Research Article
Determinants of Syphilis Among Pregnant Women Attending Antenatal Care Clinic at Public Hospital in South West Shoa, Ethiopia, Unmatched Case-Control Study, 2023
- Bacha Merga Chuko 1*
- Fikru Assefa Kibrat 1
- Zufela Sime Gari 2
- Ararso Tafese 3
- Teka Girma 4
- Shambal Negese Marami 5
- Gada Edea 6
1Department of maternity and neonatology, Ameya Primary Hospital, Waliso, Ethiopia.
2Department of Anesthesia, Waliso General Hospital, Waliso, Ethiopia.
3Departments of Midwifery, Waliso General Hospital, Waliso, Ethiopia.
4Department of Public Health, College of health sciences, Ambo University, Ambo, Ethiopia.
5Department of midwifery, College of health sciences, Metu University, Ethiopia.
6Department of Nursing, College of health sciences, Ambo University, Ambo, Ethiopia.
*Corresponding Author: Bacha Merga Chuko, Department of maternity and neonatology, Ameya Primary Hospital, Waliso, Ethiopia.
Citation: Chuko B M, Kibrat F A, Gari Z S, Tafese A, Girma T, et, al. (2024). Determinants of Syphilis Among Pregnant Women Attending Antenatal Care Clinic at Public Hospital in South West Shoa, Ethiopia, Unmatched Case-Control Study, 2023. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 4(2):1-11. DOI: 10.59657/2993-0871.brs.24.061
Copyright: © 2024 Bacha Merga Chuko, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 14, 2024 | Accepted: September 05, 2024 | Published: September 16, 2024
Abstract
Background: Syphilis is an infectious sexually transmitted disease caused by the Spirochete Treponema palladium. Untreated maternal syphilis causes adverse pregnancy outcomes such as spontaneous miscarriage, stillbirth, low birth weight, neonatal death, and congenital syphilis. There was a limited case control study to identify determinants of syphilis infections at the study area.
Objectives: The aim of this study is to identify determinants of syphilis among pregnant women attending ANC clinic at public hospital in South West Shoa, Ethiopia, 2023.
Methods: A facility based unmatched case- control study among 240(48 case and 192 control) with 1:4 ratios were conducted from March 10, 2023 – May 20, 2023 among pregnant women attending antenatal care follow at public hospital, South West Shoa. Cases were selected by Convenience and systematic sampling techniques were employed to select control and data was collected by using structured and pretested questionnaire. The collected data were entered into Epi info version 7.2.2 and exported to SPSS version 25 for analysis. Variable having p-value < 0.25 in the bi-variable analysis was entered into logistic regression model for multi variable analysis. Statistical significance was declared at p-value < 0.05. Adjusted odd ratio along with 95% confidence interval was used to show strength of association. The result was presented using text, table and graphs.
Results: In this study 235 women (47 cases and 188 controls) were completed the interview giving the response rate of 97.92%. After multivariable logistic regression analysis, significantly associated factors with Syphilis infection were status of current pregnancy [AOR = 2.697, 95% CI (1.003-7.249, ANC follow-up [AOR = 4.556, 95% CI (1.759-11.80)], history of STI [AOR = 3.080, 95% CI (1.347-7.043)], alcohol intake [AOR = 3.965, 95% CI (1.56-10.078)], age at started sexual intercourse at age [AOR = 8.951, 95% CI (3.70-21.646)] and multiple sexual partner [AOR = 2.754, 95% CI (1.065-7.118)].
Conclusion: Status of current Pregnancy, ANC follow-up, history of STI, alcohol intake, age started sexual intercourse, and multiple sexual partners were significantly associated determinants. Therefore, health care providers should focus on health education on these determinants, and strengthening necessary early diagnosis and treatment for STI.
Keywords: syphilis infection; pregnant women; public hospitals; South West Shoa Zone
Introduction
The term "sexually transmitted infection" refers to a pathogen that causes infection through sexual contact, whereas the word "sexually transmitted disease" refers to an identifiable clinical condition that has arisen from an infection [1]. Sexually transmitted infections are among the leading causes of sickness worldwide, with far-reaching health, social, and economic effects. Because of the quantity and possible difficulties of sexually transmitted illnesses, they are of public health relevance. They have a disproportionate impact on moms' health and social well-being by having a considerable impact on their reproductive capacity [2].
Untreated syphilis is a disease that lasts for many years and is classified into two stages: Early syphilis includes primary syphilis, secondary syphilis, and early latent syphilis, whereas late syphilis includes late latent syphilis and tertiary syphilis [3].
Adult syphilis symptoms vary according to stage. Signs and symptoms of the main stage include a single or multiple sores at the location where syphilis entered your body (initial stage of syphilis). Sores that are firm, round, and painless are prevalent (though not always). During the secondary stage, skin rashes and/or mucous membrane lesions, such as sores in your mouth, vagina, or anus, occurred. The absence of visible evidence or symptoms of syphilis characterizes the latent period. Tertiary syphilis is exceedingly serious and can appear 10-30 years after the initial infection. Tertiary syphilis damages internal organs and can result in death [4,5].
Syphilis has an average incubation period of 3 weeks (from exposure to the development of initial signs or symptoms), although it can be as little as 10 days or as long as 90 days. Serologic test results will stay negative during the incubation period, and the patient is not deemed infectious. However, without syphilis post-exposure treatment, those with incubating infection will develop primary syphilis lesions, a highly infectious stage of illness [5].
