis. Over the years, the material used evolved until, in 1960, Sir John Charnley created the low-friction arthroplasty used today [1]. This is an anatomical replacement of the femoral head and acetabular component through a successful, safe surgery, defined as a satisfactory surgical intervention in the functional recovery of patients with some degree of impairment in the locomotor system, with a 10-year survival rate of over 95% [2,3,4]. Hip joint involvement resulting in surgical treatment with THA (partial or total) includes proximal femur fractures, congenital deformities and coxarthrosis [5,6,]. Since it is a sphenoid diarthrosis lined with hyaline cartilage, the bone surfaces are protected for proper joint sliding. It enables the functions of support, body weight support and load transmission from the axial skeleton to the appendicular skeleton, so when it is affected by any of the pathologies mentioned above, it causes a pain crisis and functional impairment [7].
Hip osteoarthritis, or coxarthrosis, has a high prevalence - around 500 million people worldwide. It is an osteodegenerative disease that causes destruction of the joint component and compromises biomechanics, causing pain, joint stiffness, muscle dysfunction, delayed or impaired gait, which can progress to functional limitation and even disability of the hip joint [8,9]. The therapeutic choice takes into account the patient's complaint, the anatomical impairment and the physical examination, usually associating and including motor physiotherapy, postural rehabilitation and total or partial hip arthroplasty [4,5]. Therefore, from a scientific point of view, there are various approaches to surgery, such as: posterior (AP), lateral (AE) and the right anterior approach (DAA). Discussing the best access is essential for planning the operation and all of them have advantages and disadvantages. The AP approach divides the gluteus maximus for a better posterior joint image, provides excellent visualization of the acetabulum and femur, and consequently avoids rupture of the hip abductor muscles, although it has an increased risk of dislocation of the implanted prosthesis [8,9].
The lateral incision is made by dividing the gluteus medius for better anterolateral visualization, with a lower risk of dislocation, but the possibility of injury to the superior gluteal nerve, heterotopic ossification and adductor injury. Thus, the DAA is the incisional plane with internervous and intermuscular topography, between the sartorius muscle and the tensor fascia lata, with a lower risk of dislocation, less likelihood of gluteal nerve injury but significant for the lateral femoral cutaneous nerve and periprosthetic fractures [8,9,10,11]. Therefore, this study aims to evaluate the effectiveness of the direct anterior approach (DAA) versus the posterior approach (AP) for total hip arthroplasty by means of a systematic review and meta-analysis showing level 1 evidence by comparing functional results, preoperative parameters and complications.
Materials and Methods
Systematic review with meta-analysis based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria. A search was carried out in the databases (PubMed, OVID Medline, EMBASE) from the database start date until February 1, 2024. The Medical Subject Headings and Boolean operators used were: "Total hip arthroplasty" OR "Total hip replacement". The articles included in the studies were all randomized clinical trials and retrospective studies that directly compared the results of AAD versus AL or AP in THA. Non-English language studies, non-peer-reviewed studies, conference abstracts, unpublished manuscripts and studies that did not directly compare outcomes between THA approaches were excluded. Studies were selected by two independent authors and irrelevant studies were excluded. Differences of opinion were resolved by discussion between the first two authors. The quality of the methodology of the included studies was assessed using the Cochrane Collaboration tool for Risk of Bias (RoB) in RCTs. Seven criteria were used to analyze the RCT. The criterion is classified as "low risk" if the criterion is fully respected, "high risk" if it is not respected and "unclear risk" if the criterion is not mentioned. Any discrepancy in the risk assessment was resolved by open discussion and the decisive vote of a third reviewer.
Results
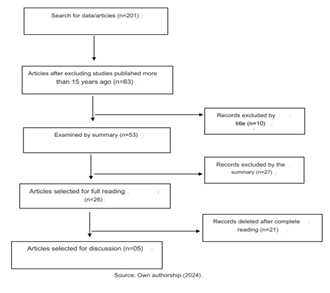
The study began by selecting 201 articles, of which 138 were excluded because they had been published more than 15 years ago, leaving 63. After analyzing the title and abstract, 37 were excluded because they did not correspond to the purpose of the study, leaving 26 for full reading. Finally, 5 articles were selected for analysis, discussion and construction of the article (Figure 1).
