Review article
Development of Insufficiency Fractures Secondary to Osteometabolic Diseases-A Systematic Review with Meta-Analysis
- Bianca Gabriella de Oliveira 1*
- Rafael Akio Watanabe Nakakogue 2
- Guilherme Augusto Pereira 2
- Isabella Silva Carvalho 2
- Luciana de Matos Mota Oliveira 3
- Melissa Alves Aires Marques 4
1Medical Student at Universidade Salvador-UNIFACS, Salvador, BA, Brazil
2Resident doctor in Orthopedics and Traumatology at Hospital Municipal Dr. Mário Gatti, Campinas, SP
3Resident doctor in Orthopedics and Traumatology at Hospital Geral Cleriston Andrade, Feira de Santana, BA
4Medical Student at the Iguaçu University, Itaperuna, RJ.
*Corresponding Author: Bianca Gabriella de Oliveira, Medical Student at Universidade Salvador-UNIFACS, Salvador, BA, Brazil
Citation: Bianca G. Oliveira, R.A.W. Nakakogue, Guilherme A. Pereira, Isabella S. Carvalho, L.M.M. Oliveira. (2024). Development of Insufficiency Fractures Secondary to Osteo metabolic Diseases-A Systematic Review with Meta-Analysis, Clinical Interventions and Clinical Trials, BioRes Scientia Publishers. 2(1):1-8. DOI: 10.59657/2993-1096.brs.24.014
Copyright: © 2024 Bianca Gabriella de Oliveira, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 06, 2024 | Accepted: February 21, 2024 | Published: February 26, 2024
Abstract
Osteometabolic diseases, especially osteopenia and osteoporosis, are degenerative pathologies caused by excessive loss of bone mineral density. The risk factors are diverse: hormonal factors, genetic predisposition, inadequate diet, obesity, sedentary lifestyle, diabetes mellitus, kidney disorders, autoimmune diseases, smoking, however, prolonged immobilization plays an important role. This study aims to analyze the development of insufficiency fractures secondary to osteometabolic diseases. This is a systematic literature review carried out using databases indexed in the Medical Literature Analysis and Retrieval System Online (MEDLINE), in accordance with the precepts established by the PRISMA methodology (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). Five articles were selected to analyze the results, including patients with osteopenia taking medication who suffered fractures and patients with osteopenia without adequate treatment who suffered fractures. It was possible to observe that the number of fractures due to insufficiency in patients without treatment for osteopenia proved to be relatively higher when compared to the group of individuals with insufficiency taking medication.
Keywords: osteoporosis; osteoporotic fractures; metabolic bone diseases
Introduction
Osteometabolic diseases, especially osteopenia and osteoporosis, are degenerative pathologies caused by the excessive loss of bone mineral density. Historically, in 1960 it became the focus of worldwide attention, evolving scientifically into an Osteoporosis Consensus in 2001, due to the context of the "21st Century epidemic", resulting from changes in the world's demographic profile, leading to increased longevity and lower birth rates, especially in the United States of America and the European Community [1]. In the eutrophic skeleton, bone is in a continuous state of renewal and resorption. As this balance is altered, with a decrease in neoformation and an increase in absorption, osteopenia develops, depending on the degree, up to osteoporosis.2 This second pathology is present in more than 200 million adults worldwide, and is multifactorial, characterized by low bone mass, poor bone quality and an increased risk of fragility fractures.3,4,5 The test used to diagnose these diseases is bone densitometry, with T-Score values for osteopenia showing a decrease in BMD of between -1.1 and -2.4 standard deviations below the average for the young adult population, while in osteoporosis BMD is - 2.5 or more standard deviations [2].
