Research Article
Determinants of Maternal Mortality in Nekemte Town Government Hospitals, Eastern Wollega, Oromia Region, Ethiopia, 2022 G.C
- Lili Asefa Merga 1**
- Tewodros Kassahun Tarekegn 2*
- Kirubel Tesfaye Hailu 3*
- Feven Negasi Abriha 3
- Hamlet Mulu Aberha 2
- Buure Ayderuss Hassen 2
- Michael Yefrashowa Betemariam 2
- Damise Dugasa Gessifata 1
- Sanyi Beyena Garbi 1
- Rediet Habtu Lebelo 4
- Helen Assefa Berhe 5
- Solomon Endale Dagnachew 2
- Birukti Gebreyohannes Habtezgi 2
- Surafel Alemayehu Tsegaye 6
1Department of Medicine, Wollega University, Oromia, Ethiopia
2Department of Medicine, Hayat Medical College, Addis Ababa, Ethiopia.
3Department of Medicine Jimma University Oromia Region, Ethiopia
4Department of Medicine, Mekelle University, College of Health Science, Mekelle. Ethiopia.
5Department of Medicine, Addis Ababa University, Tikurs Anbessa, College of Health Sciences, Ethiopia.
6MPH Candidate at the Harvard T.H. Chan School of Public Health in Boston, Massachusetts, USA.
*Corresponding Author: Tewodros Kassahun Tarekegn, Department of Medicine, Hayat Medical College, Addis Ababa, Ethiopia.
Citation: Lili A. Merga, Tewodros K. Tarekegn, Kirubel T. Hailu, Feven N. Abriha, Hamlet M. Aberha, et al., (2024). Determinants of Maternal Mortality in Nekemte Town Government Hospitals, Eastern Wollega, Oromia Region, Ethiopia, 2022 G.C., Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(1):1-14. DOI: 10.59657/2993-0871.brs.24.025
Copyright: © 2024 Tewodros Kassahun Tarekegn, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: December 13, 2023 | Accepted: December 29, 2023 | Published: January 08, 2024
Abstract
Background: Maternal mortality is defined by World health organization as the demise of a woman during maternity in the first 42 days of cessation of pregnancy, regardless of site & time of the pregnancy, from any reason linked to gravidity or its management, but not from unintentional causes. The Sustainable Development Goal puts an ambitious target of achieving maternal mortality rate of 70 per 100,000 live births in 2030, while Ethiopian Health sector transformation plan targets to decrease to 199 per 100000 Live births.
Objective: This study aimed to assess determinants of maternal mortality in Nekemte town Government Hospitals from September 2017 August 2022 G.C.
Methods: Institution-based case–control study was used to identify determinants of maternal death. A total of 216 samples (54 cases and 162 controls) with a case to control ratio of 1:3 was selected. Cases are mothers who died during their maternity period where as controls are mothers who survived. Data was edited for accuracy, readability, consistence and completeness; thereafter it was coded and entered into Epi Info version 7.2.5.0 and exported to SPSS 20 computer software programs for cleaning and descriptive analysis. Bivariate logistic regression analysis was done & variables with p-value <0.25 was transferred to Multivariate analysis & variables with P-value < 0.05 was considered as statistically significant & AOR with 95% CI was used to control for possible confounders & to interpret the result. Finally, the results were summarized & presented by using tables, graphs & charts.
Result: More than two third (75.93%) of death occurred during post-partum period. Determinants of maternal death include: age group of 20-34 (OR 2.127, 95% (0.374, 12.102)), being from rural area (OR 6.615, 95% CI (0.14, 0.562)), prolonged labour, Haemorrhage (OR=1.91, 95% CI (0.33, 2.27)), Pregnancy induced hypertension (OR=1.28, 95% CI (1.01, 3.31) and comorbidities (OR=18.458, 95%CI (3.639, 93.615)).
Conclusion: Most of the women died in the postpartum period, mainly because of direct obstetric causes, of which Haemorrhage was the leading cause of death and followed by sepsis and Pregnancy induced hypertension.
Keywords: maternal mortality; determinants; trends; nekemte specialized hospital; WURH
Introduction
Maternal mortality is defined by World health organization (WHO) as the demise of a woman during maternity in the first 42 days of cessation of pregnancy, regardless of site & time of the pregnancy, from any reason linked to gravidity or its management, but not from unintentional causes [1]. Estimates of maternal mortality are therefore based solely on the timing of the death in relationship to pregnancy. Maternal health has become one of the major public health concerns for developing countries following the first safe motherhood conference held in Kenya in 1987 [2]. In the post Millennium Development era (MDG) era, the Sustainable Development Goal (SDG) puts an ambitious target of achieving MMR of 70 per 100,000 live births (LB) in 2030 [3].While some progress have been made, according to WHO estimate in 2015, the Maternal Mortality Ratio (MMR) dropping by 43.9% worldwide between 1990 and 2015, it remains unacceptably high in developing countries particularly in sub-Sahara African countries [4]Furthermore, the 2011 Ethiopian demographic and health survey (EDHS) (676/100,000) showed that there is an increase of MMR from 2005 EDHS (673/100,000), but EDHS 2016 reveals decreasing trends (412/100000). The effects of maternal mortality have impacts on children and remaining families. For instance, the infant and under-five survival are highly correlated with child nutrition and other important child health care practices demanding maternal involvement [5]. The causes of maternal mortality are multi-factorial. An in-depth analysis on the trends of maternal health in Ethiopia pointed to demographic, behavioral, nutritional, and health services related factors are associated with poor maternal health outcomes [6]. Yet, the key factors attributable for the death of mothers are related to low facility deliveries, poor competence of providers, lack of emergency obstetric services at facilities, and inefficient referral systems for obstetric emergencies and in this regard, several studies reported limited utilization of key maternal health services in Ethiopia [7].