Figure 1: Studies selected according to PRISMA parameters.
The 05 articles selected correspond to patients undergoing total hip arthroplasty using the direct anterior approach (DAA) or posterior approach (AP). A functional assessment of the post-surgical hip was carried out using the Harris Hip Score (HHS), as well as the length of hospital stay, VAS analog scale and complications. A total of 689 patients were included. 352 underwent the procedure via the posterior approach and 337 via the direct anterior approach.
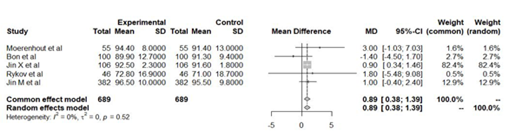
Table 1 shows the selected studies and their results (Table 1) [17,18,19,20,21]. Table 2 shows the Harris Hip Score (HHS) of patients who underwent total hip arthroplasty via the right anterior or posterior approach [17,18,19,20,21]. Figure 2 shows the analysis of the functional hip assessment of patients undergoing total hip arthroplasty [17,18,19,20,21].
Table 1: Selected works and their results.
| Study | Approach | F/M patients | Result |
| Moerenhout e col | Direct Anterior (DAA) posterior (AP) | 26/29 | Length of hospital stay surgical time; complications; Harris hip score (HHS); visual an along (VAS). |
| its good,col | Direct Anterior (DAA) posterior (AP) | 56/44 | Charnley and Harris Score (HHS); Postel- Merle-d'Aubigné and Oxford-12 scores; locomotor assessment; length of hospital stay. |
| jinX et al | Direct Anterior (DAA) posterior (AP) | 61/45 | length of hospital stays, visual analogue scale (VAS) for pain, Harris Hip Score (HHS). |
| Rykov e col | Direct Anterior (DAA) posterior (AP) | 26/20 | Outcome Score (HOOS); Harris Hip Score (HHS): visual analog scale (VAS). |
| jin e col | Direct Anterior (DAA) posterior (AP) | 195/187 | Length of hospital stay, visual analogue scale (VAS) for pain, Harris Hip Score (HHS). |
Table 2: Harris Hip Score (HHS) of patients undergoing hip arthroplasty through the right anterior or posterior approach.
| Study | Sample | Middle Ages | Previous direct approach | Later approach |
| Moerenhout e col | 55 patients | 69 years old | 94,4 +-8 | 91,4+-13 |
| It's good, col | 100 patients | 68 years | 89,9 +12,7 | 91,3 +-9,4 |
| Jin X et al | 106 patients | 52 years | 92,5±2,3 | 91,6 1,8 |
| Rykov e col | 46 patients | 61 years | 72,8 + 16.9 | 71,0 +- 18,7 |
| Jin Me col | 382 patients | 61 years | 96,5+-10 | 95.5+-9,8 |
Figure 2: Forest-plot graph of the analysis of the functional assessment of the hips of patients undergoing total hip arthroplasty
In the randomized clinical trial by Moerenhout et al [17], of the patients who underwent hip arthroplasty, 27 underwent posterior approach (PA) and 28 underwent direct anterior approach (DAA). The HHS scores showed a better functional recovery for patients who underwent direct anterior access compared to those who underwent posterior access. The VAS score (visual analog scale) was 1.1+-1.9 for AP and 1.0 +- 1.7 for DAA 3 months after the procedure, with no significant variations. In terms of leg length discrepancy, the hip undergoing arthroplasty was 2.2 mm (range -14 to 9 mm) shorter than the ideal length for LAD, and 1.0 mm (range -9 to 10 mm) longer for PA. Surgical time was significantly longer in the DAA group (59 minutes) than for the PA (45.7 minutes). Bon et al [18]. also presented a randomized clinical trial in which 50 patients were included in the PA group and 50 in the DAA group. Surgical time was longer for DAA (70 +- 1.1 minutes) versus 56.7 +- 11 in AP. Hospital stay was 2.8±1.78 days for PA and 2.84±1.25 days for DAA. The HHS score for functional analysis of the hip was 89.9 +- 12.7 for the anterior approach and 91.3 +- 9.4 for the posterior approach. On the pain scale, an index of 19 +- 7 was reported for AP and 18.2 +- 8 for DAA.
