Research Article
Determinants of Pre-Cervical Cancer Among Women Aged 30–49 Years Screened for Cervical Cancer at Health Facilities in the Woliso Town, Oromia, Ethiopia, 2022: A Case-Control Study
1Department of Midwifery, Institute of Health, Bule Hora University, Bule Hora, Oromia, Ethiopia.
2Department of Public Health, Woliso Hospital, Oromia, Ethiopia.
3Department of Public Health, College of Medicine and Health Science, Ambo University, Oromia, Ethiopia.
*Corresponding Author: Gudeta Haile Areri, Department of Midwifery, Institute of Health, Bule Hora University, Bule Hora, Oromia, Ethiopia.
Citation: Gudeta H. Areri, Berhanu B. Geleta, Mulatu Ayana M. (2024). Determinants of Pre-Cervical Cancer Among Women Aged 30–49 Years Screened for Cervical Cancer at Health Facilities in the Woliso Town, Oromia, Ethiopia, 2022: A Case-Control Study. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(6):1-10. DOI: 10.59657/2993-0871.brs.24.051
Copyright: © 2024 Gudeta Haile Areri, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 12, 2024 | Accepted: July 25, 2024 | Published: August 08, 2024
Abstract
Background: Pre-cervical cancers are identified as changes to cervical cells, making them more likely to develop into cancer. Cervical cancer is a potentially preventable and curable health problem at the pre-cancer stage. A review of documents and administrative reports showed that paracervical cancer is a major health problem in women. Hence, this study aimed to fill gaps in the literature by identifying the determinants of pre-cervical cancer among women aged 30–49 years in the study area.
Purpose: To identify the determinants of pre-cervical cancer among women aged 30–49 years screened for cervical cancer at health facilities in Woliso Town, Oromia, Ethiopia in 2022.
Patients and Methods: A facility-based unmatched case-control study design was conducted at health facilities in Oromia from December 1, 2021, to January 10, 2022. A total of 480 documents of study participants (120 patients and 360 controls) were included in this study. A simple random sampling method was used to select documents from the study participants. A data extraction checklist was used to collect necessary information about the women from the register and history card. Data were analyzed using a binary logistic regression model. The 95% confidence intervals (CI) with adjusted odds ratios (ORs) were computed to identify the presence and strength of the association. Statistical significance was declared at p < 0.05, along with the 95% CI of the adjusted odds ratio (AOR).
Results: Being a rural resident (AOR = 2.44, 95% CI = 1.55–3.85), age at menarche ≤12 years (AOR = 2.83, 95% CI = 1.25–6.39), use of oral contraceptive pills (OCP) (AOR = 1.83, 95% CI = 1.03–3.25), history of genital ulcers (AOR = 3.86, 95% CI = 1.12–13.31), being HIV positive (AOR = 2.55, 95% CI = 1.34–4.88), and a family history of cancer (AOR = 3.87, 95% CI = 1.47–10.21) were variables that were significantly associated with pre-cervical cancer.
Conclusion: Rural residence, age at menarche ≤12 years, use of oral contraceptive pills, a history of genital ulcers, being HIV positive, and a family history of cancer were determinants of pre-cervical cancer among women aged 30-49 years.
Keywords: pre-cancerous cervical lesion; VIA positive; factors associated with pre-cervical cancer; cervical cancer screening; woliso town; Ethiopia
Introduction
Pre-cervical cancer precedes the development of invasive cervical cancer by 10–20 years, making it preventable if it is detected and effectively treated. Because of this long pre-cancerous period, cervical cancer rarely develops in women aged <30>
With its high incidence and mortality per year, cervical cancer continues to be a major public health problem, ranking as the fourth most common cause of cancer incidence and mortality in women worldwide, particularly in middle-aged women. However, most cervical cancers and related mortalities can be prevented by vaccination, screening, and treatment at the pre-cervical cancer stage [4, 7]. Therefore, it is important for all women, especially those aged 30–49 years, to undergo a gynecological examination and a test to determine if they have pre-cervical cancer [8]. Although pre-cervical cancer is potentially preventable and curable, cervical cancer remains one of the most common causes of cancer-related mortality in women worldwide. Globally, the annual number of new cases of cervical cancer is projected to increase from 570,000 to 700,000 between 2018 and 2030, and the annual number of deaths is projected to increase from 311,000 to 400,000. All countries are affected, but in developing countries its incidence is nearly twice as high and its mortality rate is three times higher than that in developed countries [9,10]. The burden of pre-cervical cancer varies between countries. According to a study in Venezuela, the magnitude of pre-cervical cancer was 10% [11], whereas it was 5.9% in Rwanda [12] and 3.7% in Ghana [13]. In Ethiopia, the trends in cervical cancer show that the number of cases generally increases from year to year, even though there is a difference in regional distribution. Addis Ababa, Oromia, and Amhara had a higher proportion of patients with cervical cancer, according to a study covering 16 years [14]. Studies in Eastern Ethiopia, Southern Ethiopia, and Addis Ababa revealed prevalences of 18.5% [15], 27.7%, [16] and 14% [17] of pre-cervical cancer among screened women. Owing to the increasing prevalence of pre-cervical and cervical cancers, the Federal Ministry of Health (FMOH) has developed guidelines for cervical cancer prevention and control in Ethiopia. These guidelines include primary, secondary, and tertiary prevention [18]. Therefore, it is important to identify the determinants of pre-cervical cancer and link them with the level of prevention to decrease the magnitude of the problem.