The risk factors are diverse: hormonal factors, genetic predisposition, inadequate diet, obesity, sedentary lifestyle, diabetes mellitus, kidney disorders, autoimmune diseases, smoking, but prolonged immobilization plays a prominent role. In the context of prolonged immobilization secondary to fractures, both bone loss and sarcopenia are issues of public health impact, complications of underlying diseases and loss of quality of life for affected patients, limiting the development of daily and habitual life activities. Another point that stands out among the probable etiologies is hormonal dysfunction: estrogen deficiency in the female population from the peri-menopausal period onwards is associated with reduced bone calcium absorption, as well as significant changes in the fracture healing cascade in women with osteoporosis [3,4,6]. After the age of 50, approximately half of the population will have osteopenia or osteoporosis, of which 50% will suffer at least one fracture as a result of minor trauma. Osteoporotic fractures occur every three seconds worldwide, and this number tends to increase as the population ages [7,8,9,10]. The aim of this study is to analyze the development of insufficiency fractures secondary to osteometabolic diseases. It was carried out by means of a systematic literature review with meta-analysis, contributing to the scientific environment and medical management for diagnosis and therapeutic conduct. Taking into account the growth in the field of integrative medicine and the increase in life expectancy, more and more research is needed to help maintain quality of life.
Methodology
The search for complete articles was carried out through the PubMed, Scielo and Lilacs databases, using the following descriptors according to the Descriptors in Health Sciences (DeCS): "osteoporosis", "osteoporotic fractures" and "metabolic bone diseases". The selection criteria were free articles published in the last ten years, in Portuguese and English. After reading these, certain articles were excluded because they did not correspond to the theme. Keywords and Boolean operators were used as a search strategy: "osteoporosis" AND "osteoporotic fractures" OR "metabolic bone diseases". As this is a meta-analysis of published studies, approval by the ethics committee or institutional scientific review board was waived. This systematic review and meta-analysis study used the Preferred Reporting Items for Systematic Reviews and Metaanalyses (PRISMA) guideline as a guide for its development [11].
The PICOS principle (Population, Intervention, Comparator, Outcomes and Experimental Design) was used as an eligibility criterion.
1) Population: patients with osteopenia
2) Intervention: drug treatment
3) Comparator: patients with osteopenia taking medication who suffered fractures and patients with osteopenia without adequate treatment who suffered fractures.
4) Outcome: drug treatment efficacy rate.
5) Experimental design: Randomized controlled trial.
Studies were included if they included: [1] studies with humans [2] studies with a sample of osteopenia patients being treated or not [3] osteopenia patients who have suffered fractures [4] age over 59 years [5] studies published between 2013-2023 [5] original studies, primarily randomized clinical trials.
Exclusion criteria for studies
Non-randomized clinical trials, cohort studies, meta-analyses, reference articles and books [2] Studies conducted on animals [3] Studies that did not analyze osteometabolic diseases as causes of fractures.
The Cochrane Collaboration tool was used to analyze the methodological quality of the selected studies to determine the risk of bias.12 Each study was analyzed for randomization, blinding of the evaluator, the team, selective reporting, incomplete data and unknown source of bias [13].
The systematic review protocol was registered in the International prospective register of systematic reviews (PROSPERO) under ID CRD42023473256 in order to improve the quality and suitability of the results to the proposed objectives.
Results
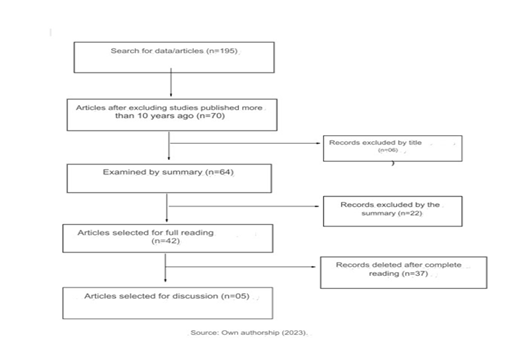
Initially, 195 articles were selected, excluding those that had been published for more than 10 years, leaving 70 articles. The titles were analyzed and 6 articles were removed, leaving 42 articles to be read in full. At the end of the process, five articles were selected for analysis of the results. Figure 1 shows the flowchart used during the selection phases of the scientific articles, using the PRISMA methodology as a basis (Figure 1).
Figure 1: Screening for study selection according to the PRISMA methodology.