Sexually transmitted infections (STIs) are a major public health issue around the world, impacting quality of life and causing significant morbidity and mortality. Congenital syphilis imposed a significant morbidity and death burden [6]. Centers for Disease Control during 2012–2016, the number of reported cases of syphilis among pregnant increased 55%, from 9,551 to 14,838, and the number of cases among pregnant women increased 61%, from 1,561 to 2,508 [7]. The burden of syphilis among pregnant women in sub-Saharan Africa was 2.9%.Syphilis infection among pregnant women was increases in East and Southern African regions (3.2% ) [8]. In Ethiopia the magnitude of syphilis was ranged from 1.1-5.1% [9-12].
The findings of different study revealed that seems literature's multiple sexual partners, Previous history of abortion and previous history of STI, substance use , starting first sexual practice before the age of 18 years, sexual partners’ history of STI were risk factors of syphilis infection [11,13,14].
At any phase of syphilis infection, the infection can be transmitted to a fetus during pregnancy and can result in adverse pregnancy outcome or severe birth defects [6]. Syphilis continues to be a major cause of pregnancy loss and adverse pregnancy outcome among mothers who do not receive antenatal syphilis screening and treatment during pregnancy. Adverse pregnancy outcome such as stillbirths, and preterm were attributable to maternal syphilis [15]. Adverse pregnancy outcome like stillbirth, preterm birth ,and low birth weight were related with untreated maternal syphilis during pregnancy [16].
Mother-to-child transmission of syphilis (congenital syphilis) is frequently fatal to the fetus if maternal infection is not detected and treated early enough in pregnancy. The fetus can be easily treated with treatment, and the danger of poor effects to the fetus is negligible if the mothers receive adequate treatment throughout early pregnancy [17]. Early detection and treatment of syphilis in pregnant women is critical for treating the infection and minimizing adverse pregnancy outcomes such as fetal and neonatal death [6].
Ethiopia has remarkable progress in screening and treatment of STI like syphilis especially for pregnant women. Since mother to child transmission at birth is the most common way transmission of syphilis infection, identifying syphilis among pregnant women in the area is very important for the prevention of vertical transmission to the new born [2].
Despite the implementation of different guidelines to control STIs in Ethiopia, the burden of syphilis during pregnancy is persisting. Although some different studies were conducted in different parts of Ethiopia on syphilis infection among pregnant women, less common determinants were identified. This variation could be due to study design in which cross-sectional study design was usually used. But, there was a limited case control study on determinants of syphilis infection at study area. Therefore, this study was aimed to address this gap by using case control study design to identify determinants syphilis among pregnant women attending ANC at Public hospital, South West Shoa.
Methods
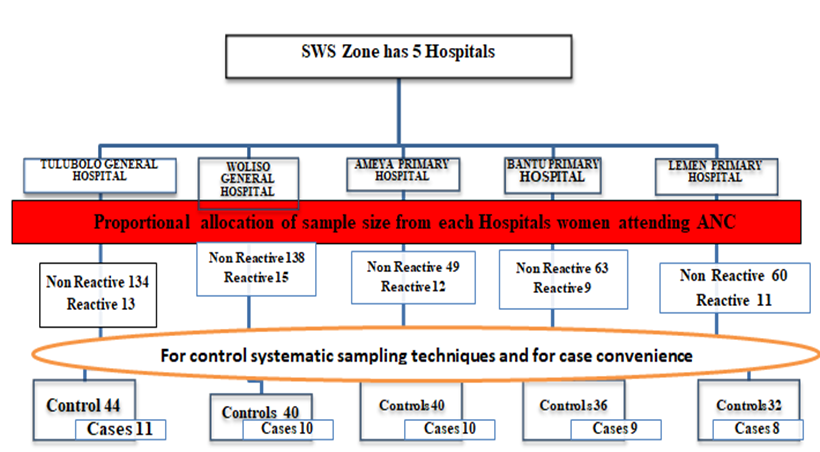
Study area and study period: The study was carried out at public hospitals in South West Shoa Zone, Oromia region, Ethiopia. Southwest Shoa Zone is 114 KM located to the south of Addis Ababa. Southwest Shoa Zone comprised five government hospitals named Tullu Bollo General Hospital, Waliso General Hospital, Ameya Primary Hospital, Bantu Primary Hospital, and Leman Primary Hospital, and one non-government hospital called Lukas Catholic Hospital which is found in Waliso, the capital city of the South West Shoa Zone. Last year's annual ANC reports were Tullu Bollo general hospital (882) from this 804 were no reactive and 78 were reactive, Woliso General Hospital (918) from this 824 were no reactive and 90 were reactive, Ameya primary hospital (366) from this 294 were no reactive and 72 were reactive, Bantu primary hospital (432) from this 378 were no reactive and 54 were reactive, and Leman primary hospital (420) from this 360 were no reactive and 66 were reactive.
Study period: The study was conducted in South West Shoa zone at five public hospitals from March 10, 2023 – May 10, 2023.
Study design: Institutional based unmatched case control study design was conducted
Source population: All pregnant women attending ANC at Public hospital in South West Shoa Zone
Study Population: Pregnant women those attending routine ANC follow up at South West Shoa zone five public hospitals and positive for syphilis tests at laboratory services while attending ANC during study period were case. Pregnant women those attending routine ANC follow up at South West Shoa zone five public hospitals and negative for syphilis tests at laboratory services while attending ANC during study period were control.