Statement of the problem
Maternal mortality is a global health problem and has devastating effects on the family she leaves behind and country level [8]. Pregnancy related complications account about five million maternal deaths with the global estimate for lifetime risk of maternal deaths 1 in 74 [9] and an estimated 295 000 maternal deaths occurred in 2017, yielding an overall MMR of 211 per 100 000 LBs [10]. Developed countries have ratios less than 10-20 per hundred thousand live births. The corresponding ratios for developing countries range in the several hundred; reaching up to eight hundred or more in some countries. Over 99% of maternal deaths occur in low- and middle-income countries due to extreme poverty resulting in lack of access to quality healthcare and education of women [11]. Which is 14 times higher than that in developed regions. The majority of maternal deaths occur in Sub-Saharan, accounting for 62 % of maternal deaths and has the highest MMR, at 510 maternal deaths per 100,000 live births [12]. There was significant regional disparity; with women in sub-Saharan Africa having a lifetime risk of 1 in16 [13]. Maternal mortality ratio is the health indicator showing the largest disparity between developed and developing countries. It becomes one of the major public health concerns for developing countries [14]. The adult lifetime risk of maternal mortality, the probability that a 15-year-old woman will die eventually from a maternal cause in Sub-Saharan Africa is the highest at 1 in 38; and 1 in 3,700 among women in developed countries [15]. Ethiopia is categorized under the countries with high maternal mortality, EDHS 2016 reports the maternal mortality is high as 412 per 100,000 live births. Levels of maternal mortality indicate the quality of maternity services rendered. A country’s level of maternal mortality is indirect evidence that shows Quality of service delivery and referral system, Number, distribution, and training of the types of providers required, including midwives and obstetrician-gynecologists, Leadership and financing, well-functioning health system, how health institutions are well organized & equipped, emergency obstetric services are highly responsive, the care given to mothers is of high standard [16].
The effects of maternal mortality have impacts on children and remaining families. For instance, the infant and under-five survival are highly correlated with child nutrition and other important child health care practices demanding maternal involvement [5]. Seventy-three percent of all maternal deaths were attributable to direct obstetric causes; (hemorrhage, PIH, Abortion, sepsis) deaths due to indirect causes accounted for 27.5 % (anemia and malaria) [13]. Some of the factors mentioned as contributory to maternal deaths are lack of intensive care unit facility, not having antenatal care, absence of blood transfusion services, and lack of essential supplies at hospitals, delayed diagnosis and surgical interventions and delayed seeking of health care. Residence in rural areas, presence of co morbidity, women who were referred from health institutions and women who had prolonged labor had increased likelihood of maternal death and most death (74.8%) occurred during post-partum period; from post-partum period of the first three days [17]. Sustainable Development Goal (SDG) puts an ambitious target of achieving MMR of 70 per 100,000 live births (LB) in 2030 [3]. While some progresses have been made, according to WHO estimate in 2015, the Maternal Mortality Ratio (MMR) dropping by 43.9% worldwide between 1990 and 2015, it remains unacceptably high in developing countries particularly in sub-Sahara African countries [4]. In Ethiopia the reports also show that there is great disparity, targeted 267per 100,000 live births, achieved is 412 per100,000 live births [16]. Maternal age (younger than 20 and over 30), parity (primipara and grand multipara), marital status (single) and occupation, places of delivery, previous C/S, showed a significant association with the risk of maternal death. However, other equally important factors like Gravidity, delivery attending physician, presence of Obstetric complications and Distance from the hospital and Residency area of patients have been given little attention, and thus are not well studied or understood [18].
Significance of the Study
Maternal death is widely regarded as one of life’s most tragic outcomes. There is a big pain in the death of a woman who is engaged in the act of creating life, and her death is an incomparable loss for any children who are left behind.
Therefore, the aim of this study is to assess determinants of maternal mortality which is essential to assess existing status as well as monitor changes effected by interventions in government hospitals in Nekemte town It will also identify variation in relation to age groups, residence (rural, urban), gravidity, parity and duration of labor as a result helps health professionals to work on early identification and detection of obstetric risk factors and complication and to give appropriate intervention to reduce maternal death. Information generated from this study can be used by health professionals, health care planners, managers and policy makers to save women’s lives by improving the quality of care provided. It is intended that this information will help or contribute to change policies and practices that will lead to improvements in maternal health. It is also intended that this study can be used as input for WURH, researchers and academicians.
Determinants of Maternal Deaths
According to the World Health Organization (WHO) document from Millennium Development Goals (MDG) to Sustainable Development Goals (SDG), an estimation of 303, 000 maternal deaths occurred worldwide from pregnancy and its complications which is equivalent to 830 mothers dying every day (more than 1 life lost every 2 minutes) in 2015. Nearly, all of these deaths are preventable in nature if appropriate interventions are taken [21]. The determinant factors were presence of obstetric complications, presence of obstructed labor and preexisting medical problems were risk factors for maternal death [31].
Socio-demographic Determinants
Many studies showed that the risk of maternal death is significantly associated with the occupation, age, education (of the mother and husband), substandard or no ANC service and visit, place of residency, maternal obstetrics characteristics (gravidity and parity), and preexisting Problems [28]. Although the overall risks of maternal death are highest among young adolescents and older women of reproductive age, the highest number of deaths is in the middle group of women around age 25 years. Study in Ghana shows the age group with the highest number of deaths was30 to 35 with 24.7 percent, followed closely by the 30-34 age groups with 23.4 percent. Indeed, the age group of 30-39 accounted for nearly half of the deaths in the cases. While, in Ethiopia the EDHS 2016, shows highest number of deaths was 30-34 followed by 40-44. The 30-39 age groups accounted for the highest number of deaths due to the fact that they were ‘multi-gravid’, thus they had given births multiple times in the past [30]. According to the World Health Organization (WHO) document from Millennium Development Goals (MDG) to Sustainable Development Goals (SDG), an estimation of 303, 000 maternal deaths occurred worldwide from pregnancy and its complications which is equivalent to 830 mothers dying every day (more than 1 life lost every 2 minutes) in 2015. Nearly, all of these deaths are preventable in nature if appropriate interventions are taken [21]. Worldwide most maternal deaths do not have well-defined causes, but nearly 73.0 percent of all maternal deaths were attributable to direct obstetric causes; deaths due to indirect causes accounted for 27.5 percent (95 percent confidence interval 19.7–37.5) of all deaths. The major causes of maternal mortality are as follows: Hemorrhage, 27.1 percent (95 percent confidence interval 19.9–36.2); more than 72.6 percent of deaths from hemorrhage were classified as postpartum hemorrhage, Hypertension, 14.0 percent (95 percent confidence interval 11.1–17. 4), Sepsis, 10.7 percent (95 percent confidence interval 5.9–18.6), Abortive outcomes, 7.9 percent (95 percent confidence interval 4.7–13.2), Embolism and other direct causes, 12.8 percent [22].