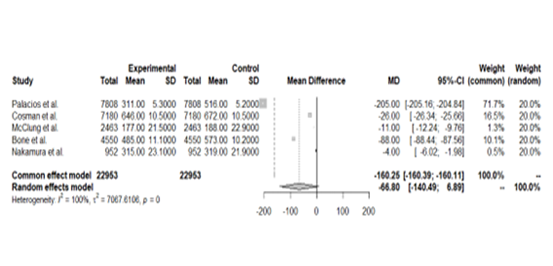
The 05 studies selected included patients with osteopenia who were victims of fractures, whether or not they had undergone drug treatment, and the drug of choice was not taken into account as a selection criterion. A total of 22,953 patients were included, of whom 1,934 had fractures due to insufficiency even when undergoing treatment for osteopenia, and 2,268 had not undergone treatment for the condition and were victims of fractures. Most of the study population (81.6%) had osteometabolic pathology, but did not suffer fractures during the period analyzed. Table 1 shows the studies selected for analysis and a summary of the results obtained (Table 1) [14,15,16,17,18,19]. Figure 2 shows the analysis of fractures by insufficiency (Figure 2) [14,15,16,17,18,19].
Figure 2: Analysis of insufficiency fractures.
Table 1: Insufficiency fractures in patients undergoing or not undergoing treatment for the pathology
| Study | Sample patients with osteopenia | Insufficiency fracture in patients undergoing |
| Palacios et al | 7,808 | 311+5.3 |
| Cosman et al | 7,180 | 646 +10.5 |
| McClung e col | 2.463 | 177 +-21.5 |
| Bone et al | 4,550 | 485 +- 11.1 |
| Nakamura and col | 952 | 315+-23.1 |
| Source: Own preparation (2023) | ||
| Study | Sample patients with osteopenia | F+ Insufficiency fractures in patients undergoing treatment for osteopenia | Insufficiency fractures in patients without treatment for osteopenia |
| Palacios e col | 7.808 | 311 +-5,3 | 516 +-5.2 |
| Cosman e col | 7.18 | 646 +- 10.5 | 672 +- 10.5 |
| McClung e col | 2.463 | 177 +-21.5 | 188 +- 22.9 |
| Bone e col | 4.55 | 485 +- 11.1 | 573 +- 10.2 |
| Nakamura col | 952 | 315+- 23.1 | 319 +-21.9 |
| Fonte: Elaboração própria (2023) | |||
Discussion
The number of insufficiency fractures in patients without treatment for osteopenia has been shown to be relatively higher when compared to the group of individuals with insufficiency taking medications such as denosumab and romosozumab, for example [14,15,16,17,18,19]. The populations most at risk of osteoporosis include individuals subjected to prolonged disuse and the elderly. Disuse, due to prolonged bed rest, immobilization, paralysis and spaceflight-induced unloading, is related to low bone mass and an increased risk of fractures [20,21,22]. Bone is a very dynamic organ that is attuned to the mechanical environment, so prolonged periods of disuse result in lasting and important changes in bone mass, microarchitecture and strength [23,24]. In the event of a fracture, treatment is instituted based on the principle: it can be conservative or surgical, both of which have the potential to have musculoskeletal repercussions. Disuse of the limb, mostly secondary to immobilization and/or mechanical restriction of movement, leads to a decrease in mechanical tension on the bones, which results in a decrease in the stimulus for bone formation and a disproportionate increase in bone resorption (action of osteoclasts), favoring osteopenia. Muscle strength in the bone stimulates the production of osteoblasts, Wolff's law, since there is a direct relationship between muscle strength and increased bone density. It is possible to state that bone tissue remodels itself in response to mechanical stimuli applied to it, adapting to become stronger and more resistant to the forces exerted, through the processes of bone remodeling and resorption [25,26].
