Research Article
Diffuse Cerebral Infarction Due to Massive Thromboembolism in A Young Male Patient With ALK-Positive Non-Small Cell Lung Cancer: Is the ALK Rearrangement Related to Thrombosis?
- Zuhat Urakci *
- Sezai Tunc
- Fatma Keskin
- Hayati Arvas
- Zeynep Oruc
- Abdurrahman Isikdogan
Dicle University, Department of Medical Oncology, Diyarbakir, Turkey.
*Corresponding Author: Zuhat Urakci, Dicle University, Department of Medical Oncology, Diyarbakir, Turkey.
Citation: Urakci Z., Tunc S., Keskin F., Arvas H., Oruc Z. et al. (2023). Diffuse Cerebral Infarction Due to Massive Thromboembolism in A Young Male Patient With ALK-Positive Non-Small Cell Lung Cancer: Is the ALK Rearrangement Related to Thrombosis? Clinical Case Reports and Studies, BRS Publishers. 2(6); DOI: 10.59657/2837-2565.brs.23.046
Copyright: © 2023 Zuhat Urakci, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 02, 2023 | Accepted: June 30, 2023 | Published: July 03, 2023
Abstract
The risk of thromboembolism is high in patients with lung adenocarcinoma, especially in patients with ALK rearrangement. The mechanism of thromboembolism due to ALK rearrangement is still unknown. Here, we present a case of diffuse cerebral infarction due to massive thromboembolism in a 25-year-old young male patient with lung adenocarcinoma and ALK rearrangement. Thrombosis, apart from metastasis, should be kept in mind when cranial symptoms develop in patients with lung cancer with ALK rearrangement. In addition, these patients should be followed closely in terms of thrombosis both at diagnosis and during treatment.
Keywords: non-small cell lung cancer; ALK rearrangement; thromboembolism
Introduction
The risk of thromboembolism is increased in cancer patients and its incidence varies in different tumor types [1]. Thromboembolic events are common in lung cancer and are relatively higher in adenocarcinoma than in other subtypes [2]. Driver mutations in lung adenocarcinoma affect the behavior of cancer and the prognosis of the disease. In addition, these different genomic mutations have been found to be associated with thromboembolic events at varying rates. Anaplastic lymphoma kinase (ALK) rearrangement is detected in approximately 5% of patients with non-small cell lung cancers (NSCLC), and targeted tyrosine kinase therapies can be used in these patients [3]. Patients with ALK rearrangement have an increased risk of both venous and arterial thrombosis [4]. The risk of venous thromboembolism was found to be 3 to 5 times higher in patients with ALK rearrangement [5]. However, there is limited information about arterial thromboembolism risk and mechanism in this patient group with driver mutation. The mechanism of thromboembolism in patients with ALK rearrangement is still unclear. Here, we present a case of diffuse brain infarction due to massive thromboembolism in a young male patient with ALK-positive non-small cell lung cancer.
Case Report
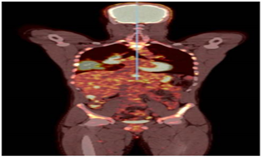
A 25-year-old male patient was admitted to our clinic with complaints of pain in the pelvic region lasting more than 3 months. The patient had no recent history of any surgery. The patient's weight according to height was within normal limits. On physical examination, there is tenderness in the pelvic region. Positron emission tomography (PET-CT) imaging reveals a lesion with a high probability of primary tumor obliterating the bronchus in the right hilar region, as well as widespread metastatic lesions including pleural, pancreatic, liver, right adrenal, and skeletal system (Figure 1).
Figure 1: PET-CT image of the patient.
The biopsy taken from the mass in the patient's lung was found to be lung adenocarcinoma. Driver mutation tests were requested to make a treatment decision for the patient. However, cisplatin and paclitaxel chemotherapy were started due to the widespread disease, high tumor burden, and rapid clinical progression. In addition, zoledronic acid treatment was given to the patient due to bone metastasis.
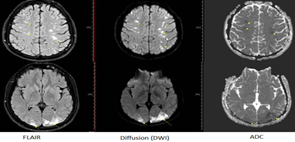
Our patient's leukocyte, hemoglobin, and thrombocyte values were within normal limits. During the follow-up, the patient developed severe headaches, nausea, and blurred vision. In cranial MRI, multiple foci compatible with acute infarction were observed in both cerebellar hemispheres, occipital cortex, white matter, and frontoparietal cortex (Figure 2).
Figure 2: Diffuse areas of acute infarction in both cerebral hemispheres on MRI.
The patient had complaints of pain and temperature increase in the right leg and Homan’s sign was positive. Thrombosis causing a filling defect in the right popliteal vein was observed in lower extremity venous Doppler ultrasonography.