Hypertensive Disease
Women in pregnancy or the puerperium can suffer from preeclampsia, eclampsia, and chronic hypertension. Eclampsia and preeclampsia tend to occur more frequently in the second half of pregnancy; less commonly, they can occur up to six weeks after delivery. Medication can alleviate the symptoms and their negative effects, but the only cure is expedited delivery. The etiology of the condition remains unclear but the overall aggregate prevalence rate of preeclampsia and eclampsia was 6.7 % (95 % CI = 5.8 %–7.6 %) [23].
Obstetric Hemorrhage
Women can experience anomalous or excessive bleeding because of an early pregnancy loss, a placental implantation abnormality, or an abnormality in the process of childbirth. The systematic review by Creswell and others finds a global prevalence of 0.5 percent for placenta Previa (95 percent confidence interval 0.4 percent to 0.6 percent (27). An equivalent systematic review for placental abruption has not been published, but most papers on this condition suggest an approximate prevalence of 1 percent [24]. WHO indicates that every year around 14 million mothers in the world suffer from vaginally bleeding following delivery. Based on world health organization data, probability of maternal mortality caused by postpartum hemorrhage is 1 in 1000 deliveries in developing countries, including Ethiopia. Moreover; all most all (99%) of maternal mortality due to vaginal bleeding following delivery occur in low- and Middle-income countries (29). World health organization reported that hemorrhage is the first leading case of maternal mortality globally [25]. Two different studies which were done in Jima and Kersa revealed that postpartum hemorrhage was the first leading cause of maternal mortality which accounts for 54% and 46.5% maternal mortality respectively [26].
Comorbidity
The study found that the indirect causes of maternal death, when combined, are the most common cause of maternal death. A breakdown of deaths due to indirect causes suggests that more than 70 percent are from preexisting medical conditions, including HIV/AIDS, exacerbated by pregnancy. The proportion of deaths due to indirect causes was highest in Southern Asia, 29.3 percent (95 percent confidence interval 12.2 percent to 55.1 percent), followed by Sub-Saharan Africa, 28.6 percent (95 percent confidence interval 19.9 percent to 40.3 percent); indirect causes also accounted for nearly 25.0 percent of the deaths in the developed regions. The overall proportion of HIV/AIDS maternal deaths is highest in Sub-Saharan Africa, 6.4 percent (95 percent confidence interval 4.6 percent to 8.8 percent) [27]. When they are expecting their first baby or when they have had many pregnancies, when they live far away from health facilities, or when they do not benefit from support from their families and friends. The risk of maternal deaths has two components: the risk of getting pregnant, which is a risk related to fertility and its control or lack of control; and the obstetric risk of developing a complication and dying while pregnant or in labor. The obstetric risk is highest at the time of delivery. The determinants of these risks share many similarities, but also have specific characteristics [29].
The accessibility and availability of good quality family planning and legal abortion services are key determinants of maternal mortality in many LICs. Quantitative models suggest that preventing pregnancy with contraception has a bigger role to play in reducing maternal mortality than does inducing abortion when pregnant with an unintended pregnancy [15]. The WHO health system building blocks offer a starting point for classifying health system determinants and include the following:
Quality of service delivery and referral system, Number, distribution, and training of the providers required, including midwives and obstetrician-gynecologists, Completeness and responsiveness of the health information system, including the adequacy of the Maternal Death Surveillance and Response, Ease of access to essential medications, such as magnesium sulphate, misoprostol, and oxytocin, and the supplies necessary for blood transfusions [2].
Antenatal care (ANC) from a skilled provider is important to monitor pregnancy and reduce morbidity and mortality risks for the mother and child during pregnancy, delivery, and the postnatal period (within 42 days after delivery). Urban women were more likely than rural women to have received ANC from a skilled provider (90 percent and58 percent, respectively) and to have had four or more ANC visits (63 percent and 27 percent, respectively). The percentage of women who used a skilled provider for ANC services and who had four or more ANC visits for their most recent birth in the five years preceding the survey increases greatly with women’s education. Among women with no education, 53 percent obtained ANC services from a skilled provider and 24 percent received four or more ANC visits compared with 98 percent and 73 percent, respectively, of women with more than a secondary education. The use of ANC services by a skilled provider and proper number of ANC visits also increases steadily with household wealth [3].
Conceptual framework
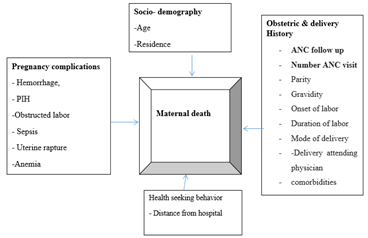
Maternal death is believed to be influenced by different factors such as Socio-demographic factor, pregnancy complications, obstetric and delivery history, health seeking behaviour.
Figure 1: Conceptual framework for the study on determinants of maternal mortality in WURH and Nekemte specialized hospital, 2022.
Objectives of the Study
General objective
To identify determinants of maternal mortality in government hospitals in Nekemte town from September 2017-August 2022 G.C., Nekemte, Eastern Wallaga, Oromia Region, Ethiopia, 2015 E.C.
Specific objectives
To identify the Socio-demographic determinants of maternal mortality in government hospitals in Nekemte town from September 2017-August 2022 G.C. To identify the obstetric related determinants of maternal mortality in government hospitals in Nekemte town from September 2017-August 2022 G.C.
Methods
Study area and Period
The study was conducted at Nekemte specialized hospital and Wallaga university referral hospital which are located in Nekemte town. Nekemte town is located 328 Km from Finfinne in the western direction, East Wallaga Zone, Oromia regional state, Ethiopia. WURH is one of the teaching hospitals found in western part of the country that runs under Wallaga University and serves catchment population of about 14 million and is located 12km west of Nekemte city on the way to Ghimbi and NSH is one of the oldest public hospitals found in western part of the country that runs under Oromia Regional state. Currently the hospital serves as referral site and provides specialized care for the western parts of Ethiopia. Services provided at both hospitals include: internal medicine, surgery, obstetrics and gynecology, pediatrics, outpatient services, emergency & intensive care, Cancer treatment and Orthopedics. The study was conducted from November 19-24, 2022 G.C on among charts of women who visited for utilization of antenatal, delivery and to 42 days postpartum, from September 2017 —August 2022 G.C.
Study Design
Institution based unmatched case–control study was used.
Source Population
All charts of mothers who visited WURH and Nekemte specialized hospital (NSH) for utilization of antenatal, delivery and to 42 days postpartum, from September 2017-August 2022 G.C.