Studies show that the highest prevalence of hospital immobility is due to fractures. Osteopenia and osteoporosis are bone disorders characterized by decreased bone mass and compromised structural strength, resulting in a structural bone deficit and increasing susceptibility to insufficiency fractures. After the age of 40, alterations in inflammatory mediators such as neutrophils, the cytokine Midkine (Mdk) and IL-6 can compromise the entire bone healing cascade in osteoporotic women. If they are elevated, they significantly reduce cell renewal activity, promoting poor bone remodeling [27,28]. Bone trophism is associated with the mechanical stresses that the skeleton receives. In cases of immobilization or decreased function, the organism realizes that to maintain structural integrity, all bone mass is not necessary, resulting in a decrease in both bone mass and BMD [29]. Most fractures that affect skeletally immature individuals with open physes are treated conventionally with plaster immobilization [30]. Due to the restriction of load and immobilization, there is loss of bone mineral tissue, functional limitations and muscular atrophy.31,32 Patients with mineral loss after a fracture can take years to recover or have a partial recovery [33,34,35,36,37]. This transient bone mineral deficit can delay rehabilitation and return to activities of daily living [38].
In the process of fracture consolidation, the impact of mechanical load is a complicated issue, which needs to be considered separately from aspects of changes in bone remodeling induced by disuse [39]. However, it is known that the compromise of the mechanical environment associated with immobilization and restrictions load in the conservative or surgical treatment of fractures and followed by consolidation problems and fractures induced by disuse [40]. Immobilization stimulates resorption and reduces bone formation [41]. Even though orthopedics has evolved towards immobilizing patients less and providing early action of physiotherapy, yet many individuals suffer from hypoactivity for long periods.42 Therefore, it is recommended to restrict it to the smallest possible segment and use it over a shorter period of days [43,44,45,46]. Bone healing is divided into two: direct and indirect. While direct occurs through high stability and low interfragmentary movement, for example with compression plates, indirect occurs through the formation of bone callus and is induced by a low degree of stability and considerable interfragmentary movement, for example the use of internal or external splints [47]. Thus, the appropriate balance between mobilization or load bearing and fracture stability is influenced by the anatomical location of the fracture and the surgical concept [48].
Bone mass recovery in response to physical exercise and pharmacotherapy has been studied in several models of disuse and unloading. Therefore, the most natural treatment for osteoporosis due to disuse is physical exercise, even if some of the disuse conditions do not allow remobilization. This combined therapy of specific medications and physical activity appears to be effective in combating, even partially, the bone loss observed. It should be noted that bone loss induced by bed rest continues in the first weeks after ambulation [49,50]. In relation to the drugs used, there are two classes of drugs for osteoporosis, anti-resorptive or anti-catabolic drugs and bone formation stimulators or anabolic drugs. The first class acts by inhibiting osteoclasts, responsible for initiating bone remodeling, being subdivided into hormonal drugs, bisphosphonates. and biological. Anabolic drugs, on the other hand, exert the function of stimulating bone formation, through osteoblasts, and are therefore stimulators of bone metabolism [51]. All patients with bone loss, or those at risk of bone loss, should be advised to supplement or increase their dietary intake of calcium and vitamin D. Since approximately 50% of the calcium ingested by the adult population is absorbed by the intestine and there is a decrease in with age, with vitamin D being responsible for the absorption of intestinal calcium, making supplementation necessary in elderly, hospitalized and sedentary people [52,53,54,55,56]. The treatment of osteoporosis prevents high mortality rates after fractures due to frailty in the first year after fracture (30%) and also leads to a reduction in mortality and an improvement in the ability to carry out activities of daily living (90%) [57,58,59,60,61,62].
Conclusion
It is already known that immobilization or disuse are conditions that may be associated with a decrease in bone mass. Bone deposition is regulated by the amount of tension applied, which means that people immobilized after fractures can suffer from osteopenia, even over a short period. As bone biomechanics is sensitive to physical stimuli, altering its mass, it is important to highlight the importance of a postoperative period with greater mobility and overload as early as possible. Furthermore, the higher prevalence in women is due to the reduction in estrogen levels in the peri-menopausal period, which can reduce bone absorption of calcium, increasing the predisposition to fractures as a result of low-energy trauma and delayed bone healing. Bone is a living tissue that is continually renewed.
References
- (2001). NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA, 285:785-795.
Publisher | Google Scholor - Kanis JA, (1996). Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 9(8):1137-1141. Comment in: J Bone Miner Res, 11(8):1199-1201.
Publisher | Google Scholor - Pisani P,Renna MD, Conversano F, et al. (2016). Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop, 7(3):171-181.