Inclusion Criteria: All pregnant mothers who attending ANC at Public hospital in South West Shoa Zone positive for syphilis tests during study period were included. Pregnant mothers who attending ANC at Public hospital in South West Shoa Zone and negative for syphilis tests during study period were included.
Exclusion criteria: Pregnant mothers who came for ANC whose cards not completely documented and others who were critically ill and unable to communicate were excluded from the study.
Sample Size Determination
Sample size was determined by using Open Epi info version 7.2.5 using double population proportion exposure difference formulas by considering major determinants of syphilis infection(history of multiple sexual partner, and alcohol use [18] and a history of sexually transmitted infections and used a substance [14] by considering CL=95%,p0wer 80% and ratio case to control was 4. The final sample size calculated after adding 10% of non- response rate was 236. But to make 1:4 proportion of case: control a total sample size of 240 was taken (48 cases and 192 controls).
Sampling Technique and Procedure
The number of study participants from each hospital was determined by proportional allocation to population size by using an average of two months last year`s ANC report taken from each hospital. To allocate Control sample size to each hospital an average of two months last year non-reactive for syphilis test reports was used., Then two month last year last year non-reactive for syphilis report of all hospitals (N) was divided by total sample size of control (n) to obtained the interval (K), K=N/n = 444/192= 2.3 ~2. The first study participant of control was determined by lottery methods. Then, by using a systematic random sampling method the data collectors were interviewed mothers every 2 daily until the required sample size was obtained and Case were selected by convenience sampling technique (all mothers who reactive for syphilis test was taken consecutively) until 48 samples was reached.
Figure 1:Proportional allocation of sample size from five South West Shoa zone Hospitals
Study variables
Dependent variable
Syphilis infection
Independent variable
Socio-demographic characteristics: - age, resident, marital status, occupational status and educational status
Obstetrics characteristics: Abortion, still birth, ANC, parity and multiple pregnancy
Lifestyle related factors: multiple partners, age at start sexual intercourse, substance usage and alcohol drink
Sexual transmitted disease history related factors: history of STI
Operational definition
Cases: are individuals who have the outcome of interest. Those who have syphilis infection in this study,
Controls: are individuals who do not have the outcome interest. Those who do not have syphilis infection in this study [19].
Data Collection instrument and Technique
A Structured questionnaire was adapted after reviewing different kinds of literature. The questionnaire consisted of 7 items of Socio-demographic characteristics, 9 items of Obstetrics related factors, and 3 items of medical history related factors, 6 items of Life style related factors and 2 items of serological test. Pregnant women’s on ANC follow up those tested and reactive for RPR Reagent were declared as positive for active syphilis and those nonreactive were negative for active syphilis (20). The questionnaires contain 5 parts and 27 items.
The data were collected using a pre-tested structured face-to-face interview questionnaire and chart review prepared by Afan Oromo. The data were collected by four BSc midwives who are fluent in the local language and supervised by two senior midwives.
Data Quality Control (Assurance)
To ensure the quality of tools, tools were adapted from related articles, pre-tested on 5% of the study participants at Holeta Primary Hospital. To ensure the consistency of the questionnaires, the English version was translated into Afan Oromo and again retranslated back to English by a language translator expert.
The data collectors and supervisors were recruited from out of the employee of the study hospitals to minimize bias and training was given for data collectors and supervisors regarding data collection procedure, tools, the purpose of study, and ethical consideration. Data collectors were strictly supervised. At the end of each day, the questionnaire was reviewed and checked for completeness by the supervisors, and a correction was made.
The collected data were checked for completeness, by the supervisors before data entry into the application and each questionnaire approved to enter the application for analysis were correctly coded, and given a specific Identification number. Data were entered into Epi info to minimize errors, to check double data entered and design skipping pattern. Outlier and missed data were checked before data analysis by exporting to SPSS version 25.
Data Processing and Analysis
The collected data was checked for completeness and consistency of the information obtained from the study participants. Then, the data was entered into the Epi info and exported to SPSS version 25 for analysis. Multi co-linearity was checked by using variance inflation factors, the maximum value variance inflation factors which was 1.47, which is by far lower than tolerable cut off point 10 and tolerance test was ranged 0.676-0.951. The goodness of fit (GOF) of the model was checked using Hosmer–Lermeshows GOF test. The p value of Hosmer –Lermeshows GOF test of our model is 0.78, which was support that the model was good fit.
Descriptive analysis (like frequencies, percentages, means, and standard deviation) and inferential analysis was done. The bivariate and multivariable logistic regression analysis was done. A p-values < 0>
Ethical Consideration
An ethical clearance letter was obtained from Ambo University College of Health Science Ethical Review committee by Ref. number AU/PGC/630/2015 on the date of 15/03/2023 and a supportive letter was obtained from the College of Health Science. Then, a permissions letter was obtained from the Zonal Health Bureau, South West Shoa Zone, and permissions for data collection were obtained from all hospitals. Verbal Informed consent from study participants before the interview was obtained. The study participant was informed about the purpose of the study and the importance of their participation in the study by contributing information that may help in assessing syphilis infection service. Also, the study participants were informed as they can skip questions or questions that they do not want to answer fully or partially and also to stop at any time if they want to do so. The interview was conducted in a separate area with protected privacy. After getting consent & their willingness to participate in the study, they were provided with the questionnaire and oriented on how to respond to the questions.
Results
A data was collected from 240 participants, and 235 women (47 cases and 188 controls) were completed the interview giving the response rate of 97.92% for both cases and controls.
