Research Article
Decisive Guidelines for Keeping the Heart Attacks on The Sidelines
1.University Institute of Pharmaceutical Sciences, Panjab University, Chandigarh, India.
2.President, APSE, Pharmacology Division, Department of Pharmaceutical Sciences, Guru Jambheshwar University of Science and Technology, Hisar, India.
*Corresponding Author: Milind Parle, Pharmacology Division, Department of Pharmaceutical Sciences, Guru Jambheshwar University of Science and Technology, Hisar, India.
Citation: S Kaur, M Parle. (2023). Decisive Guidelines for Keeping the Heart Attacks on The Sidelines. International Clinical and Medical Case Reports, BioRes Scientia Publishers. 2(2); DOI: 10.59657/2837-5998.brs.23.018
Copyright: © 2023 Milind Parle, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 07, 2023 | Accepted: July 31, 2023 | Published: August 10, 2023
Abstract
A heart attack is usually a shocking event that compels the victim to modify his lifestyle considerably out of fear of death. Cardiovascular disorders have burdened developed and developing nations with increased mortality and morbidity rates. High cholesterol levels increase atherosclerosis risk, resulting in heart attacks, strokes, and chronic kidney disease. There are many ways to reduce the risk of heart disease, although one can't change some risk factors, such as family history, age, or gender. Cessation of tobacco use, reduction of salt in the diet, eating more fruits and vegetables, regular physical activity, avoiding alcohol, and stress management have been shown to reduce the risk of cardiovascular disease. Our small choices every day have a tremendous cumulative impact on cardiovascular health. Social determinants like poverty, housing insecurity, low education, and lack of insurance can adversely influence one's cardiovascular health. One must not fear fatality if one lives a happy, healthy, and peaceful life. A personalized approach that considers individual differences in genes, metabolism rate, presence of other diseases, and lifestyle is likely the most effective strategy in reducing the risk of precipitating heart attacks. A heart-friendly diet, regular physical activity, quitting alcohol, smoking cessation, and keeping blood pressure in the normal range are effective measures to prevent heart attacks. In light of the above, the authors have recommended valuable guidelines to laymen for keeping heart attacks on the sidelines in this fascinating and helpful article.
Keywords: heart attack; atherosclerosis; cardiac arrest; exercise; nutrients
Introduction
A heart attack may be looked upon not as a death sentence but as a wake-up call alarming the patient and his family to follow a healthy lifestyle. The heart is essential for survival and plays a fundamental role in supplying nutrients and oxygen to various body parts. The menace of suffering from a heart attack, the world's foremost cause of mortality, can be averted by adopting a heart-friendly lifestyle. The term “cardiovascular diseases" (CVDs) refers to disorders impairing the efficient pumping of blood by the heart's ventricles owing to multiple pathological conditions in various body parts, including the myocardium itself. A heart attack can be a lifechanging experience that affects the individual and his loved ones. However, it can also serve as a powerful reminder to prioritize one's health and well-being. Considering the high prevalence of deaths from heart attacks in India and worldwide, the authors have recommended valuable guidelines in this fascinating review article to prevent fatal consequences due to cardiovascular diseases and to protect a healthy heart.
Prevalence
Global Scenario: Cardiovascular diseases (CVDs) are the leading cause of death worldwide. CVDs are a group of disorders of the heart and blood vessels, including coronary arteries, cerebrovascular disease, rheumatic heart disease, and stroke. More than four out of five CVD deaths are due to heart attacks, and one-third of these deaths occur prematurely in individuals aged from 20 to 70 years. Cardiovascular diseases (CVDs) alone take around 17.9 million lives each year all over the globe. Over 75% of CVD deaths occur in low- and middle-income countries where raised blood pressure is among the most critical risk factors for CVDs. High blood pressure prevalence is 56% for black adults, 48% for white adults, 39% for Hispanic adults, and 46% for Asian adults. (Centre for Disease Control and Prevention, 2022).
U.S. Scenario
Heart disease is the leading cause of death for men, women, and people of most racial and ethnic groups in the United States of America, including African American, American Indian, Alaska Native, Hispanic, and white men [1]. In the United States, someone has a heart attack every 40 seconds. Every year, about 805,000 people in the United States have a heart attack [2]. Of these, 605,000 persons face a heart attack for the first timeand200,000 patients have already suffered heart attacks. About 1 in 5 heart attacks are silent, wherein the damage has already been done, but the patient is unaware of it. About 695,000 people died in the United States from heart disease; out of these, coronary heart disease killed 375,476 people in 2021.
Over 60 million women (44%) in the United States live with heart disease. Heart disease is the leading cause of death for women in the United States and can affect women of any age. In 2021, Heart attack was responsible for the deaths of 310,661 women (about 1 in every 5 female deaths) in the United States. About 1 in 20 adults aged 20 years and older suffer from coronary artery disease (CAD) in the U.S. [2]. Therefore, The U.S. population is expected to have clinical evidence of cardiovascular disorder in 45.1% (more than 130 million people) by 2035 [4,5].
Indian Scenario
The results of the worldwide study on disease burden indicated that India has a higher myocardial mortality rate of 272 per 100,000 people in comparison to the rest of the world's mortality rate of 235 deaths [3]. Indians are genetically more prone to develop heart attacks, and adopting the Western lifestyle has further increased the risk. Hypertension, diabetes mellitus, dyslipidemia, smoking, obesity, sedentary lifestyle, psycho-social stress, vehicular and air pollution, stress, heavy workout, intake of steroids, and low intake of fruits and vegetables are the factors contributing to increasing cases of heart attacks among youngsters in India. CVDs strike Indians a decade (10 years) earlier than the Western population. CVDs such as ischemic heart disease and cerebrovascular diseases such as stroke account for 17.9 million deaths all over the globe per year, and India accounts for one-fifth of these deaths involving the younger population as well. The prevalence of CAD is 21.4% for diabetics and 11% for non-diabetics in India. The bulk of CAD in rural parts of the country is nearly half of the urban population. CVDs account for 45% of Indian deaths in the 40–69-year age group. Within India, the rates of CVD vary markedly from one state to another, with the highest prevalence in the states of Kerala, Punjab, and Tamil Nadu. However, the exact recent prevalence data remains to be compiled and documented.