In addition, in the thorax CT angiography of patients with dyspnea, there is a filling defect compatible with embolism in both main pulmonary arteries and in the lobar pulmonary artery leading to the lower lobe on the right side (Figure 3).
Figure 3: Thorax CT angiography has filling defect compatible with embolism in both main pulmonary arteries, on the right also in the branch of the lobar pulmonary artery leading to the lower lobe.
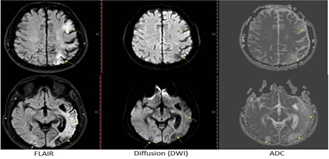
A treatment dose of anti-coagulant was started and a thrombophilia panel was studied. Factor II (G20210A) and V Leiden were homozygous normal, and MTHFR (A1298C and C677T) heterozygous deficiency was found in the thrombophilia panel. Alectinib, a tyrosine kinase inhibitor was administered at a dose of 2x600 mg/day via a nasogastric tube to the patient who was found to have positive ALK rearrangement. Within days, there was an improvement in consciousness, vision problems, and swallowing reflex returned. Partial response to treatment was detected in the control PET-CT imaging of the patient. Significant regression was detected in the cerebral infarct area in cranial MR imaging (Figure 4).The patient's follow-up and treatment continued regularly. Our patient died in the 18th month of follow-up.
Figure 4: Chronic infarcts and parenchymal malasia areas in the left cerebral hemisphere, temporo occipital, and right occipital on MRI.
Conclusion
Thrombosis should be kept in mind, apart from metastasis, when cranial symptoms develop in patients with lung cancer with ALK rearrangement. In addition, patients with ALK rearrangement should be followed closely in terms of thrombosis both at diagnosis and during treatment.
References
- Gaithersburg, MD. (2014). Guidelines for smart grid cybersecurity.
Publisher | Google Scholor - M. Dunn Cavelty and A. Wenger. (2020). Cyber security meets security politics: Complex technology, fragmented politics, and networked science. Contemp Secur Policy, 41(1):5-32.
Publisher | Google Scholor - S. Sadik, M. Ahmed, L. F. Sikos, and A. K. M. Najmul Islam. (2020). Toward a sustainable cybersecurity ecosystem. Computers, 9(3):1-17.
Publisher | Google Scholor - The Role of Internet of Things (IoT) in Smart Grid Technology and Applications.
Publisher | Google Scholor - S. Sengan, V. Subramaniyaswamy, S. K. Nair, V. Indragandhi, J. Manikandan. et al. (2020). Enhancing cyber–physical systems with hybrid smart city cyber security architecture for secure public data-smart network. Future Generation Computer Systems, 112:724-737.
Publisher | Google Scholor - V. K. V. V. Bathalapalli, S. P. Mohanty, E. Kougianos, V. P. Yanambaka, B. K. Baniya. et al. A PUF-based Approach for Sustainable Cybersecurity in Smart Agriculture. Institute of Electrical and Electronics Engineers (IEEE). 375-380.
Publisher | Google Scholor - Intrusion Detection - Prevention Systems: The Ultimate Guide.
Publisher | Google Scholor - S. Spiekermann and L. F. Cranor. (2009). Engineering privacy, IEEE Transactions on Software Engineering, 35(1):67-82.
Publisher | Google Scholor - S. Zeadally, A. S. K. Pathan, C. Alcaraz, and M. Badra, Towards privacy protection in smart grid. Wirel Pers Commun, 73(1):23-50.
Publisher | Google Scholor - Y. Liu, P. Ning, and M. K. Reiter. (2011). False data injection attacks against state estimation in electric power grids, in ACM Transactions on Information and System Security.
Publisher | Google Scholor - E. A. Dada and S. M. Musa. (2016). Smart Cities.
Publisher | Google Scholor - Institute of Electrical and Electronics Engineers Kolkata Section. (2014). National Power Systems Conference 18 2014.12.18-20 Guwahati, and NPSC 18 2014.12.18-20 Guwahati, 2014 Eighteenth National Power Systems Conference (NPSC) 18-20 Dec. 2014, Guwahati, India.
Publisher | Google Scholor - M. Govindarasu. Cyber-Physical Systems Security for Smart Grid.
Publisher | Google Scholor - R. Khatoun and S. Zeadally. (2017). Cybersecurity and privacy solutions in smart cities, IEEE Communications Magazine, 55(3):51-59.
Publisher | Google Scholor - W. Zhang and B. Natarajan. (2018). On the statistical convergence of bias in mode-based Kalman filter for switched systems. EURASIP J Adv Signal Process, 2018(1).
Publisher | Google Scholor - (2019). Cyber Security Breaches Survey, Statistical Release.
Publisher | Google Scholor