Study Population
Cases: Mothers who died during pregnancy, delivery and 42 days after delivery at WURH and NSH from September 2017-August 2022 G.C. those with fully registered variables.
Controls: Alive mothers who visited WURH and NSH for utilization of antenatal, delivery and to 42 days postpartum, from September 2017 —August 2022 G.C. those with fully registered variables.
Study unit
Selected case and controls that are with fully registered variables
Inclusion Criteria
All mothers who died during their maternity period and control which came for utilization of antenatal, delivery and to 42 days postpartum, and survived.
Exclusion criteria
Cases and controls that are registered on the log book but whose charts were missed Charts that didn’t include the assessment of admission and status of mother (dead or alive) during discharge was excluded from the study.
Sample size determination
Sample size was determined using Epi Info version 7.2.5.0 considering the following assumptions: 95% CI, 80% power, 1 case to 3 control ratios (1: 3), percent of controls represented as 45.42%, and Odds ratio of 2.594 taken from unmatched case-control study done at Borena Zone, Oromia Region, Ethiopia [28] in which variables of (Place of residence, Husband’s education, Parity, ANC attendance and Place of delivery) were included with place of residence providing largest sample size. So, a total of 216 (54 cases and 162 controls) sample size was determined.
Sampling procedures
Charts of both cases (all charts of mothers who died during pregnancy, delivery, and up to 42 days after delivery in WURH and NSH from September 2017-August 2022 G.C. and controls (all charts of mothers who visited WURH and NSH for maternal health service utilization from September 2017-August 2022 G.C. and survived were selected from delivery ward, maternity wards, gynaecology, intensive care unit and operation theatre. Individual cases and controls fulfilling the inclusion criteria were selected retrospectively from the most recent death (for cases) and control until the determined Sample size is achieved. For each selected case, three controls which are nearby to the cases were selected. If controls are more than three, simple random sampling. i.e., Lottery method was used. Charts that had missing values of more than 30% were replaced by immediate candidates. When cases are replaced the control group is also replaced with controls nearer to cases. The first case was identified from registration book from respective wards and all cases that fulfil the inclusion criteria were included in the study.
Study Variables
Dependent Variable
Maternal death
Independent Variables
Mothers Socio demographic character, Age, Religion, Residence, Distance of residence, Obstetric and delivery history, Parity, Gravidity, Duration of Labour, Mode of delivery, Delivery attending physician, Obstetric complication, comorbidity
Operational definitions
Cases: Mothers who died during pregnancy, delivery and 42 days after delivery those with fully registered variables.
Controls: A live mothers who visited WURH and NSH for utilization of antenatal, delivery and to 42 days postpartum those with fully registered variables.
Presence of co morbidity = the presence of at least one medical disease was considered.
Prolonged labour = duration of labour more than 24 hours.
Direct obstetric death-results from obstetric complications of pregnancy, like from Haemorrhage, sepsis, and hypertensive disorders (pre-eclampsia/eclampsia). Co-morbidities - results from pre-existing disease (e.g., diabetes, cardiac disease, malaria, tuberculosis, HIV or a new disease that develops during pregnancy and is unrelated to pregnancy-related conditions, but is aggravated by the physiologic effects of pregnancy.
Data collection and Quality assurance
Data was collected by using a structured data collecting checklist adapted from Maternal Death Surveillance and Response Technical Guidelines of Ethiopia. It consists of socio-demographic data, obstetric and delivery history, presence of commodities, cause of death, antenatal and intra-natal risks, and presence of complications and was collected from medical record chart. Three midwives were recruited and trained. The training covers: the contents of the tool, ethical considerations and way of extraction of necessary information from chart. One supervisor, monitor and follow data collection while the principal investigator supervised the overall data collection process. To assure the quality of data pretest was performed on 5% of the samples at before data collection was begun. Every day, the filled checklists were reviewed and checked for completeness and consistency with close supervision.
Data processing and analysis
Data was edited for accuracy, readability, consistence and completeness; thereafter it was coded and entered into Epi Info version 7.2.5.0 and exported to SPSS 20 computer software programs for cleaning and descriptive analysis. Bi variate logistic regression analysis was done & variables with p-value less than 0.25 were transferred to Multivariate analysis & variables with P-value less than 0.05 were considered as statistically significant & AOR with 95% CI was used to control for possible con founders & to interpret the result, model adequacy was assessed using Hosmer–Lemeshow goodness-of-fit tests and p-value > 0.05 was taken as the model fits the data. Finally, the results were summarized & presented by using tables, graphs & charts
Ethical consideration
Prior to data collection, ethical clearance was obtained from the Ethical Review Committee of WURH NSH. In order to establish anonymous linkage only the codes, and not the names of the participant from the chart, was registered on the checklist.
Results
A total of 54 cases (died women) and 162 controls (survived women) were included in this study. Variables such as, educational status, marital status, occupation, ANC follow up and income were included in the checklists but they are incomplete in 99% of charts: As a result, they were excluded from the analysis.
Socio-demographic and related factors
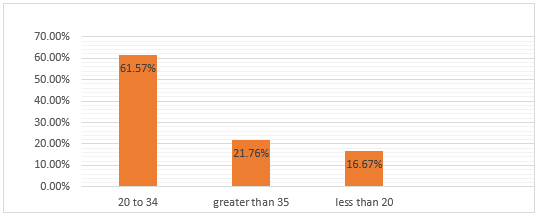
Age distribution
Majority, 133 (61.57%) of women in this study were in the age group of 20-34 years. While the least, 36 (16.67%) age group were age less than 20 years old. Of all women included in this study 33 (61.11%) of deaths were from among 20 to 34 years’ age group, while those of age group less than 20 years’ account for the least number 8(14.81%).
Figure 2: Age distribution frequency of mothers during their maternity in Gov’tal hospitals in Nekemte town from Sep.2010 to Aug.2014 E.C
Although 41(75.93%) of cases were from rural area, only 75 (46.58%) of controls were from rural areas. Twenty-five (46.3%) of cases came from 51-150km distance whereas 66 (40.74%) controls came from same distance.
Obstetric and delivery history
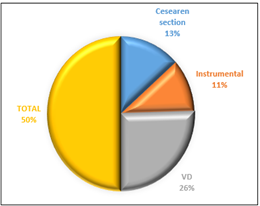
Regarding to obstetric and delivery history, 122 (56.48%) were gravid 2-5 and 59 (27.31%) were Primigravida. Similarly, 56.79% and 55.56% of the controls and cases were gravid 2 to 5 respectively. Eighteen (33.33%) of cases and only 24, (14.81%) of controls were lasted for more than 24hrs on labour. Out of all women included in this study 110 (50.93%) delivered by SVD and majority of them were attended by midwives. But ninety-three (57.41%) of controls and 20 (37.04%) of cases delivered by vaginal delivery and Cesarean section respectively.