Types of Cardiovascular Diseases
Hypertension
According to WHO, the diagnosis of hypertension (high blood pressure) is confirmed when the pressure in blood vessels is 140/90 mm Hg or higher on two different days. Blood streaming through the arteries pushes it against their walls, creating a force. A blood pressure of 120/80 mm Hg is considered normal. The first number, 120 mm of Hg (Systolic), represents the pressure against the walls of blood vessels while the heart is contracting, whereas the second number, 80 mm of Hg (Diastolic), represents the pressure against the walls of blood vessels, while the heart is at rest (relaxing) between the two beats. Symptoms of hypertension include severe headache, dizziness, difficulty in breathing, chest pain, and abnormal heart rhythm. There are different stages of
hypertension:
Normal Blood Pressure: When the systolic blood pressure varies from 110-125 mm Hg, and the diastolic pressure varies from 70-85 mm Hg, it is considered in a normal range.
Elevated Blood Pressure: One is said to have elevated blood pressure when the systolic readings range between 125-135 mm Hg, and the diastolic pressure varies from 85- 89 mm Hg. This can be managed by changing the unhealthy lifestyle.
Stage-I Hypertension (Mild): One is said to have mild hypertension (Stage-I) when the systolic reading consistently ranges between 125-139 mm Hg and the diastolic between 85-89 mm Hg. Lifestyle changes can control this stage of hypertension without any medication.
Stage-II Hypertension (Moderate): When the systolic reading is at least 140 mm Hg or higher, and the diastolic reading is 90 mm Hg or higher, one is diagnosed with moderate hypertension (Stage-II). Antihypertensive medicines (Table 1.) are required for these patients.
Stage-III Hypertension (Severe): When the diastolic blood pressure exceeds 100mm Hg, one suffers from severe hypertension. Vital antihypertensive medicines (Table 1.) and hospitalization in a few cases are recommended.
High blood pressure can be divided into two categories, i.e., primary and secondary hypertension. Primary hypertension, also known as essential hypertension, has no definite cause. There are many risk factors like obesity, old age, genetics, high-salt diet, sedentary lifestyle, tobacco smoking, and frequent drinking of alcohol. It accounts for 90% of the cases. Secondary hypertension is caused by underlying medical conditions like diabetes, thyroid conditions, sleep apnea, adrenal gland tumors, congenital blood vessel diseases, and kidney or liver impairment. It is less common and accounts for 5-10 % of cases. This hypertension occurs suddenly and can be attributed to non-cardiac pathological conditions. Appropriate measures to control hypertension prevent heart attack, stroke, and kidney damage.
Myocardial Infarction (MI)
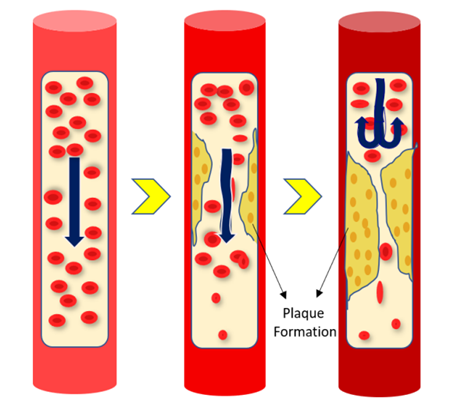
MI occurs due to the reduction or cessation of blood flow to a section of the heart, which results in ischemia and, consequently, the necrosis of heart tissue (muscle). It is caused when the blood flow supplying oxygen to the walls of the cardiac muscle is obstructed, and a few sections of the heart muscle do not receive enough oxygen. This could be due to the blood clot formed in the epicardial artery, which supplies oxygen to the heart muscle. The leading causes of myocardial infarction [6] are i. Obstructed blood flow to the heart due to atherosclerotic plaques (complex, sticky substances composed of fat), ii. Narrowing of coronary arteries (Fig. 1) and iii. Thromboembolism (when a blood clot interferes with the smooth blood flow) resulting in myocardial ischemia. Myocardial infarction (MI), despite significant advancements in therapy, is still a severe illness with substantial morbidity and fatality rates.
Figure 1: Narrowing of an Artery Due to the Development of Plaques.
Heart Attack
A heart attack is caused by a partial or complete blockage of the coronary artery, which supplies nutrients to the heart. Cholesterol deposits along the walls of the arteries that supply blood to the heart and the narrowing/spasm of coronary arteries under pathological conditions form the main reasons causing a heart attack. Blood flow and, consequently, oxygen supply to the heart is diminished when a plaque gets deposited along the walls of a coronary artery (Fig. 1). A blood clot is formed when a plaque in the arteries ruptures. The clot formation further restricts the regular supply of nutrients through the oxygenated blood to the heart. Heart failure occurs when the blood supply to a portion of the heart is wholly discontinued.
Atherosclerosis
The accumulation of fats, cholesterol, and other chemicals along the artery walls is called atherosclerosis. These deposits, called atheromatous plaques, narrow down the lumen of the arteries and hinder the smooth blood flow to the heart (Fig. 1).
Angina Pectoris
Angina pectoris occurs when there is a decreased blood supply to the heart muscle due to the narrowing of the coronary arteries. Palpitation, chest pain, tightness in the chest, shortness of breath, shoulder/back pain, sweating, fatigue, or dizziness constitutes the typical description of angina symptoms.
Stable Angina: It results from coronary obstruction caused by atherosclerosis. Predictable but persistent pain that subsides with rest or nitroglycerine and worsens with exercise exists instable angina.
Unstable Angina: An uncommon condition that results from atherosclerosis with a blood clot. Symptoms worsen and become more frequent, which cannot be eased by rest or nitroglycerine. This condition is also known as Pre-infarction Angina or Crescendo Angina.
Intractable or Refractory Angina: Intractable or Refractory Angina is marked by severe or incapacitating chest discomfort.