Studies have revealed various factors that are associated with pre-cervical cancer. Accordingly, lower levels of education [19, 20], advanced age [21], being a rural resident [22], and early age at marriage [23] were socio-demographic factors associated with pre-cervical cancer. In addition, using oral contraceptive pills [20, 24], being multiparous [21], being HIV positive, [17, 25] and having a history of STI [20,26–28] were some of the factors revealed by previous studies. In the study area, a review of documents and administrative reports of health facilities showed that pre-cervical cancer is among the major health problems in the female population. From a review of documents, the estimated magnitude of pre-cervical cancer among the screened women was approximately 6.6%. However, there is inadequate information on the determinants of pre-cervical cancer among women aged 30–49 years in the study area. The rationale of this study is to provide updated evidence on the determinants of pre-cervical cancer among women aged 30–49 years. The findings of this study may be helpful for local healthcare planners and other stakeholders as baseline information for planning the determinants of pre-cervical cancer in the area. In addition, the results obtained from this study provide baseline information and directions for further research in this area.
Methods
Study Area and Period
This study was conducted in public health facilities located in Woliso Town, Oromia Regional State, from December 1, 2021, to January 10, 2022. The study included documents of women aged 30–49 years screened for cervical cancer at health facilities in Woliso Town, which is located 114 km southwest from Addis Ababa, between July 2016 and June 2021. In 2021, the town had a total population of 64,681, of which 32,017 were females. The estimated number of women aged 30–49 years in the town was approximately 7,950 [29]. Among the health facilities located in the town, three facilities are currently providing cervical cancer screening and treatment. These included St. Luke Hospital, Woliso Town HC No. 1, and Woliso Town HC No.2. Screening for cervical cancer was initiated at three health facilities in 2015. In the past 5 years, approximately 4,331 women were screened, of whom 285 (6.6%) were VIA positive [29].
Study Design: A facility-based unmatched case-control study design was conducted.
Source population: The source populations for this study were all women who had been screened for cervical cancer at health facilities in Woliso Town in the last 5 years.
Study Population: The study population included women aged 30–49 years who were screened for cervical cancer at health facilities in Woliso Town within the last 5 years and had a VIA positive result (cases), and women aged 30–49 years who were screened for cervical cancer at health facilities in Woliso Town within the last 5 years and had a VIA negative result (controls).
Inclusion and Exclusion criteria
Inclusion Criteria for cases: Women aged 30–49 years screened for cervical cancer and registered as VIA-positive at health facilities in Woliso Town between July 2016 and June 2021 were included in the study. In addition, women registered as VIA-negative on the first screening and VIA-positive on follow-up screening within the above period were included.
Inclusion Criteria for controls: Women aged 30–49 years screened for cervical cancer and registered as VIA-negative at health facilities in Woliso Town between July 2016 and June 2021 were included in the study.
Exclusion Criteria for cases: Cases in registers with incomplete records of study variables were excluded from the study. this study did not include women whose VIA screening results were registered as uncertain or unclear.
Exclusion Criteria for controls: Controls with incomplete records of study variables were excluded from the study.
Sample Size and Sampling Technique
Sample Size determination
The sample size was determined using the Epi info 7 by considering a confidence level of 95%, power of 80%, and ratio of controls to cases of 3:1. The sample size was calculated using variables from previous studies and a variable with a larger sample size was selected for sample size determination. These variables were parity ≥4, history of STI, and HIV status of the woman [25, 30]. Therefore, a history of STI is considered a significant determinant of pre-cervical cancer. The sample size was 456 (114 cases and 342 controls), using a history of STI as a significant determinant of pre-cervical cancer (Table 1). After adding a 5% non-response rate to the cases and controls, the final sample size included in the study was 480 (120 cases and 360 controls) (Table 1).