Figure 3: Frequency distribution of mode of delivery of mothers at WURH and NSH from September 2017=August 2022 G.C.
Obstetric complications
Ninety-six (59.6%) of controls and only 3 (5.56%) cases have no obstetrics complications. Majority of women, 34 (28.57%) with obstetrics complication have obstetric haemorrhage (of which APH and PPH are predominant causes followed by pregnancy induced hypertension which accounted for 23.53%. From among cases with obstetric complication 18(33.96%) have obstetric haemorrhage while 27.27% of controls have pregnancy induced hypertension. Anemia accounts for the least complications in both groups.
Table 1: Frequency Distribution of Obstetric History of Women on Study Done At WURH And NSH From September 2017-August 2022 G.C.
| Variables | Categories | Controls (N= 162) | Case (N= 54) | Total(N=216) |
| Gravidity | Primigravida | 45(76.27%) | 14(23.73%) | 59 |
| 2-5 | 92(75.41%) | 30(24.59%) | 122 | |
| >5 | 25(71.13%) | 10(28.57%) | 35 | |
| Parity | Para-0 | 5(50%) | 5(50%) | 10 |
| Primipara | 11(84.6%) | 2(15.38%) | 13 | |
| 2-5 | 65(75.58%) | 21(24.42%) | 86 | |
| >5 | 3(50%) | 3(50%) | 6 | |
| Duration of Labor in hrs | <3hrs> | 0 | 1 | 1 |
| 4-24hrs | 138(79.77%) | 35(20.23%) | 173 | |
| >24hrs | 24(57.1%) | 18(42.9%) | 42 | |
| Mode of delivery | SVD | 93(84.55%) | 17(15.45%) | 110 |
| Instrumental | 31(64.52%) | 17(35.42%) | 48 | |
| Caesarean section | 38(65.52%) | 20(34.48%) | 58 | |
| Attending Health Professional | MW | 86(86.87%) | 13(13.13%) | 99 |
| Senior | 44(64.71%) | 24(35.29%) | 68 | |
| Others | 30(63.83%) | 17(36.17) | 47 |
Figure 4: Obstetrics complications at governmental hospitals in Nekemte town from September 2017-August 2022 G.C.
Bi variate analysis was used to assess association between various factors and maternal death. Factors which have association with maternal death (p value less than 0.25) were; age 20-34 years, living in rural area, Distance from the hospital, mode of delivery, presence of obstetrics complications, para 2-5, prolonged labour for more than 24hrs, delivery attended by seniors and others, and presence of co-morbidities. Several factors which were found not to have a significant association with maternal death were; age less than 20 and greater than 34 years, urban residence, primi gravida and primi para, para -zero, gravidity and parity, greater than five, duration of labour less than 24 hours and precipitated labour, having anemia, OL, uterine rupture and Malpresentation. In bi variate analysis, those variables having p- value less than 0.25 were further analysed in multi variate logistic regression.
Table 2: Bi Variate Analysis of Factors Associated with Maternal Death on Study Done at WURH And NSH From September 2017-August 2022 G.C.
| Variables | Categories | Controls (N=162) | Case (N= 54) | Total (N=216) | COR (95 % CI) |
| Age in Years | <20> | 28(77.7) | 8(22.3) | 36 | 0.46(0.16, 1.35) |
| 20-34 | 100 (75.2) | 33(24.8) | 133 | 1.49 (1.20, 4.22) | |
| >34 | 34(72.3) | 13(27.7) | 47 | 1 | |
| Residence | Rural | 75(64.5) | 41(35.5) | 116 | 6.6 (0.14, 0.65) |
| Urban | 86(86.9) | 13(13.1) | 99 | 1 | |
| <10> | 16(76.2) | 5(23.8) | 21 | 1 | |
| Distance From NSH in Km | Nov-50 | 62(78.5) | 17(21.5) | 79 | 0.53 (0.25, 1.11) |
| 51-150 | 66(72.5) | 25(27.5) | 91 | 0.41 (0.20,0.84) | |
| >150 | 18(72) | 7(28) | 25 | 0.72 (0.18, 2.84) | |
| Primigravida | 45(76.3) | 14(23.7) | 59 | 1 | |
| Gravidity | 02-May | 92(75.4) | 30(26.6) | 122 | 2.21 (1.21, 6.31) |
| >5 | 25(71.4) | 10(28.6) | 35 | 1.87 (0.82,4.26) | |
| Para-0 | 24(75) | 8(25) | 32 | 1 | |
| Parity | Primipara | 24(80) | 6(20) | 30 | 0.45(0.12,1.58) |
| 02-May | 101(73.7) | 36(26.3) | 137 | 32.02 (6.45,82.03) | |
| >5 | 13(76.5) | 4(23.5) | 17 | 1.21 (1.06,5.76) | |
| Duration of Labor in hrs | <24> | 138(79.3) | 36(20.7) | 174 | 1 |
| >24 | 24(57.1) | 18(42.9) | 42 | 1.69(0.622,4.602) | |
| VD | 93(84.5) | 17(15.5) | 110 | 1 | |
| Mode of delivery | Instrumental | 31(64.6) | 17(35.4) | 48 | 0.39 (0.18,0.82) |
| Caesarean section | 38(65.5) | 20(34.5) | 58 | 0.46 (0.24,0.90) | |
| Attending Health Professional | MW | 86(86.9) | 13(13.1) | 99 | 2.709(0.939,7.82) |
| Senior | 44(64.7) | 24(35.3) | 68 | 0.35 (0.19,0.66) | |
| Others | 30(63.9) | 17(36.2) | 47 | 4.452(2.541,7.80) | |
| Hemorrhage | 16(47) | 18(58) | 34 | 5.6(0.5, 53) | |
| PIH | 96(99) | 01(1) | 97 | 1.27 (1.14 ,5.27) | |
| Anemia | 1(50) | 1(50) | 2 | 0.48(0.15, 1.45) | |
| Obstructed labor | 9(60) | 6(40) | 15 | 0.74 (0.45, 3.77) | |
| Malpresentation | 4(80) | 01(20) | 5 | 2.55 (0.32, 20.30) | |
| Sepsis | 04(40) | 06(60) | 10 | 0.27 (0.14,0.53) | |
| Uterine Rupture | 436.4) | 7(63.6) | 11 | 5.6(0.59, 53.3) | |
| Comorbidity | 3(25) | 9(75) | 12 | 18.5(3.6, 93.6) | |
Further analysis with logistic regression was done to identify the factors that are independently associated with maternal mortality. Determinants of Maternal Death were; Being in the age group of 20 -34 is risk than being in the age group of >34. Women in the age group of 20 – 34, have 2.05 times risk than being in the age group of >34 for maternal death (OR 2.05, 95% (1.02, 5.54)). Women who midwives attended their deliveries were more likely to die 2.709 times than those who were attended by seniors (AOR 2.709,95%CI (0.939,7.82)). Women who lasted for more than 24 hours are more likely to die 1.69 times than those lasted for 3 to 24 hours (AOR 1.692, 95% CI (0.622,4.602)). Women who came from rural area are more likely would die 6.6 times than women who came from urban area (OR 6.615, 95% CI (0.14, 0.562). Women having gravid and para 2-5 more likely would die 2.21 and 32.01 times than the others respectively with (OR=2.21, 95% CI 1.21, 6.31) & OR=32.01, 95% CI (6.45, 82.03). Women who had uterine rupture were 5.625 times would more likely to die than women who have obstetric haemorrhage (OR 5.625,95% CI (0.593,53.377)). Women who had comorbidity were 18.458 times more likely they would die than women who didn’t have co morbid diseases. (OR= 18.458, 95% CI (3.639, 93.615).