Variant Angina (also known as Prinzmetal's Angina): Variant angina is characterized by pain at rest accompanied by reversible ST-segment elevation. It is believed to be brought on by coronary artery vasospasm. Artery spasm is caused by the contraction of the smooth muscle of the blood vessel wall rather than directly by atherosclerosis. No underlying blockage is present, which can cause a heart attack if prolonged.
Arrhythmia
Cardiac arrhythmia is a pathological condition wherein the heart beats irregularly and follows an abnormal rhythm. Deviation from the regular pattern of cardiac rhythm is known as arrhythmia. It can either cause the heart to beat slowly (known as bradycardia), rapidly (known as tachycardia), or irregular heartbeat.
Congestive cardiac failure (CCF)
CCF is a recurrent condition called chronic heart failure, which hampers the effective pumping of oxygenated blood by the heart's left ventricle to support other body organs. Fluid congestion in and around the heart, lungs, and other tissues. The left ventricle becomes stiff and loses its ability to contract as well as relax fully.
Symptoms of Heart Attack
A heart attack or stroke is the first indication of an invisible illness having its roots in damaged blood vessels. Initial signs could be a mild discomfort that worsens into a painful condition. The center of the chest, the arms, the left shoulder, the jaw, or the back may all experience pain or soreness because of a heart attack. The individual may also become pale, have a cold sweat, experience trouble in breathing, feel sick, dizzy, or faint. Women are more likely than men to experience back or jaw discomfort, difficulty in breathing, shoulder or abdomen discomfort, dizziness, and vomiting. The discomfort from a heart attack may often be misleading, particularly in women, and feel more like indigestion. Symptoms like unexplained anxiousness, nausea, dizziness, palpitations, and cold sweats could be present even without pain. Unexpected tiredness may come before heart attacks in women. Women also frequently experience fatal first heart attacks that are more serious than men. Most heart attack symptoms last at least 30 minutes and are not alleviated by rest or oral medicines. A "silent" myocardial infarction (MI) is a type of heart attack in which a person experiences no signs or symptoms until the diagnosis. People with diabetes experience heart attacks due to MI more frequently. While some heart attacks begin suddenly and intensely, others begin gradually with only minor pain or distress.
Diagnosis
Cardiovascular Disorders often require a battery of diagnostic tests. These tests may vary depending on the individual’s symptoms, medical history, and physical examination.
Electrocardiogram (ECG or EKG): A rapid and painless test called an electrocardiogram captures the heart's electrical activity. If the heart is pounding too quickly or too slowly, or if the heart anatomy is uneven, ECG can help uncover these structural abnormalities. Furthermore, the electrical signals' timing and intensity help in the early diagnosis of heart attacks, angina, arrhythmias, myocardial infarction, etc.
Sphygmomanometer: Sphygmomanometer is a medical device used to measure blood pressure. Blood pressure measurement is critical in assessing and managing a person's overall health.
Cardiac Immunoassay (CIA): Cardiac biomarkers found in human body fluids are accurate and suitable predictors of the risk and development of cardiovascular diseases. Based on antigen-antibody immuno-affinity, these biomarkers are detectable and quantifiable using a variety of cardiac immunoassays. Cardiac biomarkers offer several benefits in predicting and diagnosing cardiovascular disorders, such as high sensitivity, quickness, affordability, and non-intrusive nature. Lengthynon-coding ribonucleic acid, proteins, miRNA, messenger ribonucleic acid, corticotrophin-1, galectin-3, endoglin, atrial natriuretic peptide (ANP), brain natriuretic peptide (BNP), as well as other molecules, makeup biomarkers.
Molecular Imaging: In clinical practice, molecular imaging is a frequently used symptomatic technique for diagnosing cardiovascular diseases. Standard imaging techniques include photoacoustic tomography, magnetic resonance imaging, computed tomography scanning, positron emission tomography, and single photon emission computed tomography.
Echocardiography: Echocardiography is a non-invasive imaging technique of the preferred choice for diagnosing and monitoring cardiovascular diseases. For the vast bulk of cardiovascular disorder subtypes, it is reliable. With the advent of modern echocardiographic techniques, such as real-time 3-Dimensional echocardiography, strain rate imaging, and speckle tracking, the cardiac ultrasound's capacity to assess cardiovascular disorder's anatomy and physiology has significantly improved. Additional testing techniques include blood tests, electrocardiograms, angiograms, nuclear scintigraphy, and conventional radiography, which employs X-rays.
Nanotechnology-Based Cardiac Immunoassay: Several cutting-edge methods, including magnetic resonance imaging, optical imaging, nuclear scintigraphy, multimodal imaging strategies, Electro chemiluminescence Immunoassay (ECL), Photo electrochemical sensor, Surface-enhanced Raman scattering, Surface plasmon resonance, and Enzyme-linked immunosorbent assays, are used to precisely identify biomarkers for various types of heart disorders. A method for early-stage cardiovascular disorder detection may involve combining nanotechnologies with cardiac immunoassays. Nanotechnologies have the potential to mitigate non-specific binding sites, give elevated effectiveness of cardiac target binding, and provide excellent signal amplification.
Electro chemiluminescence Immunoassay (ECL): Electro chemiluminescence can be employed as a typical diagnostic procedure for assessing the expression of biomarkers since the intensity of the observed emission is proportional to the concentration of the biomarker’s level. Light emissions and excited states are generated because of electron transfer processes in electro chemiluminescence.
Enzyme-Linked Immunosorbent Assay: A commercially available technique called (ELISA) employs a conjugation with an enzyme and a substrate to monitor the color of antigen-antibody interactions to determine the concentration of targets.
Photo electrochemical (PEC) Sensors: Photoactive materials absorb photons after illumination and produce electron-hole pairs. Photo electrochemical sensors have the potential to rapidly detect the biomarkers associated with a damaged heart.