Table 1: Sample size determination for determinants of pre-cervical cancer among women aged 30–49 years in Woliso Town, Oromia, in 2022.
| Variable | Confidence level | Power | Ratio of controls to cases | % Of controls exposed | AOR | Calculated sample size | Reference | ||
| Cases | Controls | Total | |||||||
| Parity ≥4 | 95% | 80% | 3:1 | 41.1 | 2.3 | 68 | 203 | 271 | [30] |
| History of STI | 95% | 80% | 3:1 | 32.4 | 1.9 | 114 | 342 | 456 | |
| HIV positive | 95% | 80% | 3:1 | 13.85 | 7.4 | 16 | 47 | 63 | [25] |
Sampling Technique
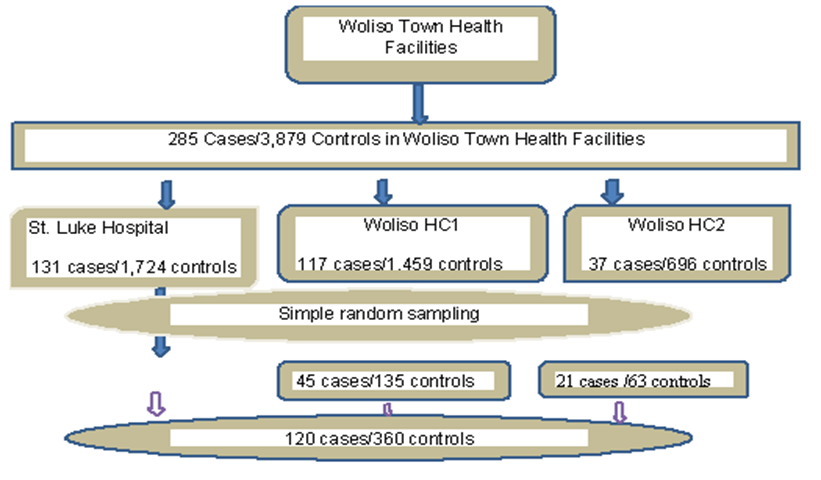
There are currently three health facilities provide routine screening for cervical cancer in Woliso Town. In the last 5 years, a total of 4,331 women were screened, of which 285 were found to be VIA-positive (cases), whereas 3,879 were VIA-negative (controls). Of the 1,964 women screened at St. Luke Hospital, 131 were found to be cases and 1,724 were controls. A total of 1,622 women were screened in Woliso Town HC No. 1, of which 117 were cases and 1,459 were controls. Similarly, in Woliso Town HC No. 2, 745 women were screened, of whom 37 were cases and 696 were controls. The sample size was allocated to the three facilities in proportion to the total uptake of cervical cancer screening in the last 5 years. For the selection of study participants’ documents, serial numbers on cervical cancer screening and treatment registration books were used as sampling frames. Cases were selected from each facility by simple random sampling using computer-generated random numbers. For each case, three controls were selected using the same method (Figure 1).
Figure 1: Sampling procedure for the determinants of pre-cervical cancer among women aged 30–49 years in Woliso Town, Oromia, in 2022
Study Variables
Dependent Variable: Status of pre-cervical cancer among women aged 30–49 years.
Independent Variables
Sociodemographic characteristics: Age, residence, educational status, and marital status of the woman.
Reproductive factors: Number of pregnancies, number of births, age at menarche, contraceptive usage, age at first marriage, contact bleeding, and pain during sexual intercourse.
Other factors: Source of information about cervical cancer screening service, history of STI, HIV status of the woman, HIV status of partner, women, and family history of cancer.
Operational Definitions
Pre-cervical cancer: A woman was taken as having pre-cervical cancer if registered as VIA positive, and not having pre-cervical cancer if registered as VIA negative, Case: A woman screened for cervical cancer and registered as VIA positive, Control: A woman Screened for cervical cancer and registered as VIA negative, early marriage: Marriage before the age of 18.
Data Collection tools and procedures
A structured data extraction form (checklist) was used to collect necessary information from the register and history card. All variables in the checklist were developed from the information available on the cervical cancer screening registration and client history cards. Trained nurses and midwives performed data extraction using a checklist. The data were collected by reviewing secondary data (from registration books and client cards).
Data quality assurance
A properly designed data-collection checklist was used to ensure data quality. Two diploma nurses and one midwife were recruited for data collection. Similarly, one Health Officer was recruited as the supervisor. A day of training was provided to all participants on the data extraction checklist and ethical principles during data collection. The collected data were reviewed daily and checked for completeness, accuracy, and consistency by supervisors and investigators.
Data processing and analysis
The completed checklists were checked for completeness and consistency. Data were coded and entered into Epi-info version 7.2.2.6, and then exported to the SPSS version 21 statistical software for analysis. Data were analyzed using a binary logistic regression model. Sociodemographic, reproductive, source of information, sexual health, and women’s previous history of cancer were summarized using descriptive statistics. The 95% Confidence Interval (95% CI)of the adjusted odds ratio (AOR)was computed to identify the presence and strength of the association. Variables with a p-value <0>p = 0.34). Statistical significance was declared at p <0>
Ethical Consideration
Ethical clearance was obtained from the Ethical Review Board of Ambo University College of Medicine and Health Sciences before data collection with Ref. No: PGC/275/2021. Permission to conduct the study in health facilities was secured from the Woliso Town Health Office and the respective health facilities. Confidentiality of the information was maintained. Since it is too difficult for patients from health institutions to sign on behalf of themselves, the agreement of study participants was sought from the legally designated head of institutions.