For Jin X et al [19], patients in the DAA group (53 participants) had lower hemoglobin levels (24.7 ± 13.3 g/L vs. 34.7 ± 16.7, P less then 0.01) and transfusion rates (9/50 vs. 18/50, P = 0.04) when compared to the AP group (53 participants). The Harris hip score was higher in the DAA group than in the AP group (92.5 ± 2.3 vs. 91.6 ± 1.8, P = 0.03). A shorter hospital stay was also noted for DAA (5.12 ± 1.5 vs. 6.40 ± 2.0 days, P less then 0.01) and shorter operating time (169.7 ± 17.3 vs. 167.5 ± 21.8 min, P = .58). The VAS score for pain was 1.5 +- 0.5 for posterior and 1.4 +- 0.5 for direct anterior access. In the randomized study by Rykov et al [20]. 23 patients were included in the DAA group and 23 in the AP group. The HSS score for the direct anterior approach group was 72.8 +- 16.9 and for the posterior approach 71 +- 18.7. The operative time for the anterior approach group was 9 minutes longer than the posterior approach group (p=0.001). The amount of blood loss in the AAD was 325.7mL compared to 273.7mL in the PA (p=0.24). Most patients were discharged within 195 days of surgery. In the study by Jin M et al21, 183 patients were included in the AAD group and 199 in the PA group. The average duration of the surgical procedure was 81 +- 11.8 minutes for the direct anterior approach and 77+- 10.1 for the posterior approach. The average hospital stay was 2 days longer for the PA. The VAS index for pain was 1.2 +- 0.4 for the DAA group and 1.3 +- 0.4 for AP.
Discussion
The direct anterior approach (DAA) was associated with better functional recovery with a slightly better Harris Hip Score (HHS) when compared to the posterior approach (AP). Regarding the VAS score, there were no significant differences between the two groups in terms of postoperative pain. The anterior approach was associated with a longer surgical time [17,18,19, 20]. Total hip arthroplasty (THA) is considered a successful orthopaedic surgical procedure²². However, 7-15% of patients are unhappy after surgery [23]. Patients continue to experience post-operative pain, which makes it difficult for them to fully return to their duties and activities [24,25]. The likely reasons for the pain include soft tissue damage linked to the trauma of the procedure, fixation failures and instability [26]. This is why it is necessary to choose the ideal surgical approach, reducing the risks and improving the results of the surgery [27]. It is still a matter of debate as to the best approach for THA; the ideal one should have low complication rates, be easily reproducible and cause less damage to soft tissues. Even though there have been numerous initiatives to solve this dilemma over the last decade, it remains controversial [17].
There are several approaches to THA, each with its advantages and disadvantages. However, we will focus on the direct anterior approach (DAA) and the posterior approach (AP). The AP approach, the most commonly performed in the United States and possibly worldwide [28,29], provides excellent visualization and exposure of the acetabulum and femur, as well as avoiding hip abductor rupture [30]. However, it has been linked to a higher risk of dislocation compared to AAD30,31,32 but this threat can be reduced with repair of the posterior capsule and soft tissue, careful positioning of the device and peri-operative attitudes [9].