Causes & Risk Factors
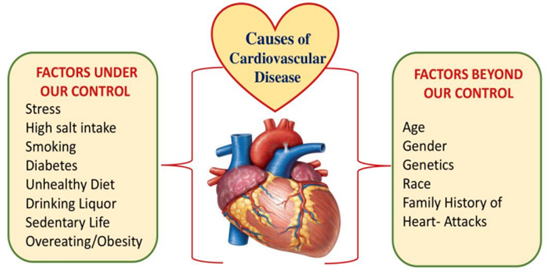
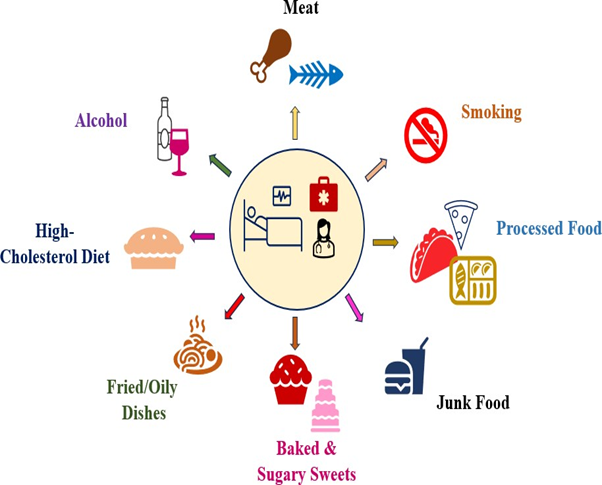
There are several factors responsible for cardiovascular diseases. They are divided into two categories, such as: under our control or beyond our control (Figure 2) factors. Coronary artery disease risk is increased with advancing age and family history of the disease, and men are more likely than women to suffer from it. As we age, we have a higher chance of developing clogged arteries. A strong connection exists between heart disease and diets rich in saturated fats, salt, sugar, and bad cholesterol. Excessive stress might damage the arteries and increase the risk of a heart attack. A sedentary lifestyle, obesity, smoking, alcohol, bad eating habits, uncontrolled hypertension, high harmful cholesterol levels, diabetes, and unrelieved stress are the risk factors (Fig. 2) responsible individually or jointly for causing a heart attack.
Figure 2: Causes of Cardiovascular Disease.
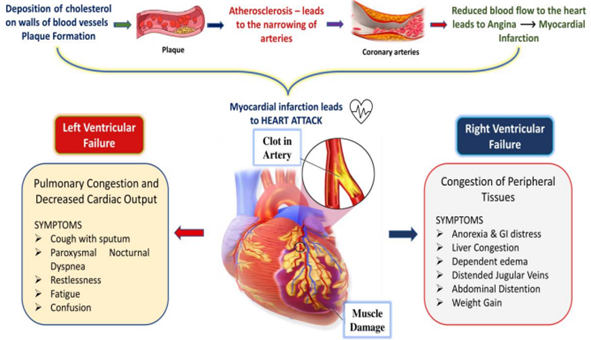
Pathophysiology
A catastrophic medical disease called a heart attack is brought on when the blood flow to any part of the heart is blocked. Often, blood flowing through an artery is obstructed due to the accumulation of fat, cholesterol, or other compounds known as plaques (Fig. 3). Angina Pectoris is a condition characterized by severe chest pain that frequently spreads to the chest, limbs, and neck and is brought on by a lack of blood flow to the heart. Ischemia occurs when an area of cardiac tissue is deprived of oxygen-rich blood. Myocardial infarction occurs when the heart muscle is starved of oxygen/nutrients and suffers severe damage resulting in necrosis. A heart attack manifests due to atherosclerotic plaque build-up in the artery, compromising the oxygen supply to the heart muscle. A patient may feel the pain just below the heart and right above the stomach and get confused, attributing the pain to indigestion. This starts a heart attack, where a clot grows and blocks two-thirds of the artery. Pain starts radiating towards the left arm and sends signals to the brain. The brain, in turn, releases adrenaline, and the heartbeat increases while the clot keeps growing. As a result, the problem gets worse because the myocardial muscles pump more forcefully and demand more energy for survival. The cardiomyocytes start rupturing and release structural proteins (troponins) into the bloodstream. The heart becomes weak and cannot maintain the oxygen demand leading to dyspnea (Fig. 3). The starving heart muscle cells either die or rupture. Over time, a process known as hypertrophy occurs in which the heart gets enlarged to meet the increased metabolic demands. If not treated within 15-20minutes, the heart begins to get damaged, and its normal rhythm cannot be restored because five hundred cardiomyocytes are lost every second. Left-sided heart failure weakens the left side of the heart, reducing the ability of the heart to pump blood into the body. Oedema in the legs, ankles, and liver occurs when the right side of the heart is weak because of fluid retention in the arteries. To minimize heart damage, the blocked artery needs to be opened as soon as possible. Clogged or restricted arteries can be opened to facilitate the normal with a minimally invasive treatment called angioplasty. The doctor identifies the narrowed blood artery using angiography [7].
Figure 3: Pathophysiology of Heart Attack.
Complications
In rare circumstances, the causative factors of angina (or a heart attack) are mysterious and cannot be attributed to conventional reasons such as a constriction of the artery, an embolus in the coronary artery, or a heart valve dysfunction. A heart attack may lead to the following complications necessitating instant hospitalization:
Arrhythmia (Irregular Heartbeat): After a heart attack, electrical signals may be disrupted by injured cardiac muscles, causing one’s heart to beat irregularly. The heart beats too quickly, slowly, or irregularly due to faulty signaling. Arrhythmia symptoms include chest pain, palpitations, tiredness, and shortness of breath. Other arrhythmias can be fatal such as. Total Heart Block, in which electrical signals from one side of the heart cannot be transmitted to the other, prevents the heart from pumping the blood effectively, and ii. Ventricular arrhythmia, in which the heart starts to beat more quickly before contracting fully and going into abrupt cardiac arrest. 48 hours following a heart attack, these fatal arrhythmias can be a substantial cause of death. Medications (Table 1.) like beta-blockers are beneficial for treating mild arrhythmias. To treat more severe bradycardias, an artificial pacemaker may become the need of the hour.