Results
Socio-demographic characteristics of the women
In the study population, 37.5% of the cases and 48.6% of the controls were aged–30–34 years. The median ages of the patients and controls were 35 ± 9 and 35 ± 8 years, respectively. Regarding the residence of the study population, 51.7% of cases and 68.3% of controls were urban residents. Regarding educational status, 33.3% of the patients and 30.8% of the controls had no formal education. Regarding marital status, the majority of patients (93.3%) and controls (92.8%) were married (Table 2).
Table 2: Socio-demographic characteristics of women aged 30–49 years, screened for cervical cancer in Woliso Town, Oromia, in 2022.
| Variables | Variable category | Cases, n (%) | Controls, n (%) | Total, n (%) |
| Age of the women in years | 30–34 | 45 (37.5%) | 175 (48.6%) | 220 (45.8%) |
| 35–39 | 38 (31.7%) | 104 (28.9%) | 142 (29.6%) | |
| 40–44 | 20 (16.7%) | 53 (14.7%) | 73 (15.2%) | |
| 45–49 | 17 (14.2%) | 28 (7.8%) | 45 (9.4%) | |
| Residence of women | Rural | 58 (48.3%) | 114 (31.7%) | 172 (35.8%) |
| Urban | 62 (51.7%) | 246 (68.3%) | 308 (64.2%) | |
| Educational status of the women | No formal education | 40 (33.3%) | 111 (30.8%) | 151 (31.5%) |
| Read and write | 19 (15.8%) | 59 (16.4%) | 78 (16.3%) | |
| Primary | 33 (27.5%) | 95 (26.4%) | 128 (26.7%) | |
| Secondary | 21 (17.5%) | 71 (19.7%) | 92 (19.2%) | |
| College and university | 7 (5.8%) | 24 (6.7%) | 31 (6.5%) | |
| Marital status of the women | Married | 112 (93.3%) | 334 (92.8%) | 446 (92.9%) |
| Divorced/widowed | 8 (6.7%) | 26 (7.2%) | 34 (7.1%) |
Reproductive characteristics of the women
Regarding the number of pregnancies, 56.7% of cases and 52.2% of controls had a pregnancy history of 2–4 times. Similarly, 59.2% of cases and 53.3% of controls were multiparous women. With regard to age at first marriage, early marriage was relatively higher among cases (40.0%) than among controls (28.1%). The median ages at first marriage for the case and control groups were 18 ± 4 and 18 ± 3 years, respectively. In addition, the mean and standard deviation of age at menarche for the cases and controls were 14.45 ± 1.41 years and 14.63 ± 1.34 years, respectively. The majority of patients (75.0%) and controls (70.6%) used at least one type of modern contraceptive. The most commonly used contraceptive method was injectable (50.8%), followed by implants (23.3%). Similarly, the most commonly used contraceptive method among the controls was injectable (51.4%), followed by implants (18.6%). The use of oral contraceptive pills (OCPs) and implants in these cases was relatively higher than that in the controls. Approximately 5.8% of the patients and 2.5% of the controls had a history of pain during sexual intercourse. Similarly, 5.0% of cases and 1.4% of controls had a history of contact bleeding (Table 3).
Table 3: Reproductive characteristics of women aged 30–49 years, screened for cervical cancer in Woliso Town, Oromia, in 2022.
| Variables | Variable category | Cases, n (%) | Controls, n (%) | Total, n (%) |
| Gravidity of the woman | No (Nulligravida) | 5 (4.2%) | 17 (4.7%) | 22 (4.6%) |
| 1 (Primigravida) | 11 (9.2%) | 40 (11.1%) | 51 (10.6%) | |
| 2–4 (Multigravida) | 68 (56.7%) | 188 (52.2%) | 256 (53.3%) | |
| ³5 (Grand multigravida) | 36 (30.0%) | 115 (31.9%) | 151 (31.5%) | |
| Parity of the woman | No (Nullipara) | 5 (4.2%) | 22 (6.1%) | 27 (5.6%) |
| 1 (Primipara) | 14 (11.7%) | 45 (12.5%) | 59 (12.3%) | |
| 2–4 (Multipara) | 71 (59.2%) | 192 (53.3%) | 263 (54.8%) | |
| ³5 (Grand multipara) | 30 (25.0%) | 101 (28.1%) | 131 (27.3%) | |
| Age at first marriage | <18> | 48 (40.0%) | 101 (28.1%) | 149 (31.0%) |
| ³18 | 72 (60.0%) | 259 (71.9%) | 331 (69.0%) | |
| Age at menarche | £12 | 13 (10.8%) | 20 (5.6%) | 33 (6.9%) |
| 13–14 | 48 (40.0%) | 140 (38.9%) | 188 (39.2%) | |
| ³15 | 59 (49.2%) | 200 (55.6%) | 259 (54.0%) | |
| Ever used contraceptive | Yes | 90 (75.0%) | 254 (70.6%) | 344 (71.7%) |
| No | 30 (25.0%) | 106 (29.4%) | 136 (28.3%) | |
| Ever used OCP | Yes | 24 (20.0%) | 49 (13.6%) | 73 (15.2%) |
| No | 96 (80.0%) | 311 (86.4%) | 407 (84.8%) | |
| Ever used injectable contraceptive | Yes | 61 (50.8%) | 185 (51.4%) | 246 (51.2%) |