Socio-Demographic characteristics of the respondents
Age of the respondents ranges from 16-36 years with mean age of 26.93 years (26.93+ 3.95) and 22 (46.8 %) of cases were between 24-29 and 78 (41.5%) of control were between 24-29. About greater than half of the cases 23 (49%) and 95 (50.5%) of controls had diploma and above educational status (see table 1).
Table 1: Socio-demographics characteristics of pregnant women attending ANC clinic at public hospital in South West Shoa, Ethiopia, 2023(n=235).
| Variable | Variable categories | Case N(%) | Control N (%) | Total N (%) |
| Age | <=24 | 15 (31.9) | 61 (32.4) | 76 (32.34) |
| 24-29 | 22 (46.8) | 78 (41.5) | 100 (42.55) | |
| 30-35 | 6 (12.8) | 9 (4.8) | 15 (6.38) | |
| >35 | 4 (8.5) | 40 (21.3) | 44 (18.73) | |
| Resident | Urban | 27 (57.4) | 107 (56.9) | 134 (57.02) |
| Rural | 20 (42.6) | 81 (43.1) | 101 (42.98) | |
| Marital status | Single | 3 (1.6) | 1 (2.1) | 4 (1.70) |
| Married | 174 (92.6) | 31 (66.0) | 205 (87.23) | |
| Divorced | 6 (3.2) | 6 (12.8) | 12 (5.12) | |
| Widowed | 5 (2.7) | 9 (19.1) | 14 (5.95) | |
| Educational status | no formal education | 9 (19.1) | 11 (5.9) | 20 (8.51) |
| Primary education | 6 (12.8) | 24 (12.8) | 30 (12.77) | |
| Secondary education | 9 (19.1) | 58 (30.9) | 67 (28.51) | |
| Diploma and above | 23 (49) | 95 (50.5) | 118 (50.21) | |
| Husband educational status | No formal education | 4 (8.5) | 10 (5.3) | 14 (5.96) |
| Primary education | 18 (38.3) | 73 (38.8) | 91 (38.72) | |
| Secondary education | 15 (31.9) | 58 (30.9) | 73 (31.06) | |
| Diploma and above | 10 (21.3) | 47 (25) | 57 (24.26) | |
| Occupational Status | Housewife | 26 (55.3) | 92 (48.9) | 118 (50.21) |
| Farmer | 1 (2.1) | 3 (1.6) | 4 (17.39) | |
| Merchant | 9 (19.1) | 37 (19.7) | 46 (19.57) | |
| Government employee | 11 (23.4) | 39 (20.7) | 50 (21.28) | |
| Self-Employee | 0 (0.0) | 17 (9) | 17 (7.23) | |
| Husband occupational Status | Farmer | 33 (17.6) | 14 (29.8) | 47 (20) |
| Merchant | 66 (35.1) | 12 (25.5) | 78 (33.19) | |
| Government employee | 54 (28.7) | 10 (21.3) | 64 (27.23) | |
| Self-Employee | 35 (18.6) | 1 1(23.4) | 46 (19.57) |
Obstetrics characteristics of the respondents
From respondents, 37 (78.7%) of cases and 141 (75%) controls were multiparous while 10 (21.3%) of cases and 47 (25%) of controls were multigravida. Among 235 women, 34 (72.3%) of cases and 166 (88.3%) of controls were planned their current pregnancy. Among cases, 17(36.2%) were had history of still birth and among control 38 (20.2%) were had history of still birth. About 150 (79.8%) of controls and 30(63.8) cases were had no history of still birth (see table 2).
Table 2: Obstetrics characteristics of pregnant women attending ANC clinic at public hospital in South West Shoa, Ethiopia, 2023 (n=235).
| Variable | Variable categories | Case N(%) | Control N (%) | Total |
| Parity | Primiparous | 10 (21.3) | 47 (25.0) | 57(24.26) |
| Multiparous | 37 (78.7) | 141 (75.0) | 178 (75.74) | |
| Previous history of multiple pregnancy | Yes | 30 (63.8) | 150 (79.8) | 180 (76.59) |
| No | 17 (36.2) | 38 (20.2) | 55 (23.40) | |
| Status of current Pregnancy | Planned | 34 (72.3) | 166 (88.3) | 200 (85.11) |
| Unplanned | 13 (27.7) | 22 (11.7) | 35 (14.89) | |
| ANC follow-up | Yes | 31 (66.0) | 159 (84.6) | 190 (80.85) |
| No | 16 (34.0) | 29 (15.4) | 45 (19.15) | |
| Number visit | First visit | 16 (36.4) | 34 (21.7) | 50 (21.28) |
| Second visit | 16 (36.4) | 82 (52.2) | 98 (41.70) | |
| Third visit | 9 (20.5) | 20 (12.7) | 29(12.34) | |
| Fourth visit | 3 (6.8) | 21 (13.4) | 24 (10.21) | |
| History of abortion | Yes | 36 (76.6) | 110 (58.5) | 146(62.12) |
| No | 11 (23.4) | 78 (41.5) | 89 (37.87) | |
| Still birth | Yes | 17 (36.2) | 38 (20.2) | 55 (23.40) |
| No | 30 (63.8) | 150 (79.8) | 180 (76.59) | |
| Neonatal death | Yes | 0 (0.0) | 10 (5.3) | 10 (4.26) |
| No | 47 (100.0) | 178 (94.7) | 225(95.74) |
Sexual transmitted disease history related factors
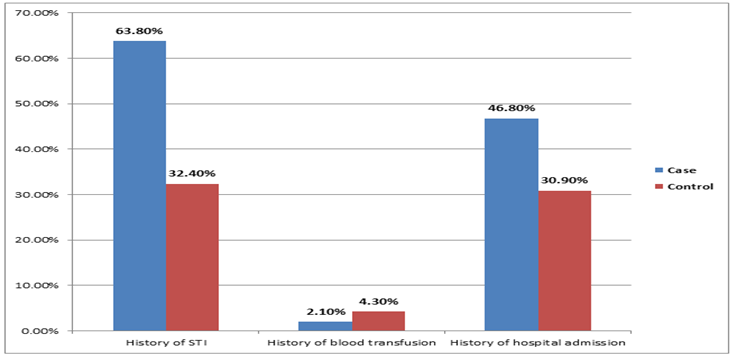
Based on the result of the study, more than of cases 30 (63.8%) and 61(32.4) among controls had history of STI, while 17(36.2) and 127 (67.6%) among cases and controls were had no history of sexual transmitted infection respectively. From history of hospital admission more than half of case 25 (53.2%) and controls 130 (69.1%) had no history of hospital admission (Figure 2).