Myocardial Infarction: Myocardial infarction occurs when blood flow to a portion of the myocardium is reduced or ceased altogether. The heart muscle gets damaged extensively if appropriate steps are not taken in time to improve blood flow. A Heart attack is also known as “myocardial infarction,” in which “death of a part of the heart muscle occurs. The signs and symptoms include chest pain, fatigue, heartburn, nausea, shortness of breath, and dizziness. Within three hours of the commencement of a heart attack, appropriate steps need to be initiated to dissolve the arterial blockage as soon as possible with the help of thrombolytic or clot-dissolving medications such as tissue plasminogen activator, streptokinase, or urokinase as a life-saving measure.
Heart failure: Heart failure occurs when the heart cannot efficiently circulate blood throughout the body. If the heart muscle of the left ventricle is severely damaged by a heart attack, cardiac arrest may occur. Because of fluid accumulation, heart failure signs and symptoms include breathlessness, weariness, and swelling in your arms and legs. The primary therapies include surgical procedures, implanted medical equipment, medicines to manage heart rhythm and healthy lifestyle adjustments.
Cardiogenic Shock: Severe cardiac muscle injury causes the whole body to go into shock. This uncommon ailment occurs when the heart's ability to pump blood is suddenly and unexpectedly compromised. Some signs are mental haziness, frigid fingers and toes, decreased desire to pee or no need to pee at all, rapid heartbeat, pale skin, and breathing difficulties. Vasopressors (also known as inotropes), which raise blood pressure and improve blood circulation, may sometimes help under careful medical supervision.
Heart Rupture: When the heart's muscles, walls, or valves rupture after a heart attack, it is a severe but uncommon condition known as a heart rupture. The signs and symptoms are identical to those of cardiogenic shock. Typically, the only way to fix the problem is through open-heart (bypass) surgery.
Inflammation of the sac-like tissue surrounding the heart (pericarditis): An unfavorable immunological response can occasionally be brought on by a heart attack. Post-myocardial infarction syndrome, Dressler syndrome, or post-cardiac injury syndrome are some names for this illness.
Cardiac Arrest: Cardiac arrest is the sudden cessation of a heartbeat. Sudden cardiac arrest results from an abrupt alteration in the heart's signals. Heart attacks increase the likelihood of one dying from this illness, which poses a significant threat to life. Every heart attack potentially would bring about fatal consequences (sudden cardiac death) if not addressed immediately by an expert cardiologist. Treatment includes beta-blockers (Table 1.), coronary artery bypass surgery, angioplasty, and an implantable cardioverter defibrillator.
Aneurysm: An aneurysm develops when the arterial wall weakens and the artery bulges. The leading cause of an aneurysm is enhanced pressure on the walls of an artery. Symptoms depend on the area where it develops. Brain aneurysm leads to eye strain, headache, speech difficulties, and numbness on one side of the face. Abdominal aneurysm leads to lower back pain, abdominal pain, and a pulsating sensation in the belly. A ruptured aneurysm requires immediate surgery, whereas an unruptured one might not require invasive treatment.
Pulmonary edema: Pulmonary edema is when fluid accumulates in and around the lungs, making breathing difficult. Symptoms of pulmonary edema include coughing with blood, difficulty in breathing, increased heartbeat, fatigue, and fluid retention. Treatment includes diuretics, anti-anginal drugs (Table 1.), oxygen therapy, and a low-sodium diet.
Stroke: When the heart is not functioning efficiently, blood clots are more likely to accumulate in the arteries. As soon as one of these clots obstructs an artery and stops the blood flow to the brain, an attack of stroke (ischemic stroke) is experienced. Symptoms of a stroke with ischemic brain damage include perplexity on the body's left side, numbness, difficulty speaking, and loss of coordination or balance. Treatment of stroke includes tissue plasminogen activators, blood thinning agents, anticoagulants, and angioplasty.
| HeartDisorder | Category | Medicines |
| Hypertension | Diuretics, Vasodilators, Potassium Channel Openers Nitric Oxide Releasers Dopamine Agonists Calcium Channel Blocking Agent Sympatholytics, Alpha Blockers, Alpha-2 Agonists Beta-1 Blockers, Angiotensin-converting enzyme Inhibitors, Angiotensin Receptor Blockers, Renin Blockers | Furosemide, Hydrochlorothiazide Hydralazine, Minoxidil, Diazoxide Sodium Nitroprusside, Hydralazine Fenoldopam Verapamil, Diltiazem, Nifedipine, Nimodipine Prazosin, Doxazocin, Barazocin, Alfuzocin, Silodosin, Tamsulosin Clonidine, Methyl dopa Atenolol, Metoprolol Enalapril, Ramipril, Lisinopril,Fosinpril, Benazepril, Trandolapril Losartan, Valsartan, Telmisartan, Candesartan, Olmesaratan Aliskiren, Remikiren, Enalkiren |
| Acute Heart Failure | Diuretics, Ionotropic Agents, Cardiac Glycosides, Ionodilators | Furosemide, Bumetanide, Dobutamine, Dopamine, Digoxin, Digitoxin, Stropanthin, Amrinone, Milrinone, Vesnarinone |
| Congestive Heart Failure | Vasodilators Angiotensin Converting Enzyme Inhibitors Blockers of the Angiotensin Receptor Aldosterone, Antagonists Beta Blockers, Vasopeptidase Inhibitors | Hydralazine, Minoxidil, Nifedipine Enalapril, Ramipril, Lisinopril Losartan, Valsartan, Telmisartan, Candesartan Spironolactone, Epleronone Carvedilol, Metoprolol, Bisoprolol, Atenolol Sampatrilat, Omapatrilat, Fasidotril |
| Angina Pectoris | Nitrates Calcium Channel Blockers Beta Blockers Potassium Channel Openers Sodium Channel Blockers Partial Fatty Acid Oxidation Inhibitors | Nitroglycerine, Isosorbide dinitrate Verapamil, Diltiazem Propanolol, Atenolol, Carvedilol Nicorandil Ivabradine Trimetazidin, Ranolazine |
| Myocardial Infarction | Beta Blockers Alpha Blockers, Thrombolytics Platelet Inhibitors, ACE Inhibitors Coronary dilators Statins, Narcotic Analgesics | Metoprolol, Atenolol, Prazosin Streptokinase, Alteplase Aspirin, Clopidogrel Enalapril, Ramipril, Lisinopril Nitroglycerine, Atorvastatin Pentazocine, Buprenorphin |
| Arrhythmia | Class 1 Sodium channel Blockers, Class 2 Beta Blockers, Class 3 Potassium channel Blockers, Class 4 Calcium Channel Blockers, Class 5 Miscellaneous Drugs | Flecainide, Lignocaine, Quinidine, Esmolol, Metoprolol, Sotalol, Amifampridine, Ampyra, Dalfampridine, Firdapse, Ruzurgi, Dofetilide, Ibutilide, Verapamil, Diltiazem, Digoxin, Adenosine, Magnesium, Atropine |
Table 1: Classification of Drugs for Heart Disorders.