| No | 59 (49.2%) | 175 (48.6%) | 234 (48.8%) | |
| Ever used implant | Yes | 28 (23.3%) | 67 (18.6%) | 95 (19.8%) |
| No | 92 (76.7%) | 293 (81.4%) | 385 (80.2%) |
Sexual health and previous history of cancer
Regarding the history of STI, approximately 12.5% of cases and 11.7% of controls were treated for at least one type of STI. The history of genital ulcers was higher among cases (6.7%) than among controls (1.4%). In addition, the majority of cases (94.2%) and controls (95.0%) were aware of their HIV status. The HIV prevalence was higher among cases (17.5%) than among controls (8.1%). Regarding screening for breast cancer, all cases and controls were screened for breast cancer, while the magnitude of positive results was relatively higher among cases (6.7%) as compared to controls (2.2%). In addition, only 0.8% of cases and 1.1% of controls had a history of cancer. Cases had a relatively higher family history of cancer (8.3%) than controls (2.5%) (Table 4).
Table 4: Sexual health and previous history of cancer among women aged 30–49 years screened for cervical cancer in Woliso Town, Oromia, in 2022.
| Variables | Variable category | Cases, n (%) | Controls, n (%) | Total, n (%) |
| Ever treated for STI | Yes | 15 (12.5%) | 42 (11.7%) | 57 (11.9%) |
| No | 105 (87.5%) | 318 (88.3%) | 423 (88.1%) | |
| Had history of vaginal discharge | Yes | 12 (10.0%) | 30 (8.3%) | 42 (8.8%) |
| No | 108 (90.0%) | 330 (91.7%) | 438 (91.2%) | |
| Had history of genital ulcer | Yes | 8 (6.7%) | 5 (1.4%) | 13 (2.7%) |
| No | 112 (93.3%) | 355 (98.6%) | 467 (97.3%) | |
| The woman knew her HIV status | Yes | 113 (94.2%) | 342 (95.0%) | 455 (94.8%) |
| No | 7 (5.8%) | 18 (5.0%) | 25 (5.2%) | |
| HIV status of the woman | Reactive | 21 (17.5%) | 29 (8.1%) | 50 (10.4%) |
| Non-reactive or not known | 99 (82.5%) | 331 (91.9%) | 430 (89.6%) | |
| Partner HIV status | Reactive | 6 (5.0%) | 19 (5.3%) | 25 (5.2%) |
| Non-reactive | 39 (32.5%) | 97 (26.9%) | 136 (28.3%) | |
| Not known | 75 (62.5%) | 244 (67.8%) | 319 (66.5%) | |
| Result of breast cancer screening | Negative | 112 (93.3%) | 352 (97.8%) | 464 (96.7%) |
| Breast lump, cancer or other | 8 (6.7%) | 8 (2.2%) | 16 (3.3%) | |
| Had family history of cancer | Yes | 10 (8.3%) | 9 (2.5%) | 19 (4.0%) |
| No | 110 (91.7%) | 351 (97.5%) | 461 (96.0%) |
Source of information about pre-cervical cancer screening service
The sources of information regarding cervical cancer screening were analyzed for cases and controls. Accordingly, the dominant sources of information about cervical cancer screening for cases and controls were healthcare workers, followed by the mass media. Women’s development armies, families, and friends were sources of information for only a small proportion of cases and controls.
Factors associated with pre-cervical cancer
Multivariable Analysis
In the multivariable binary logistic regression, being a rural resident, age at menarche ≤12 years, use of OCP, history of genital ulcer, being HIV positive, and a family history of cancer were factors that were significantly associated with pre-cervical cancer. Accordingly, rural resident women were 2.44-times more likely to have pre-cervical cancer (AOR = 2.44, 95% CI = 1.55–3.85) as compared to urban residents. Women who had seen their first menstrual cycle at the age of ≤12 years were 2.83-times more likely to have pre-cervical cancer (AOR = 2.83, 95% CI = 1.25–6.39) as compared to women who had seen their first menstrual cycle at the age of ≥15 years. Similarly, women who had ever used OCP were 1.83-times more likely to have pre-cervical cancer (AOR = 1.83, 95% CI = 1.03–3.25) as compared to women who never used OCP. In addition, women with a history of genital ulcer were 3.86-times more likely to have pre-cervical cancer (AOR = 3.86, 95% CI = 1.12–13.31) as compared to women with no history of genital ulcers. Women who were reactive for HIV were 2.55-times more likely to have pre-cervical cancer (AOR = 2.55, 95% CI = 1.34–4.88) as compared to women with no history of HIV infection. Similarly, women with a family history were 3.87-times more likely to have pre-cervical cancer (AOR = 3.87, 95% CI = 1.47–10.21) as compared to women with no family history of cancer (Table 5).