Publisher | Google Scholor - Cosman F, de Beur SJ, LeBoff MS, et al. (2017). Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int, 25(10):2359-2381.
Publisher | Google Scholor - Rachner TD, Khosla S, Hofbauer LC. (2011). Osteoporosis: now and the future. Lancet, 377:1276-1287
Publisher | Google Scholor - Black DM, Rosen CJ. (2016). Clinical Practice. Postmenopausal Osteopo- rosis. N Engl J Med, 374(03):254-262.
Publisher | Google Scholor - Froes NDTC, Pereira E dos S, Negrelli WF. (2002). Fatores de risco da osteoporose: prevenção e detecção através do monitoramento clínico e genético. Acta ortop bras, 10(1):52-56.
Publisher | Google Scholor - Souza MP. (2010). Osteoporosis Diagnosis and Treatment. Rev Bras Ortop, 45(03):220-229
Publisher | Google Scholor - Kurrle LC. (2020).
Publisher | Google Scholor - Moher D, Liberati A, Tetzlaff J, Altman DG; (2009). PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med, 6(7)
Publisher | Google Scholor - Higgins JP, Altman DG, Gøtzsche PC, et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ, 343(5928):18.
Publisher | Google Scholor - DerSimonian R, Laird N. (1986). Meta-analysis in clinical trials. Control Clin Trials, 7(3):177-188.
Publisher | Google Scholor - Palacios S, Kalouche-Khalil L, Rizzoli R, et al. (2015). Treatment with denosumab reduces secondary fracture risk in women with postmenopausal osteoporosis. Climacteric, 18(6):805-812.
Publisher | Google Scholor - Cosman F, Crittenden DB, Adachi JD, et al. (2016). Romosozumab Treatment in Postmenopausal Women with Osteoporosis. N Engl J Med, 375(16):1532-1543.
Publisher | Google Scholor - McClung MR, Williams GC, Hattersley G, Fitzpatrick LA, Wang Y et.al. (2018). Geography of Fracture Incidence in Postmenopausal Women with Osteoporosis Treated with Abaloparatide [published correction appears in Calcif Tissue Int. Calcif Tissue Int, 102(6):627-633.
Publisher | Google Scholor - Bone HG, Wagman RB, Brandi ML, et al. (2017). 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol, 5(7):513-523.
Publisher | Google Scholor - Nakamura T, Matsumoto T, Sugimoto T, et al. (2014). Clinical Trials Express: fracture risk reduction with denosumab in Japanese postmenopausal women and men with osteoporosis: denosumab fracture intervention randomized placebo controlled trial (DIRECT). J Clin Endocrinol Metab, 99(7):2599-2607.
Publisher | Google Scholor - Kurrle LC. (2020).
Publisher | Google Scholor - Sinaki M (2022). Exercise and osteoporosis. Arch Phys Med Rehabil, 70(3):220-229.
Publisher | Google Scholor - Barbosa L. (2022). Ocorrência de Osteoporose e Fraturas em mulheres Pós-Menopausa : Revisão de Literatura Occurrence of Osteoporosis and Fractures in Postmenopausal women : Literature Review. Brazilian Journal of Health Review, v, 5(1):2783-2792.
Publisher | Google Scholor - Rolvien T, Amling M. (2022). Disuse Osteoporosis: Clinical and Mechanistic Insights. Calcif Tissue Int,110(5):592-604.
Publisher | Google Scholor - LeBlanc AD,Spector ER,Evans HJ,Sibonga JD.(2007). Skeletal responses to space flight and the bed rest analog: a review. J Musculoskelet Neuronal Interact. 7(1):33-47.
Publisher | Google Scholor - Cosman F, de Beur SJ, LeBoff MS, et al. (2014). Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int, 25(10):2359-2381.
Publisher | Google Scholor - Lloyd SA, Lang CH, Zhang Y, et al. (2014). Interdependence of muscle atrophy and bone loss induced by mechanical unloading. J Bone Miner Res, 29(5):1118-1130
Publisher | Google Scholor - Ellman R, Grasso DJ, van Vliet M, et al. (2014). Combined effects of botulinum toxin injection and hind limb unloading on bone and muscle. Calcif Tissue Int, 94(3):327-337.