Nutritional Management
Background
Start Taking Care of Your Heart Before It Falls Apart. Nutritional therapy is a type of healthcare that uses nutrition to promote health and treat medical conditions. The therapy may necessitate dietary changes, nutritional supplements, and other interventions to optimize nutrient intake and support overall health. Allopathic medicines have many side effects and are expensive. Lifestyle modifications, including healthy dietary patterns, have been shown to reduce the risk of cardiovascular disorders and improve the prognosis in those individuals suffering from chronic diseases. Consumption of food items that include processed foods, artificial sweeteners, and saturated/ trans fats has been associated with an increased risk of heart attacks.
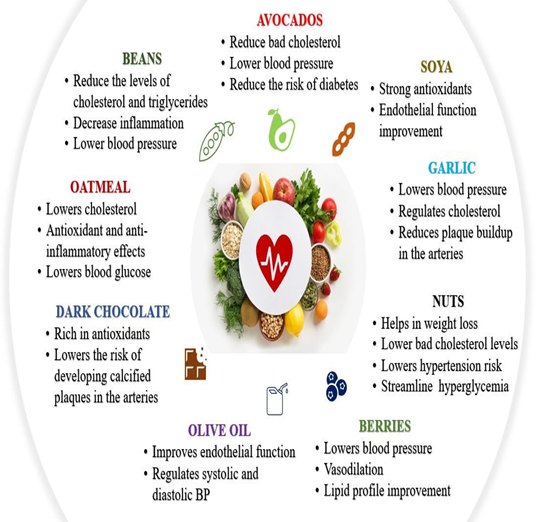
Heart-Friendly Nutrients
Berries: Anthocyanins, flavonols, and flavonoids are among the bioactive compounds found in berries called polyphenols, which safeguard the heart and blood vessels. According to numerous studies, they successfully decrease blood pressure, lower triglyceride levels, and rejuvenate blood vessel endothelium [8]. These heart-friendly nutrients (Fig. 4) help prevent blood clotting by significantly inhibiting platelet aggregation caused by adenosine-5′-diphosphate. Therefore, berries help the body avoid cardiovascular diseases by preventing platelet activation, regulating blood cholesterol levels, lowering oxidative stress, improving endothelial function, and managing metabolism [8, 9].
Avocados: Avocado is a vital tropical fruit that contains compounds known to reduce cholesterol, including mono-unsaturated fatty acids (MUFAs), flavonoids, polyphenols, tocopherols, plant-based sterols, and squalene. However, compared to hydrophilic compounds in the fruit, less attention has been paid to the antioxidant capacities of these lipid-soluble substances. The lipophilic extract of the fruit showed a more powerful antioxidant effect than its hydrophilic extract [10]. According to recent findings, avocado pulp, which contains acetogenic compounds, inhibited platelet aggregation, thereby preventing the development of thrombi [11].
Oatmeal: The consumption of whole grains positively impacts cardiovascular disorder-related morbidity and mortality. Cereals are consumed extensively in Mediterranean nations as well as other parts of the globe. Patients had a significantly lower chance of developing heart failure, stroke, and other cardiovascular disorders when they consumed 90 g or more of whole grains daily [11]. LDL and total cholesterol levels were reduced by eating whole grains due to the presence of dietary fiber. The favorable effects of dietary fiber are caused by the fact that it causes more bile acids to be excreted in feces, which reduces blood serum cholesterol levels [8]. Besides this, dietary fiber could lead to a loss of excess weight, which would reduce systolic and diastolic pressure levels. The WHO recommends consuming 27-40g of fiber daily because it has significant advantages, like improving blood flow and reducing body weight. It has been demonstrated that a healthy diet rich in dietary fiber reduces visceral fat accumulation, improves insulin sensitivity, lowers hypertension, and reduces bad cholesterol levels because it decreases cholesterol absorption from the gastrointestinal system [12].
Dark Chocolate: Flavanols found in chocolate, especially dark chocolate, has been shown to boost endothelial nitric oxide production, supporting vascular health by promoting vasodilatation and lowering blood pressure. Numerous studies have been done on the outcome of chocolate on cholesterol levels, with the reduction of atherogenesis and the LDL oxidative impact being the most likely mechanisms [13]. Additionally, dark chocolate consumption has been linked to decreased mortality and coronary artery disease (CAD) prevention. Chocolate consumption reduces the risk of heart failure, CAD, myocardial infarction, and hypertension. [14].
Soya: Soybeans are a major source of phytonutrients like flavonoids, sitosterol, and lecithin, as well as dietary fiber, saponins, and polysaccharides that may together or function in different ways to provide unique medical benefits [15]. Soya has been found to reduce the risk of high blood pressure mediated through vasodilatation and repression of an essential enzyme that regulates blood pressure. Studies have proven that isoflavones decrease blood pressure by concentrating on vasodilatation-related processes [16]. Isoflavones boost endogenous nitric oxide production by interacting with the estrogen-responsive element of genes associated with vascular endothelial nitric oxide (NO) synthase, which improves carotid artery circulation [17].