Table 3: multi variate of factors associated with maternal mortality in study at WURH and NSH from September 2017-August 2022 G.C.
| Variables | Categories | Controls | Case | Total | COR (95 % CI) | AOR (95 % CI) |
| Age in Years | 20-34 | 100(75.18) | 33(2481) | 133 | 1.49 (1.20, 4.22) | 2.05 (1.02,5.54) |
| Residence | Rural | 76(64.95) | 41(35.04) | 117 | 6.6 (0.14, 0.65) | 5.45(1.34, 22.08) |
| Gravidity | 2-5 | 92(75.40) | 30(24.59) | 122 | 2.21 (1.21, 6.31) | 2.21 (1.21,6.31) |
| Parity | 2-5 | 101(73.72) | 36(26.27) | 137 | 32.02(6.45,82.03) | 2.01(1.36,6.34) |
| Duration of Labor in hrs | >24 | 24(57.14) | 18(42.85). | 42 | 1.69(0.622,4.602) | 3.39(2.15, 5.21) |
| Attending Health Professional | midwife | 30(63.83) | 17(36.16) | 47 | 2.709(0.939,7.82) | 2.49(3.15,5.13) |
| Hemorrhage | Yes | 16(47.05) | 18(52.94) | 34 | 5.6(0.5, 53) | 2.19(1.03,6.33) |
| PIH | Yes | 18(64.28) | 10(35.71) | 28 | 1.27 (1.14 ,5.27) | 1.27(1.01,3.13) |
| comorbidity | Yes | 159(77.94) | 45(22.05) | 204 | 18.5(3.6, 93.6) | 1.28(2.17,16.61) |
Discussion
Most (96.3%) of the maternal deaths were due to obstetrics determinants in which haemorrhage was the leading cause followed by PIH, which is consistent with studies done in different countries, as well as Ethiopia. A systematic review done on causes of maternal death in Ethiopia shows nearly 92.4% of all maternal deaths between 1990 and 2013 were due to direct obstetric causes(38). Haemorrhage was the leading direct cause of maternal death worldwide, representing 27.1% of maternal deaths, similarly 25.7 % of direct maternal death was due to haemorrhage in Ethiopian between 1990 and 2013. In this finding, haemorrhage was about 38.5% (OR=1.91, 95% CI (0.33, 2.27)) which is almost similar with worldwide as well as study done at national level. In Ghana, haemorrhage accounts for 22.8% of maternal mortality, which is nearly similar with our finding [33]. PIH accounts for (14.0%) (14)(25)(20) of direct cause worldwide and a systemic review done in Tanzania showed that death from hypertensive disorders of pregnancy accounts for 20% which is slightly higher than our current study findings. In Ethiopia, PIH accounts 10.3% of maternal death, also the study conducted at Tigray Ayder hospital and JUSH reveals 19.2% and 19% of maternal death respectively, which is slightly greater than current study. This is might be due to low ANC follow up as well as they present after complication developed [34,32,33].
The study done in Tigray region of Ayder hospital showed other direct causes of maternal death like Sepsis (13.5%), Anemia (8%), uterine rupture (7%), OL (16%) as well as study done at JUSH reveals Sepsis (14. %), Anemia (28.3%), Uterine rupture (23.3%) and OL (34.17%). According to our study Sepsis, Anemia, Uterine rupture and OL accounts 21.15%, 1.9%, 7.69% and 9.62% respectively. The result of our finding showed that sepsis is also other leading cause of maternal death only preceded by haemorrhage which might be due to late presentation after home delivery and low post-natal care and follow up [34, 38]. Associated factors touched in this study were age group, residence area, distance from the hospital, mode of delivery, as well as delivery attending professionals. The study done in Tanzania Shenyang national hospital in 2014 showed most deaths (74.5%) occurs in age group of 20 – 34(38). Also According to EDHS 2016 the most commonest age group of maternal death were 20-34 (88%) (16). Likewise, study done in Tigray region of Ayder hospital and JUSH showed that most deaths (55%) and (52,5%) were respectively occur in age group of 20 – 34 which is similar in terms of affected age groups with this study (74.3%)(24)(26). Our study differs only in percentage when compared to other studies which might be due to sample size. Most death occurred in this age groups which is more risk than being in the age group of greater than 34 years. Women in the age group of 20 – 34 has increased the risk of maternal death by 2.127 times (OR 2.127, 95% (0.374,12.102)). [16, 20, 33, 38]
Regarding obstetric history, the study done in Tanzania and Kenya in 2014 showed that the women who were gravida and para 2-5 accounted for 42.5% & 49% respectively. As well a systemic review done in MizanTepi Hospital & JUSH showed that most maternal death were in gravid and para 2-5 which accounts (26.4%) and (24.8%) respectively [20, 34, 38,42]. Similarly, in our study most deaths occur in women with gravid & para 2-5 respectively (55.6%, 66.7%). This might be due over representation of this category. The study done in Tanzania shinyanga regional hospital in 2014 showed that 60% of women who came from rural area were died. Likewise study done in JUSH showed 75.8 % women who came from rural area were died (14)(23). Similarly, in our study more than three fourth (75.9%) with OR= 6.615, 95% CI (0.140, 0.582)) women who died came from rural area. This might be because of women who came from rural area are at higher risk than who came from urban women. These imply that women who live in rural area are poor at utilization of maternal health services which might be due to different reasons like lack of awareness or inaccessibility or unavailability of maternal health services.