Figure 2:Sexual transmitted disease history of pregnant women attending ANC clinic at public hospital in South West Shoa, Ethiopia, 2023.
Lifestyle related Factors
The study revealed that 16 (34%) of pregnant women with cases and 34(18.1%) among controls were drunk alcohol during pregnancy, while 31 (66%) cases and 154 (81.9%) women with controls were no alcohol drink. More than two third of cases 32 (68.1%) were started sexual intercourse before 18 years old and one fourth of control 47 (25%) were started sexual intercourse before 18 years old. Regarding history of multiple sexual inter course, more than one third of cases 17 (36.2%) and most of controls 161 (85.6%) had no history of multiple sexual inter course (Table 3).
Table 3:Lifestyle of pregnant women attending ANC clinic at public hospital in South West Shoa, Ethiopia, 2023 (n=235).
| Variable | Variable categories | Case N (%) | Control N(%) | Total |
| Alcohol | Yes | 16 (34.0) | 34 (18.1) | 50 (21.28) |
| No | 31 (66.0) | 154 (81.9) | 185 (78.72) | |
| partner alcohol | Yes | 24 (51.1) | 56 (29.8) | 80 (34.04) |
| No | 23 (48.9) | 132 (70.2) | 155 (65.96) | |
| Addictive substance | Yes | 16 (34.0) | 34 (18.1) | 50 (21.28) |
| No | 31 (66.0) | 154 (81.9) | 185 (78.72) | |
| Age started sexual intercourse | <18> | 32 (68.1) | 47 (25.0) | 79 (33.62) |
| >18 | 15 (31.9) | 141 (75.0) | 166 (70.64) | |
| Multiple partner | Yes | 17 (36.2) | 27 (14.4) | 44 (18.72) |
| No | 30 (63.8) | 161(85.6) | 191(81.28) | |
| Multiple partners within last three months | Yes | 2 (4.3) | 3 (1.6) | 5 (2.13) |
| No | 45 (95.7) | 185 (98.4) | 230 (97.87) | |
| History of Coerce sexual intercourse | Yes | 1 (2.1) | 3 (1.6) | 4 (1.71) |
| No | 46 (97.9) | 185 (98.4) | 231 (98.29) | |
| HIV test results | Yes | 5 (10.6) | 6 (3.2) | 11 (4.68) |
| No | 42 (89.4) | 182 (96.8) | 224 (95.32) |
Bivariable binary logistic regression analysis of factors associated with syphilis infection. There were about 14 candidate variables in bivariate analysis model with p-value of less than 0.25. These were: educational status, previous history of multiple pregnancy, Status of current Pregnancy, ANC follow-up, history of abortion, still birth, history of STI, history of hospital admission, alcohol intake history, partner alcohol intake, using addictive substance, age started sexual intercourse, multiple sexual inter course and maternal HIV co-infection were identified as candidate variables for multivariable logistic regression analysis. Then those the above variables were entered into multivariable logistic regression for analysis (see table 4).
Table 4: Binary logistics regression of pregnant women attending ANC clinic at public hospital in South West Shoa, Ethiopia, 2023 (n=235).