Table 5: Multivariable binary logistic regression analysis of selected variables among women aged 30–49 years screened for cervical cancer in Woliso Town, Oromia, in 2022.
| Variables | Variable category | Cases, n (%) | Controls, n(%) | COR (95% CI) | AOR (95% CI) | p-value |
| Residence of women | Rural | 58 (48.3%) | 114 (31.7%) | 2.02(1.33–3.08) | 2.44 (1.55–3.85) | <0> |
| Urban | 62 (51.7%) | 246 (68.3%) | 1 | |||
| Age at menarche | £12 | 13 (10.8%) | 20 (5.6%) | 2.20 (1.03–4.69) | 2.83 (1.25–6.39) | 0.01** |
| 13–14 | 48 (40.0%) | 140 (38.9%) | 1.16 (0.75–1.80) | 1.31 (0.83–2.09) | 0.25 | |
| ³15 | 59 (49.2%) | 200 (55.6%) | 1 | |||
| Ever used oral contraceptive pills | Yes | 24 (20.0%) | 49 (13.6%) | 1.59 (0.93–2.72) | 1.83 (1.03–3.25) | 0.04** |
| No | 96 (80.0%) | 311 (86.4%) | 1 | |||
| Had history of genital ulcer | Yes | 8 (6.7%) | 5 (1.4%) | 5.07 (1.63–15.82) | 3.86 (1.12–13.31) | 0.03** |
| No | 112 (93.3%) | 355 (98.6%) | 1 | |||
| HIV status of the woman | Reactive | 21 (17.5%) | 29 (8.1%) | 2.42 (1.32–4.43) | 2.55 (1.34–4.88) | 0.005** |
| Non-reactive or not known | 99 (82.5%) | 331 (91.9%) | 1 | |||
| Had family history of cancer | Yes | 10 (8.3%) | 9 (2.5%) | 3.55 (1.40–8.95) | 3.87 (1.47–10.21) | 0.01** |
| No | 110 (91.7%) | 351 (97.5%) | 1 |
**Significant at p-value <0>Abbreviations: COR, Crude odds ratio; AOR, Adjusted odds ratio; CI, Confidence Interval
Discussion
This study aimed to identify the determinants of pre-cervical cancer among women aged 30–49 years screened for cervical cancer at health facilities in Woliso Town. Secondary data from cervical cancer screening registration books and women’s history cards were used as sources of information. The results of this study revealed that being a rural resident, age at menarche ≤12 years, ever use of OCP, having a history of genital ulcer, being HIV positive, and having a family history of cancer were significant determinants of pre-cervical cancer. In this study, there was a significant association between residence and pre-cervical cancer. This study revealed that women residing in rural areas were 2.44-times more likely to develop pre-cervical cancer than urban residents. The findings of this study are consistent with those of a study conducted in Northwest Ethiopia [22]. A possible explanation for this association might be due to the fact that rural women are not well informed about the risk of STI, particularly HPV. In addition, health facilities providing screening for pre-cervical cancer might not be easily accessible for the early screening of rural women. In the current study, the age at menarche was significantly associated with pre-cervical cancer. Accordingly, women who had experienced menarche at the age of ≤12 years were 2.83-times more likely to have pre-cervical cancer than those who had experienced menarche at the age of ≥15 years. This finding is supported by a study conducted in the United Kingdom in which women whose menarche was at the age of ≤12 years were more likely to have cervical cancer as compared to those whose menarche was at the age of ≥15 years [31]. The reason for this association may be the exposure of cervical cells to pubertal hormones at an early age and for a longer time. In addition, menarche at an early age might be associated with early sexual activity, which in turn predisposes them to STI, including HPV [32].