Fruits and Vegetables: Lycopene, an unsaturated lipophilic carotenoid, is a pigment present in fruits and vegetables (Fig. 4), which are usually red, like tomatoes, papayas, and watermelons. Lycopene may reduce the chance of developing atherosclerosis by improving endothelial function (increases nitric oxide bioavailability and blood circulation) and lipid oxidation, especially in the initial stages of atherosclerosis. Lycopene may also lower blood pressure, improve metabolic profile (by reducing cholesterol synthesis), reduce the risk of atherosclerosis, and limit the synthesis of inflammatory biomarkers and aggregation of platelets [18]. Additionally, post-menopausal women benefit from dietary lycopene’s' beneficial effects on the cardiovascular system [19].
Olive Oil: In the Mediterranean diet, olive oil serves as the primary supply of vegetable fat. Oleic acid represents the topmost mono-unsaturated fatty acid (MUFA) present in the diet, exhibiting beneficial effects on the heart and brain. The bioactive components in olive oil reduce oxidative stress and enhance endothelial function, thereby decreasing the likelihood of atherosclerosis due to their profound anti-inflammatory, antioxidant, and anti-thrombotic actions. Oleuropein and hydroxytyrosol, both strong antioxidants and enzyme modulators, are olive oil's main phenolic substances [20]. When olive oil is consumed, the production and levels of circulating inflammatory indicators related to atherosclerosis decline, and systolic and diastolic blood pressure levels in hypertensive and normotensive individuals improve [21].
Nuts: Nuts (Fig. 4), particularly peanuts and walnuts, have been shown to lower cardiovascular disorder-related morbidity and mortality in numerous big prospective cohort studies. In addition to being a great source of PUFAs, particularly linoleic as well as alpha-linolenic acid, nuts are also abundant in nutritional fiber, nutrients such as calcium, selenium, potassium, micronutrients like folic acid, and other bioactive components (coenzyme Q10, phytosterols, and polyphenols). The effects of nut consumption on weight reduction, LDL-c levels, risk of hypertension, hyperglycemia, insulin resistance, and oxidative stress are all favorable. A 15% to 23% lowered risk of heart attack or stroke was linked to eating nuts like peanuts and walnuts. Nutty foods improve lipid and lipoprotein profiles, reduce oxidative stress and inflammation, and enhance endothelial function, which is the main mechanism by which they protect against cardiovascular disorders [22]. Flaxseed contains omega-3 fatty (alpha- linolenic acid) in abundant quantity. Numerous preclinical and clinical investigations have demonstrated the benefits of flaxseed supplementation for cardio protection. These benefits are attributed to the antihypertensive, anti-atherosclerotic (decreased cholesterol levels), and anti- inflammatory properties of flaxseed's bioactive ingredient [23].
Salmon: As intake of fish in the diet lowers the accumulation of pro-inflammatory cytokines, improves the function of blood vessel intima, lowers triglyceride levels, and reduces the aggregation of platelets, the occurrences of the formation of thrombus are inhibited [24]. Salmon have also been linked with reduced blood sugar levels, decreased blood pressure in the arteries, and better lipid profiles in the elderly population from the Mediterranean islands. They are also known to have a hypotensive effect, which is supported by numerous meta-analyses, and they have been acknowledged as a factor in lowering the chance of heart failure [25]. Vitamin D is also present in large quantities in various kinds of fish. The bioactive component present in fish is omega-3 fatty acid, which regulates the synthesis of adhesion molecules and pro-inflammatory mediators, which makes it an essential element in avoiding atherosclerosis [26]. Fatty fish is a wonderful dietary supply of coenzyme Q10, which is believed to be effective for patients in managing atherosclerosis, high blood pressure, and heart attack [27].
Garlic: Garlic inhibits both the oxidation of low-density lipoproteins and the liver's ability to produce cholesterol, which contributes favorably to the therapy of hypercholesterolemia. The first line of defense against dyslipidemia is diet, and many people with the condition turn to garlic as an alternative treatment to bring their elevated lipid levels back into the normal range [28]. Garlic also has blood pressure-lowering properties, which are linked to the generation of hydrogen sulfide, the amount of allicin released from alliin, and the activity of the enzyme alliinase, which is thought to have angiotensin II-inhibiting and vasodilating properties. In many countries, garlic is used as a remedy to lower blood pressure. Allicin and ajoene, components of garlic, also show anti-thrombotic properties via inhibition of platelet aggregation. Garlic also enhances fibrinolysis, the process of breaking down blockages due to clots and thrombi [29]. Although lowering lipid levels is how garlic primarily protects against cardiovascular disease, some studies suggest it improves endothelium function and produces arterial dilatation. By decreasing reactive oxygen species and enhancing glutathione production, allicin improved the antioxidant state [30]. Garlic also protects against cardiovascular disease by preventing LDL oxidation, which in turn prevents atherosclerosis of the vessels.
Sesame Seeds: An individual with heart disease should use sesame seed oil with reduced saturated fat content. Sesame seeds contain extremely high concentrations (up to 2.5%) of furfural lignans, primarily sesamin, sesamolin, and glucosides, which have advantageous metabolic effects. Sesamin and sesamolin are transformed during preparation into the polyphenol antioxidants such as sesamol and sesaminol. These compounds help reduce high blood pressure and cholesterol, resulting in increased levels of vitamin E. Phytosterols found in sesame nuts have been linked to lower levels of bad cholesterol in the blood by preventing absorption and reducing cholesterol synthesis in animal studies [31].
Figure 4: Heart-Friendly Nutrients
Nutrients Harmful to The Heart
Processed Food: Salt, unhealthy fats, and added sugar are common ingredients in processed foods. These components cause oxidative stress and inflammation, damaging blood vessels and raising the risk of cardiac disorders. Obesity, elevated blood pressure, and high cholesterol are all indicators of cardiovascular disease and can be brought on by these unhealthy substances. Deli ham, tuna fish, turkey, bologna, chicken, hot dogs, pâté, bacon, sausage rolls, and salami harm the heart. The excessive quantities of salt and preservatives contained in processed meats are contributing heavily to the problem of heart disorders. Bacon has a significant amount of saturated and trans-fat, which increases LDL cholesterol [32].