| Variables | Variables Category | Case N (%) | Control N (%) | COR 95% CI | P-value |
| Educational status | No formal education | 9(19.1) | 11(5.9) | 3.379(1.25-1.254) | 0.016 |
| Primary education | 6(12.8) | 24(12.8) | 1.033(0.38-2.82) | 0.950 | |
| Secondary education | 9(19.1) | 58(30.9) | 0.641(.28-1.48) | 0.298 | |
| Diploma and above | 23(49) | 95(50.5) | 1 | ||
| Previous history of pregnancy | Yes | 30(63.8) | 150(79.8) | 1 | |
| No | 17(36.2) | 38(20.2) | 2.237(1.12-4.48) | 0.023 | |
| Status of current Pregnancy | Planned | 34(72.3) | 166(88.3) | 1 | |
| Unplanned | 13(27.7) | 22(11.7) | 2.885(1.32-6.29) | 0.008 | |
| ANC follow-up | Yes | 31(66.0) | 159(84.6) | 1 | |
| No | 16(34.0) | 29(15.4) | 2.830(1.38-5.82) | 0.005 | |
| History of abortion Status | Yes | 36(76.6) | 110(58.5) | 2.321(1.11-4.84) | 0.025 |
| No | 11(23.4) | 78(41.5) | 1 | ||
| Still birth | Yes | 17(36.2) | 38(20.2) | 2.237(1.12-4.48) | 0.023 |
| No | 30(63.8) | 150(79.8) | 1 | ||
| History of STI | Yes | 30(63.8) | 61(32.4) | 3.674(1.88-7.17) | 0.000 |
| No | 17(36.2) | 127(67.6) | 1 | ||
| History of hospital admission | Yes | 22(46.8) | 58(30.9) | 1.972(1.023-3.78) | 0.041 |
| No | 25(53.2) | 130(69.1) | 1 | ||
| Alcohol | Yes | 16(34.0) | 34(18.1) | 2.338(1.15-4.75) | 0.019 |
| No | 31(66.0) | 154(81.9) | 1 | ||
| partner alcohol | Yes | 24(51.1) | 56(29.8) | 2.460(1.28-4.72) | 0.007 |
| No | 23(48.9) | 132(70.2) | 1 | ||
| Addictive substance | Yes | 16(34.0) | 34(18.1) | 2.338(1.15-4.75) | 0.019 |
| No | 31(66.0) | 154(81.9) | 1 | ||
| Age started sexual intercourse | <18> | 32(68.1) | 47(25.0) | 6.40(3.19-12.84) | 0.000 |
| >18 | 15(31.9) | 141(75.0) | 1 | ||
| Multiple partner | Yes | 17(36.2) | 27(14.4) | 3.379(1.64-6.95) | 0.001 |
| No | 30(63.8) | 161(85.6) | 1 | ||
| HIV test results | Yes | 5(10.6) | 6(3.2) | 3.611(1.05-12.46) | 0.041 |
| No | 42(89.4) | 182(96.8) | 1 |
Key: - *= statistically significant,1= Reference COR= Crude odd ratio, AOR= Adjusted odd ratio, CI= confidence interval
Multiple binary logistics regression analysis of factors associated with syphilis infection
After variables having p-value of less than 0.25 entered into multivariable analysis, variables significantly associated with syphilis infection were Status of current Pregnancy, ANC follow-up, history of STI, alcohol intake history, age started sexual intercourse, and multiple sexual partners.
According to this study, the odds of syphilis infection were 2.697 times higher in pregnant women than unplanned their current pregnancy [AOR = 2.697, 95% CI (1.003-7.249)]. The odds of syphilis infection were 4.556 times more likely among pregnant women who had no ANC follow-up than pregnant women who had ANC follow-up [AOR = 4.556, 95% CI (1.759-11.80)]. The odds of syphilis infection were 3.080 times higher in pregnant women who had history of STI [AOR = 3.080, 95% CI (1.347-7.043)].
Similarly, the odds of syphilis infection were 3.965 times higher among pregnant women who were drunk alcohol than pregnant women who were no drunk alcohol [AOR = 3.965, 95% CI (1.56-10.078)]. Likewise, pregnant women who were started sexual intercourse at age less than 18 years old were 8.951 times more likely to have syphilis infection than women who were started sexual intercourse at age greater than 18 years old [AOR = 8.951, 95% CI (3.70-21.646)]. In addition, the odds of syphilis infection were 2.754 times higher in pregnant women were multiple sexual inter course [AOR = 2.754, 95% CI (1.065-7.118)] (see table 5).
Table 5: Multiple logistics regression of pregnant women attending ANC clinic at public hospital in South West Shoa, Ethiopia, 2023 (n=235).
| Variables | Variables Category | Case N (%) | Control N (%) | COR95%CI | AOR 95% CI | P value |
| Previous history of multiple pregnancy | Yes | 30(63.8) | 150(79.8) | 1 | 1 | |
| No | 17(36.2) | 38(20.2) | 2.237(1.12-4.48) | 2.229(0.91-5.47) | 0.080 | |
| Status of current Pregnancy | Planned | 34(72.3) | 166(88.3) | 1 | 1 | |
| Unplanned | 13(27.7) | 22(11.7) | 2.885(1.32-6.29) | 2.697(1.03-7.25) | 0.049* | |
| ANC follow-up | Yes | 31(66.0) | 159(84.6) | 1 | 1 | |
| No | 16(34.0) | 29(15.4) | 2.830(1.38-5.82) | 4.556(1.76-11.80) | 0.002* | |
| History of abortion | Yes | 36(76.6) | 110(58.5) | 2.32(1.11-4.84) | 2.22(0.87-5.65) | 0.096 |
| No | 11(23.4) | 78(41.5) | 1 | 1 | ||
| History of STI | Yes | 30(63.8) | 61(32.4) | 3.67(1.88-7.17) | 3.08(1.35-7.04) | 0.008* |
| No | 17(36.2) | 127(67.6) | 1 | 1 | ||
| History of hospital admission | Yes | 22(46.8) | 58(30.9) | 1.97(1.023-3.78) | 2.31(0.98-5.40) | 0.054 |
| No | 25(53.2) | 130(69.1) | 1 | 1 | ||
| Alcohol | Yes | 16(34.0) | 34(18.1) | 2.34(1.15-4.75) | 3.96(1.56-10.08) | 0.004* |
| No | 31(66.0) | 154(81.9) | 1 | 1 | ||
| Age started sexual intercourse | <18> | 32(68.1) | 47(25.0) | 6.40(3.19-12.84) | 8.95(3.70-21.65) | 0.001** |
| >18 | 15(31.9) | 141(75.0) | 1 | 1 | ||
| Multiple sexual inter course | Yes | 17(36.2) | 27(14.4) | 3.38(1.64-6.95) | 2.75(1.07-7.12) | 0.037* |
| No | 30(63.8) | 161(85.6) | 1 | 1 |
Key: - *= statistically significant, **= strongly statistically significant ,1= Reference COR= Crude odd ratio, AOR= Adjusted odd ratio, CI= confidence interval
Discussion
This study has attempted to look at the determinants of syphilis infection among pregnant women attending ANC by incorporating as many as risk factors as possible in order to reduce risks and complication related to syphilis infection by preventing these determinant factors.