The study done in Ayder Hospital showed most of mothers (44.5%) who were died came from distance of 51-150 km, where as in JUSH most mothers (40%) who were died came from 11-50km. According to our current study most deaths (46.3%) were from 51-150km which is similar with study done at Ayder Hospital. [33, 34] A review in JUSH and MizanTepi Hospital showed most maternal death (54.9%) and (37.3%) respectively had length of labor > 24hrs, but in this study most of deaths (64.8%) had labor that had lasted for less than 24hr which might be due to under reporting of time elapsed from time of onset of labour to presentation to the hospital. Prolonged labour (>24hrs), is the other most risk factor for maternal death [20, 34]. When the duration of labor is 24 hour or more, the mother is 2.96 times more likely would die than women who had less than 24-hour duration of labor with (OR= 2.96, 95% CI (1.45,6.04)).
Regarding mode of delivery, study done in Tanzania reveals that almost half of maternal death occurred following SVD. But a review in JUSH and MizanTepi hospital in Ethiopia showed (46%) and (36%) of maternal death occurred following cesarean delivery respectively. Our finding (37.4%) is similar with JUSH and MizanTepi hospitals in which the most deaths occurred in women who gave birth by cesarean section [36][34] [38]. This may be due to associated complications. Regarding birth attendants, study done in Tigray region reveals majority of deaths occurred in those attended by midwifes (38.7%), whereas 25.8% and 6.5% maternal deaths occurred in those who were attended by Seniors and Others respectively [6]. Other study done in JUSH indicates from total maternal deaths 91.3% were attended by doctors, only 8.7% were attended by other health professionals [14]. Our current study shows that from total maternal deaths, half (44.4%) of death occurred in those attended by seniors, whereas 31.5% and 24% were attended by other professionals and midwives respectively. When compared with the studies done in Tigray region and JUSH, death was high in those attended by seniors which is might be due to late consultation and attendance of complicated cases.
Most (75.93%) of maternal deaths were occurred in post-partum period which is nearly similar with the finding in JUSH in which 68% of maternal death occurred in the post-partum period. However, the study from maternity hospital of Nigeria shows about 61.9% of the maternal deaths occurred in post-partum period which is lower than this finding. This might be because of small sample size and shorter study period which is only 84 maternal deaths and two years respectively [20, 35]. Higher number of maternal deaths in post-partum period implies that the management following delivery and during delivery might be poor. Prolonged period of labor due to OL or due to not having timely intervention might contribute a lot for death occurring in post-partum period. The second period in which higher number of deaths occurred is the intra-partum period (14.81%). It is smaller than finding from JUSH which was 25%. But it is almost similar with the findings of maternity hospital of Nigeria which was 13.1% [20, 34]. In the maternity hospital of Nigeria, 25% of women died before reaching to intrapartum period but in our set up antepartum death is only 9.26%, which is almost similar with JUSH (7%). This is might be due to high prevalence of death associated with abortion in Nigeria, which is opposite to our current findings. The other reason might be due to dramatic reduction of maternal death related with abortion due to the introduction of misoprostol or safe mother hood services in our country [20, 34]. These implies that the proper care during antenatal period reduce home delivery, intra-partum period and after abortion save the lives of many women in antenatal and intrapartum period. The implication of these findings is, management after terminating pregnancy might be poor or the women might not utilize postpartum care service.
Problem faced, strength and Limitation of study
Problem faced
Poor registration
Poor documentation of charts and log books
Registration of different age for a single person
Unreadable hand writings
Not writing women on the day of admission and discharge on the log books
Not writing discharge summary sheet
Strength of study
Free of recall bias
Study design-case control is preferable for rare event like maternal death and for determining associated factors.
Limitation of study
Selection bias due to intentional selection of controls
Does not observe effect of some of socio demographic variables like economy, education…due to 99% missing of socio demographic variables.
Wider confidence interval-due to rarity of events and lower sample size.
Conclusion
Most of the women died in the postpartum period, mainly because of direct obstetric causes, of which Haemorrhage was the leading cause of death and followed by sepsis and PIH. Being age group 25-34 years, gravida and para 2-5, coming from rural area, prolonged labour and delivery attended by midwives and others are the main determinants factors for maternal death.
Recommendation
To decrease the number of maternal death multi-sectorial collaboration is important. Everybody starting from a single individual to the higher officials and organizations has a responsibility to alleviate the problem. Based on the findings from this study the following recommendations are made:
1. To East Wallaga zonal health department:
It should follow, monitor and evaluate IEC/BCC provided by woreda health offices and health institutions to increase awareness of the community in rural part of area about complications of pregnancy and strengthen the referral system to avoid delay in intervention or to avoid prolonged labour.
2. To WURH and NSH:
NSH and WURH should strengthen service provision to reduce death in intra-partum period and post-partum period (particularly after operative delivery) and to avoid prolonged labor.
NSH and WURH should improve the registration system of events and place for the placement of patient charts.
3. To health professionals:
Health professionals should have to improve timely intervention given for women and Early consultation of cases requiring senior interventions
4. To HEWs:
They should have to improve awareness of the rural community about pregnancy
complications and simultaneous co morbidities.
5. To academicians and researchers:
They should dig out associated socioeconomic factors for maternal death
They should respond, why most women who came from rural area would die most as compared to urban? Why most women would die in post-partum period?
Abbreviations and Acronyms
ANC : Antenatal care
EDHS : Ethiopia demographic & household’s survey
HIV : Human Immune Deficiency syndrome
ICD : International Classification of Disease
JUSH : Jimma University specialized Hospital
LBs : Live births
LICs : Low-income countries
MDG : Millennium Development Goal
MMR : Maternal Mortality Ratio
NSH : Nekemte Specialized Hospital
OL : Obstructed Labor
PIH : Pregnancy Induced Hypertension
SDG : Sustainable development goal
WHO : World Health organization
WURH: Wallaga University Referral Hospital
References
- Rafiq S, Syed W, Ghaffar SF. (2019). Trends and causes of maternal mortality in a tertiary care hospital over five years: 2013-2017. Pak J Med Sci., 35(4):1128-1131.
