Case Report
Diagnostic Dilemma: A Case of Necrotizing Neutrophilic Dermatosis Misdiagnosed as Necrotizing Fasciitis
- Andre Pinto *
- Diogo Conduto
- Rafael Rocha
- Odete Martinho
- Afonso Almeida
- Duarte Garcao
Plastic Surgery, Hospital de Santa Maria - ULSSM - Lisboa, Lisbon, Portugal.
*Corresponding Author: Andre Pinto, Plastic Surgery, Hospital de Santa Maria - ULSSM - Lisboa, Lisbon, Portugal.
Citation: Pinto A, Conduto D, Rocha R, Martinho O, Almeida A, et al. (2025). Diagnostic Dilemma: A Case of Necrotizing Neutrophilic Dermatosis Misdiagnosed as Necrotizing Fasciitis, Clinical Case Reports and Studies, BioRes Scientia Publishers. 9(2):1-5. DOI: 10.59657/2837-2565.brs.25.218
Copyright: © 2025 Andre Pinto, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 16, 2024 | Accepted: January 01, 2025 | Published: January 11, 2025
Abstract
We report the case of a 15-year-old female who presented with a necrotizing neutrophilic dermatosis (NND) following an unknown insect bite on her right leg. Initially misdiagnosed, she developed sepsis and required intermediate care for acute kidney injury and volume support. Through multidisciplinary collaboration between Pediatrics, Infectious Diseases, Dermatology, and Plastic Surgery teams, the diagnosis of NND was suspected and confirmed via skin biopsy. She was successfully treated with corticosteroids and wound care, avoiding surgical intervention typically required for necrotizing fasciitis (NF). This case highlights the importance of considering NND in the differential diagnosis of progressive inflammatory skin lesions and emphasizes the value of conservative management to prevent iatrogenic complications.
Categories: plastic surgery, dermatology, allergy/immunology
Keywords: debridement; fasciitis; multiple skin necrosis; skin blister; necortizing fasciitis; neutrophilic dermatosis
Introduction
Neutrophilic dermatoses (NDs) are rare inflammatory skin disorders characterized by neutrophilic infiltration without identifiable infection [1]. Their clinical presentations vary, including vesicles, papules, nodules, ulcerations, or extracutaneous involvement [2]. The etiology of NDs is often idiopathic and poorly understood [3]. These conditions can resemble necrotizing fasciitis (NF), posing a diagnostic challenge due to overlapping clinical features [2, 4]. Pathergy-a hypersensitivity reaction to trauma-is a hallmark of NDs, where procedures such as biopsies or injections can exacerbate lesions [4]. Misdiagnosing NDs as NF and proceeding with surgical interventions may result in significant iatrogenic harm. Early recognition of NDs, supported by biopsy and imaging findings, is crucial for optimal management [5, 6]. This report describes a challenging case of NND initially mistaken for NF.
Case Presentation
A healthy 15-year-old girl presented to a peripheral healthcare center with extensive cellulitis of the right leg after a suspected insect bite. Symptoms included fever (>38°C), erythema, swelling, and inability to walk. She was treated with amoxicillin/clavulanic acid and admitted for monitoring. Despite treatment, her condition worsened, with circumferential leg inflammation, exudative papules, and systemic inflammatory signs, as shown in below (Figure 1).
Figure 1: Skin lesions at admission
Vesicles and necrotic papules of the right leg, two weeks since symptoms onset
Transferred to our center two weeks after symptoms onset, she exhibited sepsis, acute kidney injury, bilateral pleural effusion, and hemorrhagic blisters. Laboratory tests showed leukocytosis and coagulopathy (platelets: 87,000/μL, INR: 2.38, fibrinogen: 141 mg/dL). Complete blood test results are shown below (Table 1).
Table 1: Blood test results
| Blood test | Result | Normal Value |
| RBC | 2.63 x 10^12/L | 3.8-5.1 |
| Hemoglobin | 8.6 g/dL | 12.0-15.3 |
| Hematocrit | 25.4 % | 36.0-46.0 |
| WBC | 14.60 x10^9/L | 4.0-11.0 |
| Neutrophils | 73.4 / 10.72 % | 1.9-7.5. |
| Monocytes | 8.8 / 1.28 % | 0.1-1.0. |
| Platelets | 78 x10^9/L | 150-450 |
| INR | 2.33 | |
| Urea | 36 mg/dL | 16 - 49 |
| Creatinine | 1.24 mg/dL | 0.50-0.90 |
| Albumin | 1.9 g/dL | 3.5 - 5.2 |
| CRP | 6.75 mg/dL | <0> |
Complete blood test results with normal intervals, at admission.