Publisher | Google Scholor - Lloyd SA, Lewis GS, Zhang Y, Paul EM, Donahue HJ. (2012). Connexin 43 deficiency attenuates loss of trabecular bone and prevents suppression of cortical bone formation during unloading. J Bone Miner Res, 27(11):2359-2372.
Publisher | Google Scholor - Schoenau E, Frost HM. (2002). The
Publisher | Google Scholor - Goldberg VM, Aadalen R. (1978). Distal tibial epiphyseal injuries: the role of athletics in 53 cases. Am J Sports Med, 6:263-268
Publisher | Google Scholor - Behm DG, St-Pierre DM. (1997). Fatigue characteristics following ankle fractures. Med Sci Sports Exerc, 29:1115-1123.
Publisher | Google Scholor - Bloomfield SA. (1997). Changes in musculoskeletal structure and function with pro- longed bed rest. Med Sci Sports Exerc, 29:197-206.
Publisher | Google Scholor - Edgerton VR, Roy RR, Allen DL, Monti RJ. (2002). Adaptations in skeletal muscle disuse or decreased-use atrophy. Am J Phys Med Rehabil, 81(11):127-147.
Publisher | Google Scholor - Cattermole HC,Cook JE,Fordham JN,Muckle DS,Cunningham JL. (1997). Bone mineral changes during tibial fracture healing. Clin Orthop Relat Res, 339:190-196.
Publisher | Google Scholor - Kannus P, Jarvinen M, Sievanen H, Oja P, Vuori I. (1994). Osteoporosis in men with a history of tibial fracture. J Bone Miner Res, 9:423-429
Publisher | Google Scholor - Sarangi PP, Ward AJ, Smith EJ, Staddon GE, Atkins RM. (1993). Algodystrophy and osteoporosis after tibial fractures. J Bone Joint Surg Br,75:450-452.
Publisher | Google Scholor - Van der Poest Clement E, van der Wiel H, Patka P, Roos JC, Lips P. (1999). Long-term consequences of fracture of the lower leg: cross-sectional study and long-term lon- gitudinal follow-up of bone mineral density in the hip after fracture of lower leg. Bone, 24:131-134.
Publisher | Google Scholor - Weinreb M, Rodan GA, Thompson DD. (1991). Immobilization-related bone loss in the rat is increased by calcium deficiency. Calcif Tissue Int, 48:93-100.
Publisher | Google Scholor - Szalay EA, Harriman D, Eastlund B, Mercer D. (2008). Quantifying postoperative bone loss in children. J Pediatr Orthop, 28:320-323.
Publisher | Google Scholor - Rolvien T, Amling M. (2022). Disuse Osteoporosis: Clinical and Mechanistic Insights. Calcif Tissue Int, 110(5):592-604.
Publisher | Google Scholor - Claes L, Recknagel S, Ignatius A. (2012). Fracture healing under healthy and inflammatory conditions. Nat Rev Rheumatol, 8:133-143
Publisher | Google Scholor - Bloomfield SA. (1997). Changes in musculoskeletal structure and function with prolonged bed rest. Med Sci Sports Exerc, 29:197-206.
Publisher | Google Scholor - Volpon jb, Cecim pes, Miyase ci, gava nf. (2008). O alendronato de sódio na prevenção da osteopenia secundária à imobilização gessada em ratas: avaliação histomorfométrica. Rev Bras Ortop, 43(10):442-451
Publisher | Google Scholor - LeBlanc AD, Driscol TB, Shackelford LC, Evans HJ, Rianon NJ et al. (2002). Alendronate as an effective countermeasure to disuse induced bone loss. J Musculoskelet Neuronal Interact, 2(4):335-343.
Publisher | Google Scholor - Mosekilde L, Thomsen JS, Mackey MS, Phipps RJ. (2000). Treatment with risedronate or alendronate prevents hind-limb immobilization-induced loss of bone density and strength in adult female rats. Bone, 27(5):639-645.