The AAD uses an intermuscular and inter-nerve access between the sartorius muscle and the tensor fascia latae [30]. Its advantages include a shorter hospital stay [33]. a faster and more functional recovery [10]. and less chance of dislocation [34]. The disadvantages include the risk of injury to the lateral femoral cutaneous nerve (LFCN) [35]. the need for a long learning curve on the part of the surgeon [36,37]. and the risk of intraoperative fractures [38].
Some studies agree that AAD has an efficient post-operative recovery [32,10,38,39,40]. This factor has been attributed to the nature of preserving the muscles, by using an access between the sartorius and tensor fascia lata superficially and more deeply between the rectus femoris and gluteus medius, thus reducing injury to the soft tissues lata [10]. This fact is even supported by radiological studies and biochemical tests, with fewer tendon and muscle injuries recorded on post-operative magnetic resonance imagin [41]. In addition to having lower creatine kinase or myoglobin levels at the start of surgery, which are indicative of muscle damage [42-44]. In the initial period, AAD patients do indeed recover more quickly, but three to six months after surgery, there is no significant difference between the two approaches (AAD versus PA) in terms of range of motion, functional exercise and pain [21]. As for the risk of dislocations, the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) pointed to an increase in the risk of revision surgeries of ATQ in AP indicated for recurrent dislocations [9]. In addition, three meta-analyses have also reported a higher risk than DAA [31,32,45].
In both approaches, there is a risk of iatrogenic damage to certain nerves.DAA is more likely to cause injury to the LFCN, with an incidence of 14.8 to 81%, due to its location within the intermuscular plane. As it is a sensory nerve, the patient complains of neuropathic pain and paresthesia, with improvement in 88% of patients after two years [46]. On the other hand, the sciatic nerve is involved in PA due to its posterior location [9]. Although the overall incidence of this injury is low (0.068-1.9%) [46]. the rate of total recovery is less than 50%. [47]. As it is an essential motor nerve for the muscles of the posterior compartment, such an injury can have important functional consequences [9]. During the surgeon's learning curve with the direct approach, there are high risks of postoperative complications and even unfavorable results [48]. This factor is related to the orthopaedic surgeon's familiarization and experience with this technique [49]. For this reason, guidance and supervision by experienced surgeons and the performance of initial cases in less complex conditions is fundamental, and can significantly reduce these complications [50]. In terms of operative time, AAD requires significantly more time than PA, which can be explained by the experience of the orthopedist, the use of intraoperative fluoroscopy and/or the intraoperative fracture table [20]. Since blood loss increases with the duration of surgery, greater loss is observed during this access [51].
Conclusion
The DAA has better early functional results, as well as shorter hospital stays, fewer complaints of pain and soft tissue injury, but it requires more operative time and blood loss than the AP, with the orthopedic surgeon needing a long curve to avoid possible complications, such as injury to the NFCL. As for the PA, it allows visualization of the acetabulum and femur. It does have a risk of dislocation, but this can be avoided by preventative measures, such as repairing the acetabular capsule and muscles. In general, patients reported more pain due to the soft tissue injury, but the functional results are not as fast as the AAD at first, but they soon catch up. This is why the choice of which approach to use should be based on the surgeon's experience, preference and factors related to the patient and their condition.
References
- Vos T, Lim SS, Abbafati C, et al. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258).
Publisher | Google Scholor - Demange MK, Kakuda CMS, Pereira CAM, Sakaki MH, Albuquerque RF da M e. (2007). Influence of the femoral head ligament on hip mechanics. Acta Ortop is a Brazilian tip, 15(4).
Publisher | Google Scholor - Galia CR, Diesel CV, Guimar ães MR, Ribeiro TA. (2017). Update on total hip arthroplasty: a technique still under development. Brazilian Journal of Orthopedics, 52(5).
Publisher | Google Scholor - Moreira EM, Vaz MR, Rivero LG, et al. (2021). Arthrosis: knowledge profile of Bajeense women on prevention , diagnosis and treatment . Brazilian Journal of Development, 7(9).