In the current study, it was also found that women who had used OCP were 1.83-times more likely to have pre-cervical cancer than those who had never used OCP. This finding is supported by previous studies conducted in the referral hospitals from Amhara Region [20] and Adama Town [24]. This association might be due to the fact that oral contraceptive pills change the cells of the cervix, which increases the susceptibility of cervical cells to persistent infection with high-risk HPV types. In contrast, the findings of this study are inconsistent with those of a study conducted in Finland on the risk of cervical atypia in oral contraceptive users, in which the use of oral contraceptives was a protective factor against cervical atypia [33]. This inconsistency in association might be due to the difference in the duration of oral contraceptive use among the study populations. The findings of this study showed a significant association between the HIV status of women and pre-cervical cancer. In this study, women who were HIV-positive were 2.55-times more likely to have pre-cervical cancer than those with no history of HIV infection. This finding is consistent with those of studies conducted in Addis Ababa [17] and Hawassa University Referral Hospital [25]. This association might be due to the fact that HIV weakens the immune system of women and puts them at higher risk of HPV infection. Therefore, HIV-positive women should be prioritized for screening and management of pre-cervical cancer. Another finding of the present study is that there is a significant association between genital ulcers that cause sexually transmitted infections and pre-cervical cancer. Several studies have shown a significant association between STI and pre-cervical cancer. Accordingly, studies conducted in North Ethiopia [27], Amhara region referral hospitals [20], Adama [26], and Addis Ababa [28] showed a positive association between STI and pre-cervical cancer, which was consistent with the findings of this study. However, what is new in the present study is that the association of STI with pre-cervical cancer is limited to genital ulcers that cause STI. This may be due to genital ulcers facilitating HPV transmission. This study also revealed that a family history of cancer is a significant determinant of pre-cervical cancer among women aged 30–49 years. Women with a family history of cancer were 3.87-times more likely to have pre-cervical cancer than women with no family history of cancer. Pre-cervical cancer is more prevalent among women with a family history of cancer because some women may inherit conditions that make them less able to fight HPV infections than others [34].
Limitations of the study
As the data were extracted from secondary sources, the validity of the test could not be verified. Some data on the lifestyle and sexual behavior of the women, such as history of smoking and number of lifetime sexual partners, could not be included in the study because they were not available on registration. Furthermore, this study was health-facility-based, making it difficult to generalize the findings to the general population.
Conclusion
This study revealed that being a rural resident, age at menarche ≤12 years, use of oral contraceptive pills, history of genital ulcers, being HIV positive, and having a family history of cancer were determinants of pre-cervical cancer among women aged 30–49 years in Woliso Town. Therefore, it is better to focus on these determinants to prevent pre-cervical cancer among women aged 30–49 years in the area.
Acronyms and abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; FGAE, Family Guidance Association of Ethiopia; FMOH, Federal Ministry of Health; HC, Health Center; HIV, Human Immunodeficiency Virus; HPV, Human papilloma virus; IQR, interquartile range; IUCD, intrauterine contraceptive device; OCP, Oral Contraceptive Pills; STI, Sexually Transmitted Infections; VIA, Visual Inspection of the cervix with acetic acid; VIF, Variance inflation factor; WHO, World Health Organization
Acknowledgments
First and most importantly, we would like to thank the Ambo University for giving us this special opportunity. Again, our sincere appreciation goes to the women screened for cervical cancer at health facilities in Woliso Town. In addition, we would like to express our appreciation to the Woliso Town Health Office and the three health facilities for their cooperation during the data collection. Finally, we would like to extend our thanks to data collectors for their active participation and cooperation.
Declarations
Authors declared that there are no conflicts of interests.
References
- Castle, P. E. et al. (2017). Treatment of cervical intraepithelial lesions. Int. J. Gynecol. Obstet, 138:20-25.
Publisher | Google Scholor - (2019). A How-to-Guide to cervical cancer screening and treatment programmes. Int. Plan. Parent. Fed.
Publisher | Google Scholor - WHO. (2014). Comprehensive Cervical Cancer Control. Geneva, 366-378.
Publisher | Google Scholor - Arbyn, M. et al. (2020). Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob. Heal, 8:e191-e203.
Publisher | Google Scholor - WHO. (2019). Screening and Treatment of Pre-Cancerous Lesions for Secondary Prevention of Cervical Cancer Technology Landscape. 1-46.
Publisher | Google Scholor - (2021). Human papillomavirus (HPV) and cervical cancer Key facts. 20.
Publisher | Google Scholor - Echelman, D. & Feldman, S. (2012). Management of cervical precancers: A global perspective. Hematol. Oncol. Clin. North Am, 26:31-44.
Publisher | Google Scholor - (2015). Pan American Health Organization, WHO & Cervical Cancer Prevention in Latin America and The Caribbean. Health Education Series on Human Papillomavirus and Cervical Cancer Fact Sheet 5 Treatment of Cervical Cancer. Pan Am. Heal. Organ.
Publisher | Google Scholor - Strategy, G. et al. (2020). Global strategy to accelerate the elimination of cervical cancer as a public health problemand its associated goals and targets for the period 2020-2030.
Publisher | Google Scholor - FMoH. (2015). National Cancer Control Plan 2016 - 2020 of Ethiopia. Dis. Prev. Control Dir. 83.
Publisher | Google Scholor - Fuenmayor, A. et al. (2018). Detection of precancerous lesions in the cervix and HPV infection in women in the region of Maniapure , Bolivar State. 1-11.
Publisher | Google Scholor - Riedel, J. & Rwanda, mes. (2015). Prevalence and risk factors for cervical cancer and pre-cancerous lesions in. Open Access, 8688:1-8.