Publisher | Google Scholor - Akkari M, Santili C. (2003). Metabolismo do cálcio e do fósforo. In: Pardini Júnior AG, Souza JMG, Cunha LAM, editores. Clínica ortopédica. Rio de Janeiro: Medsi, 253-259
Publisher | Google Scholor - Cecim PES.(2007). Uso de alendronato de sódio em ratas submetidas à imobilização gessada. Análise de propriedades mecânicas do fêmur e da densidade óssea radiográfica do colo femoral. São Paulo: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo.
Publisher | Google Scholor - Claes L, Recknagel S, Ignatius A. (2012). Fracture healing under healthy and inflammatory conditions. Nat Rev Rheumatol, 8:133-143.
Publisher | Google Scholor - Kubiak EN, Beebe MJ, North K, Hitchcock R, Potter MQ . (2013). Early weight bearing after lower extremity fractures in adults. J Am Acad Orthop Surg, 21:727-738.
Publisher | Google Scholor - Rolvien T, Amling M. (2022). Disuse Osteoporosis: Clinical and Mechanistic Insights. Calcif Tissue Int, 110(5):592-604.
Publisher | Google Scholor - Rittweger J, Beller G, Armbrecht G, Mulder E, Buehring B, Gast U. et.al. (2010). Prevention of bone loss during 56 days of strict bed rest by side-alternating resistive vibration exercise. Bone. 46:137-147.
Publisher | Google Scholor - Oliveira LG, Carneiro MLRG, Souza MPG, Souza CG, Moraes FB, FL. Atualização do Tratamento Medicamentoso da Osteoporose. Rev Bras Ortop. 56(5):550-7, 2021.
Publisher | Google Scholor - Stolnick B, Oliveira LG. (2016). Para que a primeira fratura seja a última. Rev Bras Ortop, 51(02):121-126.
Publisher | Google Scholor - Freedman BA, Potter BK, Nesti LJ, Cho T, Kuklo TR. (2007). Missed opportunities in patients with osteoporosis and distal radius fractures. Clin Orthop Relat Res, 454(454):202-206.
Publisher | Google Scholor - Souza BGSE, Carvalho LGVA, Oliveira LFMM, Ferreira AG, Amaral RCSD. et.al. (2017). Primary and secondary osteoporotic fractures prophylaxis: evaluation of a prospective cohort. Rev Bras Ortop, 52(05):538-543.
Publisher | Google Scholor - Radominski SC, Bernardo W, Paula AP, Albergaria BH, Moreira C. Et.al. (2017). Diretrizes brasileiras para o diagnóstico e trata- mento da osteoporose em mulheres na pós-menopausa. Rev Bras Reumatol, 57(2):452-466.
Publisher | Google Scholor - Black DM, Rosen CJ. (2016). Clinical Practice. Postmenopausal Osteoporosis. N Engl J Med, 374(03):254-262.
Publisher | Google Scholor - De Souza MP. (2010). Osteoporosis Diagnosis and Treatment. Rev Bras Ortop, 45(03):220-229.
Publisher | Google Scholor - Stolnick B, Oliveira LG. (2016). Para que a primeira fratura seja a última. Rev Bras Ortop, 51(02):121-126.
Publisher | Google Scholor - Freedman BA, Potter BK, Nesti LJ, Cho T, Kuklo TR. (2007). Missed opportunities in patients with osteoporosis and distal radius fractures. Clin Orthop Relat Res, 454(454):202-206.
Publisher | Google Scholor - Souza BGSE, Carvalho LGVA, Oliveira LFMM, Ferreira AG, Amaral RCSD, Oliveira VM. (2017). Primary and secondary osteoporotic fractures prophylaxis: evaluation of a prospective cohort. Rev Bras Ortop, 52(05):538-543.
Publisher | Google Scholor - Radominski SC, Bernardo W, Paula AP, Albergaria BH, Moreira C, et.al. (2017). Diretrizes brasileiras para o diagnóstico e trata- mento da osteoporose em mulheres na pós-menopausa. Rev Bras Reumatol, 57(2):452-466.
Publisher | Google Scholor