Publisher | Google Scholor - Park S, Shin BK. (2022). Intermittent fasting with a high-protein diet mitigated osteoarthritis symptoms by increasing lean body mass and reducing inflammation in osteoarthritic rats with Alzheimer’s disease-like dementia. Br J Nutr,127(1):55-67.
Publisher | Google Scholor - Garland A, Bülow E, Lenguerrand E, et al. (2021). Prediction of 90-day mortality after total hip arthroplasty. Bone Joint J, 103(3):469-478.
Publisher | Google Scholor - Baron JE, Westermann RW, Bedard NA, Willey MC, Lynch TS et.al. (2020). Is the Actual Failure Rate of Hip Arthroscopy Higher Than Most Published Series? An Analysis of a Private Insurance Database. Iowa Orthop J, 40(1):135-142.
Publisher | Google Scholor - Schwartsmann CR, Boschin LC, Gonçalves RZ, Yépez AK, Spinelli L de F. (2012). Novas superfícies em artroplastia total do quadril. Revista Brasileira de Ortopedia, 47(2).
Publisher | Google Scholor - Ang JJM, Onggo JR, Stokes CM, Ambikaipalan A. (2023). Comparing direct anterior approach versus posterior approach or lateral approach in total hip arthroplasty: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol, 33(7):2773-2792.
Publisher | Google Scholor - Wang Z, Hou JZ, Wu CH, et al. (2018). A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res, 13(1):229.
Publisher | Google Scholor - Jin Z, Wang L, Qin J, Hu H, Wei Q. (2023). Direct anterior approach versus posterolateral approach for total hip arthroplasty in the treatment of femoral neck fractures in elderly patients: a meta-analysis and systematic review. Ann Med, 55(1):1378-1392.
Publisher | Google Scholor - Lazaru P, Bueschges S, Ramadanov N. (2021). Direct anterior approach (DAA) vs. conventional approaches in total hip arthroplasty: A RCT meta-analysis with an overview of related meta-analyses. PLoS One, 16(8):24.
Publisher | Google Scholor - Yan L, Ge L, Dong S, et al. (2023). Evaluation of Comparative Efficacy and Safety of Surgical Approaches for Total Hip Arthroplasty: A Systematic Review and Network Meta-analysis. JAMA Netw Open, 6(1):2253942.
Publisher | Google Scholor - Ramadanov N, Bueschges S, Liu K, Lazaru P, Marintschev I. (2021). Direct anterior approach vs. Super PATH vs. conventional approaches in total hip replacement: A network meta-analysis of randomized controlled trials. Orthop Traumatol Surg Res, 107(8):103058.
Publisher | Google Scholor - Ramadanov N, Bueschges S, Liu K, Lazaru P, Marintschev I. (2021). Comparison of short-term outcomes between direct anterior approach (DAA) and Super PATH in total hip replacement: a systematic review and network meta-analysis of randomized controlled trials. J Orthop Surg Res, 16(1):324.
Publisher | Google Scholor - Ramadanov N. (2022). An Updated Meta-Analysis of Randomized Controlled Trials on Total Hip Arthroplasty through Super PATH versus Conventional Approaches. Orthop Surg, 14(5):807-823.
Publisher | Google Scholor - Moerenhout K, Derome P, Laflamme GY, Leduc S, Gaspard HS, Benoit B. (2020). Direct anterior versus posterior approach for total hip arthroplasty: a multicentre, prospective, randomized clinical trial. Can J Surg, 63(5):412-417.
Publisher | Google Scholor - Bon G, Kacem EB, Lepretre PM, Weissland T, Mertl P. et.al. (2019). Does the direct anterior approach allow earlier recovery of walking following total hip arthroplasty? A randomized prospective trial using accelerometry. Orthop Traumatol Surg Res, 105(3):445-452.
Publisher | Google Scholor - Jin X, Chen G, Chen M, Riaz MN, Wang J. et.al. (2023). Comparison of postoperative outcomes between bikini-incision via direct anterior approach and posterolateral approach in simultaneous bilateral total hip arthroplasty: a randomized controlled trial. Sci Rep, 13(1):7023.