The study identified that, Status of current Pregnancy, ANC follow-up, history of STI, alcohol intake history, age started sexual intercourse, and multiple sexual inter course were significantly associated determinant factors with syphilis infection among pregnant women attending ANC at public hospital of South West Shoa, Zone.
According to this study, having history of STI was more likely to have syphilis infection compared to pregnant women who had no STI. This study was comparable to the study conducted in hospitals of Wolaita zone, Southern Ethiopia which revealed that pregnant women who had STI were more likely to develop syphilis infection than those who had no STI [14]. This is may be due to the fact that both STI and syphilis infection can be transmitted through unprotected sexual contact and women with current or past STI are at high risk for syphilis infection. However, this study was not supported by previously conducted in Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia [11],
This study identified that; pregnant women who had no ANC follow up had higher odds of syphilis infection than who had ANC follow up. It was supported by study conducted in west Arsi zone, Ethiopia [21]. This could be due to the fact that women who had no ANC follow up may be became pregnant without planning or by unsafe sexual intercourse.
Additionally, the finding of this study showed that alcohol intake was the determinant of syphilis infection. Pregnant women who were alcohol drunk were more likely to have syphilis infection than women who had alcohol drunk. This was similar to the previous study conducted Jinka town public health facilities, Southern Ethiopia [19]. This may be due to the fact that alcohol consumption exposes the women for unsafe sexual practice.
Furthermore, this study also showed that women who had started sexual intercourse at age of less than 18 years old were higher to have syphilis infection than who had started sexual intercourse at age of greater than 18 years old. This was supported by study done in Dilla University Referral Hospital, Ethiopia [13]. This might be due to the sociocultural status for early marriage of women or the earlier the onset of sexual life, the greater chance of having many sexual partners that increase vulnerability for syphilis infections.
The present study revealed that women who had multiple sexual inter course had higher odds to be infected with syphilis than women who had no multiple sexual inter course. This finding was similar with the study carried in Dilla University Referral Hospital, Ethiopia [13] and Jimma University Specialized Hospital, Ethiopia [22]. This might be a result of the nature of the disease is asymptomatic in most of the cases and the partners might not seek treatment for the infections. Therefore, if there is unprotected sex, the chance of acquiring the diseases is higher.
The finding of current study showed that pregnant women who were unplanned their current pregnancy had higher odds of syphilis infection than women who had planned their current pregnancy. This might be as a result of women who had unplanned pregnancy may be became pregnant by unsafe sexual intercourse which expose them to sexually transmitted infection like syphilis.
Conclusion
Syphilis infection is a significant public health concern that is linked with multiple factors. The findings of this study suggested that, Status of current Pregnancy, ANC follow-up, history of STI, alcohol intake, age started sexual intercourse, and multiple sexual inter course were significantly associated determinants with Syphilis infection among pregnant women attending ANC at Public hospital, South West Shoa. Identifying these factors is significant for reduction of new Syphilis infection by preventing these determinant factors. Health Facility (Hospitals), strengthening routine laboratory testing of Syphilis infection in all pregnant women attending ANC and treatment to prevent new Syphilis infections. Screening and treatment of symptomatic and asymptomatic STI in all pregnant women in accordance with guideline will be encouraged. Health care workers provide community health education on risk factors of Syphilis infections like alcohol intake, age at started sexual intercourse, and multiple sexual inter course. Professionals who are working at antenatal care services should be adhered to routine investigation of Syphilis infections diagnosis and early treatment. Special attention to the pregnant mother with history of STI, alcohol intake, started sexual intercourse before 18 years old and multiple sexual inter course. For mothers’ abstinence from alcohol intake and multiple sexual inter course. Plan their future pregnancy. Furthermore, they would need to prevent STI and seek prompt medical help if positive for any STI. What already known on this topic. Magnitude of syphilis infection among pregnant women. This study adds. Identify determinant of syphilis infection among pregnant women. Identify reason of why pregnant women infected by syphilis infection.
Abbreviation and Acronym
ANC; Antenatal Care. AOR; Adjusted Odds Ratio, CI;Confidence Interval, COR;Crude Odds Ratio, SPSS;Statistical Package for the Social Sciences, STI;Sexually Transmitted Infections nad VDRL; Venereal Disease Research Laboratory test.
Declarations
Funding
There is no fund
Declaration of Conflict of Interest
Authors declare no conflict-of-interest respect to this study.
Data availability
The corresponding author is willing to provide the dataset that was used in this study based upon reasonable request using.
Author contribution
All the authors contributed to the proposal development, questionnaires, and data collecting process, analysis, and interpretation.
Data curation by: Bacha Merga Chuko, Fikru Assefa Kibrat, Taka Girma, Zufela Sime Gari and Ararso Tafese.