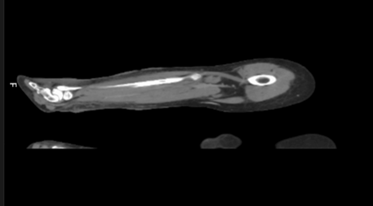
Cultures remained negative, and broad-spectrum antibiotics were administered. A CT scan ruled out NF, showing infection confined to subcutaneous tissue without fascial involvement, specifically absence of deep plane infiltration, emphysema or organized collections (Figure 2).
Figure 2: CT scan of right leg Signs of subcutaneous tissue densification without collections or deep-tissue gas formation
Multidisciplinary discussions among Pediatrics, Infectious Diseases, Dermatology, and Plastic Surgery teams deferred surgical debridement. A skin biopsy was performed to investigate NDs, and corticosteroids (prednisolone 30 mg IV every 12 hours) were initiated. Wound care included Flaminal®, Allevyn®, and Mepilex® dressings (Figure 3).
Figure 3: Wound care Progressive resolution of skin lesions with frequent dressings
Over two weeks, the patient’s condition improved. Biopsy results confirmed NND, showing neutrophilic infiltrate, vasculitis and necrosis. After 45 days of hospitalization, the patient was discharged on prednisolone and cyclosporine, with follow-up care. Scarring was evident but improved progressively (Figure 4).
Figure 4: 8 months after hospital discharge Secondary healing with scarring of previous wounds.
Discussion
Diagnosing NDs is challenging due to their rarity and clinical overlap with NF [1, 7]. Both conditions present with progressive skin lesions, fever, leukocytosis, and systemic inflammatory markers involving necrosis of tissues [8, 9]. Distinguishing between these entities is crucial for appropriate treatment, as one is primarily infectious and the other is inflammatory. NF, however, often involves deep tissue destruction and requires emergent surgical debridement [10, 11]. In contrast, NDs are treated with systemic corticosteroids and conservative wound care [10, 12]. Pathergy is a key differentiator, as trauma-induced lesions in NDs may worsen with surgical interventions [8].
NF is infectious in origin, often followed by trauma and caused by bacteria as Streptococcus pyogenes, Staphylococcus aureus (including MRSA), Clostridium species, or polymicrobial infections [11,13]. Clinical presentation is a rapidly progressing infection of the fascia and subcutaneous tissue with systemic toxicity, severe pain out of proportion, skin changes with eventual necrosis, fever, tachycardia, hypotension and multi-organ dysfunction in advanced cases [11, 13]. Bacterial toxins and enzymes cause tissue destruction, vascular occlusion and necrosis and systemic inflammatory response can lead to septic shock [13].
Histopathology shows necrosis with neutrophilic infiltration and presence of bacteria in tissue samples. Surgical exploration for confirmation and positive cultures is the current diagnostic criteria [13]. Treatment needs emergent surgical debridement, broad-spectrum antibiotics and supportive care. [7, 11, 13].
NND is an inflammatory condition, non-infectious in nature associated with immune dysregulation or underlying systemic or inflammatory disorders [9]. Clinical presentation is a progressive painful skin necrotic plaques, nodules or ulcers, resembling NF but without signs of systemic infection [6, 10]. Immune mediated neutrophilic infiltration cause tissue necrosis without pathogen involvement and histopathology shows neutrophilic infiltrate with tissue necrosis without organisms [5, 9]. Diagnosis is based on clinical suspicion with exclusion of infectious causes such as NF and biopsy with absence of infection and no microbial growth [2, 6, 12]. Treatment involves high-dose systemic corticosteroids, immunosuppressive agents as cyclosporine and treatment of underlying systemic disease [9, 10]. Key diagnostic differences listed in table below (Table 2) [5, 6, 9-13].