Publisher | Google Scholor - Rykov K, Reininga IHF, Sietsma MS, Knobben BAS, Ten Have BLEF. (2017). Posterolateral vs Direct Anterior Approach in Total Hip Arthroplasty (POLADA Trial): A Randomized Controlled Trial to Assess Differences in Serum Markers. J Arthroplasty, 32(12):3652-3658.
Publisher | Google Scholor - Jin MW, Zhang L, Chu XB, Lv SJ, Zhang. et.al. (2023). Comparison of clinical efficacy between direct anterior approach and posterolateral approach in primary total hip arthroplasty. Eur Rev Med Pharmacol Sci, 27(12):5604-5613.
Publisher | Google Scholor - Putananon C, Tuchinda H, Arirachakaran A, Wongsak S, Narinsorasak T. (2018). Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: network meta-analysis. Eur J Orthop Surg Traumatol, 28(2):255-267
Publisher | Google Scholor - Anakwe RE, Jenkins PJ, Moran M (2011). Predicting dissatisfac- tion after total hip arthroplasty: a study of 850 patients. J Arthro- plasty, 26(2):209-213.
Publisher | Google Scholor - Caton J, Prudhon JL (2011). Over 25 years survival after Charnley’s total hip arthroplasty. Int Orthop, 35(2):185-188.
Publisher | Google Scholor - Restrepo C, Parvizi J, Pour AE, Hozack WJ (2010). Prospec- tive randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty, 25(5):671-679.
Publisher | Google Scholor - Bremer AK, Kalberer F, Pfirrmann CW, Dora C (2011). Soft- tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the trans gluteal approaches. J Bone Jt Surg Br, 93(7):886-889.
Publisher | Google Scholor - Barrett WP, Turner SE, Leopold JP (2013). Prospective ran- domized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty, 28(9):1634-1638.
Publisher | Google Scholor - Waddell J, Johnson K, Hein W, Raabe J, FitzGerald G. et.al. Orthopaedic practice in total hip arthroplasty and total knee arthroplasty: results from the Global Orthopaedic Registry (GLORY). Am J Orthop (Belle Mead NJ), 39(9):5-13.
Publisher | Google Scholor - Chechik O, Khashan M, Lador R, Salai M, Amar E. (2013). Surgical approach and prosthesis fixation in hip arthroplasty worldwide. Arch Orthop Trauma Surg, 133(11):1595-600.
Publisher | Google Scholor - Talia AJ, Coetzee C, Tirosh O, Tran P (2018) Comparison of outcome measures and complication rates following three different approaches for primary total hip arthroplasty: a pragmatic randomised controlled trial. Trials, 19(1):13.
Publisher | Google Scholor - Docter S, Philpott HT, Godkin L, Bryant D, Somerville L, et.al. (2020) Comparison of intra and post-opera- tive complication rates among surgical approaches in total hip arthro- plasty: a systematic review and meta-analysis. J Orthop, 20:310-325.
Publisher | Google Scholor - Higgins BT, Barlow DR, Heagerty NE, Lin TJ (2015). Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplast, 30(3):419-434.
Publisher | Google Scholor - Christensen CP, Karthikeyan T, Jacobs CA (2014). Greater preva- lence of wound complications requiring reoperation with direct ante- rior approach total hip arthroplasty. J Arthroplast, 29(9):1839-1841.
Publisher | Google Scholor - Sheth D, Cafri G, Inacio MCS, Paxton EW, Namba RS. (2015). Ante- rior and anterolateral approaches for THA are associated with lower dislocation risk without higher revision risk. Clin Orthop Relat Res, 473(11):3401-3408.
Publisher | Google Scholor - Barton C, Kim PR. (2009). Complications of the direct ante- rior approach for total hip arthroplasty. Orthop Clin North Am, 40(3):371-375.