Publisher | Google Scholor - Who E, Bank TW. (2013). Trends in Maternal Mortality: 1990 to 2013.
Publisher | Google Scholor - Report KI. Federal Democratic Republic of Ethiopia Demographic and Health Survey.
Publisher | Google Scholor - Ahmed S. (2014). An Assessment of Dhs Maternal Mortality Data And Estimates Dhs Methodological.
Publisher | Google Scholor - Who E, Group WB. (2015). Trends in Maternal Mortality: 1990 to 2015.
Publisher | Google Scholor - Health C. Maternal mortality and associated factors:2012 to 2014.
Publisher | Google Scholor - Bayray A, Gebrehiwot h. (2013). Patterns of maternal mortality and associated factors; a case- control study at public hospitals in tigray region, ethiopia, 2012.
Publisher | Google Scholor - Tegene Legese, Misra Abdulahi, and Anteneh Dirar. (2016). Risk Factors of Maternal Death in Jimma University Specialized Hospital: A Matched Case Control Study. American Journal of Public Health Research, 4(4):120-127.
Publisher | Google Scholor - Yaya Y, Lindtjorn B. (2012). High maternal mortality in rural south-west Ethiopia: estimate by using the sisterhood method.
Publisher | Google Scholor - Lemi Kumela, Temesgen Tilahun, Demeke Kifle. (2020). Determinants of Maternal Near Miss in Western Ethiopia. Ethiop J Health Sci., 30(2):161.
Publisher | Google Scholor - Gaym A. (2009). Maternal mortality studies in Ethiopia-Magnitude, causes and trends.
Publisher | Google Scholor - Who E, Group WB. (2015). Trends in Maternal Mortality: 1990 to 2015.
Publisher | Google Scholor - Tessema et al. (2017). Trends and causes of maternal mortality in Ethiopia during 1990–2013: findings from the Global Burden of Diseases study 2013. BMC Public Health, 17:160.
Publisher | Google Scholor - Gerdts C, Tunçalp O, Johnston H, Ganatra B. (2015). Measuring abortion-related mortality: challenges and opportunities. 10-12.
Publisher | Google Scholor - EDHS. Ethiopia. 2016.
Publisher | Google Scholor - Who E, Bank TW. (2013). Trends in Maternal Mortality: 1990 to 2013.
Publisher | Google Scholor - Berhan Y, Berhan A. (2014). Review of Maternal Mortality in Ethiopia: A Story of the Past 30 Years Review Review of Maternal Mortality in Ethiopia: A Story Of The Past 30 Years. 2-14.
Publisher | Google Scholor - WHO. (2015). Trends in maternal mortality: 1990 to 2015: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, Geneva, Switzerland.
Publisher | Google Scholor - Legese T, Abdulahi M, Dirar A. (2016). Risk Factors of Maternal Death in Jimma University Specialized Hospital. A Matched Case Control Study, 4(4):120-127.
Publisher | Google Scholor - FMO. (2015). Health Sector Transformation Plan 2015/16 - 2019/20. Finfinne, 98.
Publisher | Google Scholor - Legesse T, Misra Abdulahi AD. Trends and causes of maternal mortality in Jimma University specialized hospital, southwest Ethiopia: a matched case–control study. Int J Women’s Health, 2017; 9:307.
Publisher | Google Scholor - Tesfaye G, Loxton D, Chojenta C, Assefa N, Smith R. (2018). Magnitude, trends and causes of maternal mortality among reproductive aged women in Kersa health and demographic surveillance system, eastern Ethiopia. BMC Women’s Health, 18:198.
Publisher | Google Scholor - Abdella A. (2015). Maternal Mortality Trend in Ethiopia.
Publisher | Google Scholor - Jarso etal, (2019). Determinants of Maternal Death in a Pastoralist Area of Borena Zone, Oromia Region, Ethiopia: Unmatched Case-Control Obstetrics and Gynecology International.
Publisher | Google Scholor - Yaya Y, Data T, Lindtj B. (2015). Maternal Mortality in Rural South Ethiopia: Outcomes of community-based birth registration by health extension workers, 1(430):1-17.
Publisher | Google Scholor - Ababa A. (2014). Federal Democratic Republic of Ethiopia Ministry of Health Maternal Death Surveillance and Response (MDSR) Technical Guideline.
Publisher | Google Scholor - Benova L, Cumming O, Campbell OMR. (2014). Systematic Review Systematic review and meta-analysis: association between water and sanitation environment and maternal mortality. 19(4):368-387.
Publisher | Google Scholor - Girma S, Gizachew A, Ismael K. (2019). Maternal Mortality and its Determinants among Women Utilized Obstetrics and Gynecologic Services in Asella Teaching and Referral Hospital. Oromia Region, Ethiopia. 2018. Curre Res Diabetes & Obes J. 2019; 10(3): 555788.
Publisher | Google Scholor - Mapunda OE, Msuya SE, Kapologwe NA, John B, Damian DJ, Mahande MJ. Assessment of Maternal Mortality and its Associated Causes at Shinyanga Regional Hospital in Tanzania Assessment of Maternal Mortality and its Associated Causes at Shinyanga Regional Hospital in Tanzania. 2016;(October).
Publisher | Google Scholor - Teka H, Zelelow YB. (2018). Comprehensive A, Hospital S. A 3 years review of maternal death and associated factors at ayder comprehensive spcialized hospital. Northern ethiopia abstracT. 10(3):38-45.
Publisher | Google Scholor - Legese T, Mulatu K, Kahsay T. (2016). Trends and Determinants of Maternal Mortality in Mizan-Tepi University Teaching and Bonga General Hospital from 2011-2015: A Case Control Study Study area and period. iMedPub Journals, 1-8.
Publisher | Google Scholor - Paine GM. (2019). Maternal Mortality in Nigeria: A Literature Review. 11(1):83-94.
Publisher | Google Scholor - Submitted T, The TO, Studies P. (1999). Partial IN, Of F, Requirements THE, et al. Morbidity in kenya.
Publisher | Google Scholor - Negussie D, Gedlu NM. (2014). Review of maternal death in Jimma university specialized hospital review of maternal in 2014.
Publisher | Google Scholor