Table 2: Key diagnostic differences
| Feature | Necrotizing Fasciitis | Necrotizing Neutrophilic Dermatosis |
| Cause | Infectious (bacterial) | Non-infectious (immune-mediated) |
| Systemic Signs | Prominent (fever, hypotension, sepsis) | Mild or absent; prominent in advanced cases |
| Pain | Severe and out of proportion | Severe but more localized |
| Tissue Involvement | Deep fascia and subcutaneous tissue | Dermis and subcutaneous tissue |
| Cultures | Positive (bacteria detected) | Negative (sterile) |
| Histopathology | Neutrophils with bacterial presence | Neutrophils without bacteria |
| Treatment | Surgical debridement, antibiotics | Corticosteroids, immunosuppressants |
Key diagnostic differences between NF and NND
Accurate diagnosis often requires tissue biopsy, culture, and imaging to distinguish between these two entities, as the treatment strategies are fundamentally different. In this case, imaging findings, slow disease progression and multidisciplinary collaboration helped avoid unnecessary surgery. Early corticosteroid therapy supported the diagnosis, with the patient showing rapid improvement. This case emphasizes the importance of a multidisciplinary approach, especially involving dermatology teams, to navigate ambiguous clinical presentations and reduce morbidity.
Conclusion
This case underscores the diagnostic complexity of NND and the importance of distinguishing it from NF. High clinical suspicion and conservative management can prevent iatrogenic complications. Multidisciplinary collaboration and early biopsy are essential for accurate diagnosis and effective treatment. Awareness of NND as a differential diagnosis for necrotizing skin lesions may improve outcomes and reduce unnecessary surgical interventions.
Declarations
Human subjects
Consent for treatment and open access publication was obtained or waived by all participants in this study.
Conflicts of interest
In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info
All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships
All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships
All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- Otero TM, Barber SR, Yeh DD. (2017). Necrotizing Soft Tissue Infection or Sweet Syndrome: Surgery Versus No Surgery?: A Case Report. A & A Case Reports, 8(7):182-185.
Publisher | Google Scholor - Callen JP. (2002). Neutrophilic dermatoses. Dermatol Clin, 409:419.
Publisher | Google Scholor - Kobayashi SD, Malachowa N, DeLeo FR. (2018). Neutrophils and bacterial immune evasion. J Innate Immun, 10:432:441.
Publisher | Google Scholor - Shah N, Asdourian MS, Jacoby TV. (2022). Neutrophilic dermatosis and management strategies for the inpatient dermatologist. Current dermatology reports. 3:146-157.
Publisher | Google Scholor - Nelson CA, Stephen S, Ashchyan HJ, James WD, Micheletti RG, Rosenbach M. (2018). Neutrophilic dermatoses: pathogenesis, sweet syndrome, neutrophilic eccrine hidradenitis, and Behçet disease. J Am Acad Dermatol, 76(6): 987-1006.
Publisher | Google Scholor - Sanchez IM, Lowenstein S, Johnson KA. (2019). Clinical features of neutrophilic dermatosis variants resembling necrotizing fasciitis. JAMA dermatology. 155:79-84.
Publisher | Google Scholor - Wong CH, Yam AKT, Tan ABH. (2008).
Publisher | Google Scholor - Rahman S, Daveluy S. (2022). Pathergy test. Treasure Island (FL). StatPearls Publishing.
Publisher | Google Scholor - Kroshinsky D, Alloo A, Rothschild B. (2012). Necrotizing Sweet syndrome: a new variant of neutrophilic dermatosis mimicking necrotizing fasciitis. J. Am. Acad. Dermatol, 67:945-954.
Publisher | Google Scholor - Gowda A, Christensen L, Polly S. (2020). Necrotizing neutrophilic dermatosis: a diagnostic challenge with a need for multi-disciplinary recognition, a case report. Annals of Medicine and Surgery, 57:299-302.
Publisher | Google Scholor - Allaw F, Wehbe S, Kanj SS. (2024). Necrotizing fasciitis: an update on epidemiology, diagnostic methods, and treatment. Curr Opin Infect Dis, 37:105-111.
Publisher | Google Scholor - Su WP, Liu HN. (1986). Diagnostic criteria for Sweet's syndrome. Cutis, 37:167-174.
Publisher | Google Scholor - Misiakos E, Bagias G, Patapis P. (2014). Current concepts in the management of necrotizing fasciitis. Frontiers in surgery vol, 1:29-36.
Publisher | Google Scholor