Publisher | Google Scholor - Bhandari M, Matta JM, Dodgin D, Clark C, Kregor P. et.al. (2009) Outcomes following the single-incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin North Am, 40(3):329-342.
Publisher | Google Scholor - Hartford JM, Bellino MJ. (2017). The learning curve for the direct anterior approach for total hip arthroplasty: a single surgeon’s first 500 cases. Hip Int, 27(5):483-488.
Publisher | Google Scholor - Jia F, Guo B, Xu F, Hou Y, Tang X. et.al. (2018). A comparison of clinical, radiographic and surgical outcomes of total hip arthro- plasty between direct anterior and posterior approaches: a systematic review and meta-analysis. Hip Int, 29(6):584-596.
Publisher | Google Scholor - Meermans G, Konan S, Das R, Volpin A, Haddad FS (2017) The direct anterior approach in total hip arthroplasty. Bone Joint J, 99(6):732-740.
Publisher | Google Scholor - Yue C, Kang P, Pei F (2015). Comparison of direct anterior and lateral approaches in total hip arthroplasty: a systematic review and meta- analysis (PRISMA). Medicine 94(50):2126-2126.
Publisher | Google Scholor - Martin CT, Pugely AJ, Gao Y, Clark CR (2013). A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplasty, 28(5):849-854.
Publisher | Google Scholor - Zhao HY, Kang PD, Xia YY, Shi XJ, Nie Y. (2017) Com- parison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplasty, 32(11):3421-3428.
Publisher | Google Scholor - De Anta-Díaz B, Serralta-Gomis J, Lizaur-Utrilla A, Benavidez E, López-Prats FA. (2016). No differences between direct anterior and lateral approach for primary total hip arthroplasty related to muscle damage or functional outcome. Int Orthop, 40(10):2025-2030.
Publisher | Google Scholor - Nistor DV, Caterev S, Bolboacă SD, Cosma D, Lucaciu DOG. et.al. (2017). Transitioning to the direct anterior approach in total hip arthroplasty. Is it a true muscle sparing approach when performed by a low volume hip replacement surgeon? Int Orthop, 41(11):2245-2252.
Publisher | Google Scholor - Miller LE, Gondusky JS, Kamath AF, Boettner F, Wright J. et.al. (2018) Influence of surgical approach on complication risk in primary total hip arthroplasty. Acta Orthop, 89(3):289-294.
Publisher | Google Scholor - Patel NK, Krumme J, Golladay GJ (2021). Incidence, injury mecha- nisms, and recovery of iatrogenic nerve injuries during hip and knee arthroplasty. JAAOS J Am Acad Orthop Surg, 29(19):940-949.
Publisher | Google Scholor - Hasija R, Kelly JJ, Shah NV, Newman JM. et.al. (2018) Nerve injuries associated with total hip arthro- plasty. J Clin Orthop Trauma, 9(1):81-86.
Publisher | Google Scholor - Hasija R, Kelly JJ, Shah NV, Newman JM, Chan JJ. et.al. (2018). Nerve injuries associated with total hip arthro- plasty. J Clin Orthop Trauma, 9(1):81-86.
Publisher | Google Scholor - Hasija R, Kelly JJ, Shah NV, Newman JM, Chan JJ. et.al. (2018) Nerve injuries associated with total hip arthro- plasty. J Clin Orthop Trauma, 9(1):81-86.
Publisher | Google Scholor - Peters RM, Ten Have B, Rykov K, Van Steenbergen L, Putter H. et.al. (2022) The learning curve of the direct anterior approach is 100 cases: an analysis based on 15,875 total hip arthroplasties in the dutch arthroplasty register. Acta Orthop, 93:775-782.
Publisher | Google Scholor - Ross D, Erkocak O, Rasouli MR, Parvizi J. (2019). Operative Time Directly Correlates with Blood Loss and Need for Blood Transfusion in Total Joint Arthroplasty. Arch Bone Jt Surg, 7(3):229-234.
Publisher | Google Scholor