Format analysis
Bacha Merga Chuko, Fikru Assefa Kibrat, and Ararso Tafese, Gada Edea and Shambel Negese Marami.
Investigation
Bacha Merga Chuko, Fikru Assefa Kibrat, Taka Girma, Zufela Sime Gari, Ararso Tafese, Gada Edea and Shambel Negese Marami.
Methodology
Bacha Merga Chuko, Fikru Assefa Kibrat, Ararso Tafese, Gada Edea and Shambel Negese Marami.
Revise the manuscript
Bacha Merga Chuko, Fikru Assefa Kibrat, Taka Girma, Zufela Sime Gari and Shambel Negese Marami.
Final version of the article was checked by all authors.
Consent
Informed consent was taken from every study participant before the actual data collection started.
Acknowledgments
We would like to thank Ambo University, college of health science, Department of Public health for funding and data collectors for their contribution to accomplishing this research
References
- Control D. (2002). Sexually transmitted diseases treatment guidelines 2002. Centers for Disease Control and Prevention, 51:1-78.
Publisher | Google Scholor - MOH. (2015). National guidelines for the management of sexually transmitted infections using syndromic approach. Fed Minist Heal.
Publisher | Google Scholor - W H O giudeline. (2016). who guidelines for the Treatment of Treponema pallidum (syphilis).
Publisher | Google Scholor - (2016). CDC. Syphilis - CDC fact sheet. 2.
Publisher | Google Scholor - New T, City Y, Hygiene M, Transmitted S. (2019). The Diagnosis, Management and Prevention of Syphilis an Update and Review.
Publisher | Google Scholor - All AMA. (2018). Screening for Syphilis in Pregnant Women. 320(9).
Publisher | Google Scholor - Trivedi S, Williams C, Torrone E, Kidd S. (2019). National Trends and Reported Risk Factors among Pregnant Women with Syphilis in the United States, 2012-2016. Obstet Gynecol, 133(1):27-32.
Publisher | Google Scholor - Hussen S. (2019). Prevalence of Syphilis among Pregnant Women in Sub-Saharan Africa: A Systematic Review and Meta-Analysis.
Publisher | Google Scholor - E Kebede, B Chamso. (2000). Prevalence of Syphilis in Pregnancy in Addis Ababa. 77(4):212-216.
Publisher | Google Scholor - Fikadu B, Gebrish S, Asfaw T. (2019). Sero-Prevalence of Syphilis among Pregnant Women Attending Antenatal Careclinic at Jimma Univeristy Specialized Hospital. 5(1):28-31.
Publisher | Google Scholor - Tareke K, Munshea A, Nibret E. (2019). Seroprevalence of syphilis and its risk factors among pregnant women attending antenatal care at Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia : a cross ‑ sectional study. BMC Res Notes, 1-7.
Publisher | Google Scholor - Azeze B, Fantahun M, Kidan KG, Haile T. (1995). Seroprevalence of syphilis amongst pregnant women attending antenatal clinics in a rural hospital in north west Ethiopia. 347-350.
Publisher | Google Scholor - Hailu K, Gebretsadik A. (2020). Determinants of gonorrhea and syphilis infections among pregnant women attending antenatal clinic at Dilla University Referral Hospital, Ethiopia: Unmatched case-control study.
Publisher | Google Scholor - Lendado TA, Tekle T, Dawit D, Daga WB, Diro CW, Arba MA, et al. (2022). Determinants of syphilis infection among pregnant women attending antenatal care in hospitals of Wolaita zone, Southern Ethiopia. 1-13.
Publisher | Google Scholor - Watson-jones D, Changalucha J, Gumodoka B, Weiss H, Rusizoka M, Ndeki L, et al. (2022). Syphilis in Pregnancy in Tanzania. I. Impact of Maternal Syphilis on Outcome of Pregnancy. 940-947.
Publisher | Google Scholor - Wan Z, Zhang H, Xu H, Hu Y, Tan C, Tao Y. (2020). Maternal syphilis treatment and pregnancy outcomes: a retrospective study in Jiangxi. 1-8.
Publisher | Google Scholor - (2017). W H O Guideline on Syphilis screening and treatment for pregnant women.
Publisher | Google Scholor - Enbiale M, Id AG, Haile F, Tekabe B. (2021). Magnitude of syphilis sero-status and associated factors among pregnant women attending antenatal care in Jinka town public.1-12.
Publisher | Google Scholor - Gutema GL, Abeya SG, Ayele GA. (2020). Determinants of Syphilis Infection among Women Seeking Antenatal Care and Delivery Services in Olenchity Primary Hospital: A Case-Control Study. 3(1):8-14.
Publisher | Google Scholor - Andres F. Henao-Martinez S c. J. (2022). Diagnostic test for syphilis new test and new algorithms. Neurolgy Cinical Pract, 4(2):114-122.
Publisher | Google Scholor - Wubete M, Mohammed M, Mengistu M, Mekonnen R. (2019). Prevalence of syphilis among pregnant women attending antenatal clinic of Bulchana Health Center, Shashemene, West Arsi Zone, Ethiopia. 3(2):2-4.
Publisher | Google Scholor - B. Fikadu, S. Gebrish and TA. (2019). “Sero-prevalence of syphilis among pregnant women attending Antenatal Care Clinic at Jimma Univeristy specialized Hospital, Ethiopia,” Journal of Medicine and Medical Sciences. Journa Med Med Sci, 1-5.
Publisher | Google Scholor