Publisher | Google Scholor - Donkoh, E. T., Agyemang-yeboah, F. & Bl, L. L. B. (2019). Prevalence of cervical cancer and pre-cancerous lesions among unscreened Women in Kumasi, Ghana. 1-6.
Publisher | Google Scholor - Abate, S. M. (2015). Cervical Cancer: Open Access Trends of Cervical Cancer in Ethiopia. Cerv. Cancer, 1:1-4
Publisher | Google Scholor - Eliyas B.W, K. S. (2020). Prevalence of Abnormal Cervical Lesions and Associated Factors Among Women in Harar, Eastern Ethiopia. 12429-12437.
Publisher | Google Scholor - Kote, M., Kejela, G. & Getachew, T. (2019). Magnitude and Factors Associated with Precervical Cancer among Screened Women in Southern Ethiopia.
Publisher | Google Scholor - Temesgen, T., Adhena, G. & Figa, Z. (2020). Precancerous Cervical Lesion Among Women in Public Hospitals of Addis Ababa, Ethiopia. 8:94-99.
Publisher | Google Scholor - (2015). Federal Democratic Republic of Ethiopia Ministry of Health. Guideline for Cervical Cancer Prevention and Control in Ethiopia.
Publisher | Google Scholor - Nessa, A. et al. (2020). Influence of Demographic and Reproductive Factors on Cervical Pre-Cancer and Cancer in Bangladesh. 21:1883-1889.
Publisher | Google Scholor - Taye, B. T., Mihret, M. S. & Muche, H. A. (2021). Risk factors of precancerous cervical lesions : The role of women ’ s socio-demographic , sexual behavior and body mass index in Amhara region referral hospitals ; case-control study. 2:1-15.
Publisher | Google Scholor - International, T. (2019). Proportions of Pre-Cancerous Cervical Lesions and Its Associated Factors among Women Clients in the Age Group of 30-49yrs in Gynecology Ward of Dessie Referral Hospital and FGAE , North-East. 9:1-15.
Publisher | Google Scholor - Getinet, M. Precancerous Lesions of the Cervix and Associated Factors among Women of East. (2021).
Publisher | Google Scholor - Ansa, M., Mekonnen, T. & Ababa, A. (2018). Prevalence of via positive cervical lesions and determinant factors among women attending regular gynecology outpatient department (RGOPD) at saint paul’ s hospital millennium medical college (SPHMMC). 10:22-30.
Publisher | Google Scholor - Kassa, R. T. (2018). Risk factors associated with precancerous cervical lesion among women screened at Marie Stops Ethiopia, Adama town, Ethiopia 2017: A case control study. BMC Res. Notes, 11:1-5.
Publisher | Google Scholor - Dejene, A. S. & Hailu, D. (2020). Determinants of pre-cervical cancer among women visiting Hawassa University Comprehensive Specialized Hospital, Ethiopia: A case control study. 19:63-69.
Publisher | Google Scholor - Merera, D. & Jima, G. H. (2021). Precancerous cervical lesions and associated factors among women attending cervical screening at Adama hospital Medical College, Central Ethiopia. Cancer Manag. Res, 13:2181-2189.
Publisher | Google Scholor - Hailemariam, G. et al. (2020). Magnitude and associated factors of VIA positive test results for cervical cancer screening among refugee women aged 25-49 years in North Ethiopia. BMC Cancer, 20:1-7.
Publisher | Google Scholor - Teame, H. et al. (2018). Factors associated with cervical precancerous lesions among women screened for cervical cancer in Addis Ababa, Ethiopia: A case control study. PLoS One, 13:1-13.
Publisher | Google Scholor - (2021). Woliso Town Health Office, Socio-demographic data of Woliso Town 2020/2021.
Publisher | Google Scholor - Tekalegn, Y., Aman, R., Woldeyohannes, D., Sahiledengle, B. & Degno, S. (2020). Determinants of VIA Positivity Among Women Screened for Cervical Precancerous Lesion in Public Hospitals of Oromia Region, Ethiopia: Unmatched Case-Control Study. 587-596.
Publisher | Google Scholor - Sharma, P. & Pattanshetty, S. M. (2018). A study on risk factors of cervical cancer among patients attending a tertiary care hospital: A ase-control study. Clin. Epidemiol. Glob. Heal. 6:83-87.
Publisher | Google Scholor - Ibitoye, M., Choi, C., Tai, H., Lee, G. & Sommer, M. (2017). Early menarche: A systematic review of its effect on sexual and reproductive health in low- and middle-income countries. 1-24.
Publisher | Google Scholor - Adhikari, I., Eriksson, T., Luostarinen, T., Lehtinen, M. & Apter, D. (2018). The risk of cervical atypia in oral contraceptive users. Eur. J. Contracept. Reprod. Heal. Care, 23:12-17.
Publisher | Google Scholor - American Cancer Society. (2020). Cervical Cancer Causes , Risk Factors , and Prevention Risk Factors for Cervical Cancer. 1-15.
Publisher | Google Scholor