Red Meat: Overeating pork, mutton, lamb, beef, and other meats may increase the risk of heart disease primarily because they contain trans and saturated fats, which can heighten cholesterol levels. Cholesterol increases the number of fatty plaques deposited along blood vessel walls, making blood flow more difficult. The levels of chemical trimethylamine N-oxide (TMAO) produced by gut microbes (a side product of digestion) have been found to rise with a red meat-heavy diet, which in turn increases cholesterol deposits in arterial walls and promotes platelet aggregation, raising the risk of thromboembolism and stroke [33].
White Rice, Bread, and Pasta: White rice, bread, and pasta are customarily prepared from white flour, thereby losing their healthy fiber, vitamins, and minerals. Refined grains quickly get converted into sugar, which is then stored as fat in the body, potentially leading to heart disease. White rice, as opposed to brown rice, is a refined carbohydrate that gets digested and absorbed, leading to insulin resistance, high blood sugar levels, and elevated levels of triglycerides and LDL cholesterol. White rice is low in fiber and has a high glycemic index which can contribute to free radical damage and inflammation [34].
Fried Foods: Fried foods comprise a high amount of saturated fat, further promoting plaque deposits in arteries gradually, putting an individual at risk for coronary artery disease and a heart attack. Food's nutritional content changes when fried since water is lost and fat is absorbed. During frying, the oil used for cooking the food degrades, becomes oxidized, and gets hydrogenated, resulting in the loss of unsaturated fats and increased trans fats. Frying food certainly adds calories, which will sooner or later lead to weight gain and damage to the artery walls. These damaged areas in the blood vessels develop plaques over time, thereby narrowing the artery lumen and reducing the oxygen supply to the brain, resulting in stroke attacks [35].
Smoking: A well-established risk factor for all cardiovascular diseases is tobacco smoking. Smoking (Fig. 5) forms a crucial factor that often determines the likelihood of survival or death of the individual facing a heart attack. The nicotine content in tobacco causes an increase in heart rate, blood pressure, and serum homocysteine levels, which is thought to result in vascular damage. Smoking is typically responsible for the gradual development of atherosclerosis, and myocardial inflammation, which results in impaired heart contractility and arrhythmias. Smoking also increases blood carbon monoxide levels, decreasing blood's ability to carry oxygen to tissues. Carbon monoxide (C.O.) present in smoke reacts with hemoglobin to generate carboxyhemoglobin, which obstructs the smooth exchange of oxygen and carbon dioxide, thereby interfering with the process of purification of blood. Besides, smoking has also been reported to cause ventricular arrhythmias and coronary artery spasms [36]. Passive smokers are also at risk of developing cardiovascular disorders [37].
High Cholesterol Diet: Hypercholesterolemia reflects a high cholesterol level in the blood. Low-density lipoprotein (LDL) cholesterol is associated with an elevated threat of atherosclerosis and coronary heart disease by forming plaques that deposit along the artery wall, causing narrowing and blocking the blood flow. These plaques can even burst, resulting in blood clots [38]. Cardiovascular disease can be exacerbated by a high-cholesterol (Fig. 5) diet via a rise in LDL cholesterol and a fall in HDL cholesterol, increasing inflammation, contributing to obesity, and increasing the risk of diabetes. High cholesterol diet includes foods such as butter, cheese, processed snacks, full-fat dairy items, fried foods, baked goods, sweets, etc., [39].
Alcohol Consumption: Overindulgence in alcohol (Fig. 5) has detrimental effects on health, raising the risk of developing hypertension, fatty liver, and mortality from cardiovascular disease [40]. The quantity of alcohol consumed appears to be of utmost significance as far as the fatal influence of alcohol is concerned on heart function.
Figure 5: Nutrients Harmful to the Cardiovascular System.
Limitations of Nutritional Therapy
If one suffers from hypertension, one must take medicines regularly to keep blood pressure in a normal range. Nutrition therapy can help maintain the status quo but would not be of much help in the long run to control hypertension without allopathic medicines. Senior citizens and widowers at advanced age would face financial instability because of retirement. Such elderly individuals can rely on generic medications instead of expensive branded drugs. The active ingredients of branded and generic medicines are the same, evoking almost the same therapeutic effect. Branded drugs are usually costly. After all, they compensate for the expenses incurred by the company in the discovery process; the generic medicines are cheap because they are permitted to be manufactured by local firms after the expiry of the patent period. Every person is unique and requires different nutrients based on his lifestyle and culture. Therefore, one should follow dietary recommendations strictly to maintain a healthy heart. One should not resort to crash diets or fasting for many hours to lose weight or look slim because one may succeed in controlling one's body weight but would face a bigger challenge in lack of essential amino acids and deficiency of vitamins. There cannot be one nutrition package perfectly fitting to one and all individuals.
Lifestyle Measures to Prevent Heart Attack
A heart attack is often a life-changing experience for the patient and his loved ones. However, it also serves as a powerful reminder to prioritize health and well-being.
Exercise: Exercise has been proven to be an essential element for preventing cardiovascular disorders by minimizing the cardiovascular risk involved due to obesity, high blood pressure, hypertriglyceridemia, hyperglycemia, and systemic inflammation. Around 70% of Americans lead a physically inactive lifestyle, which exposes them to a higher risk of developing cardiovascular diseases (CVD) [41]. There are different types of exercises, like aerobic exercise, anaerobic exercise/strength training, and stretching. Aerobic exercise promotes circulation and transports more oxygenated blood to the heart. During aerobic exercise, a person breathes faster and deeper, carrying more oxygen to purify the blood. Aerobic exercises include running, cycling, jogging, dancing, walking, and swimming. It can be performed for a long duration and helps in developing stamina and endurance. Strength training exercise increases muscle strength. Anaerobic exercise does not require oxygen, while it uses already stored energy. It can be performed only for a short duration and helps in developing force. Anaerobic exercise includes sprinting, jumping, hill climbing, and weightlifting. Stretching activities improve peripheral circulation, posture, coordination, and stress management, which may lower the incidence of musculoskeletal injuries. Population-based educational camps and programs should be organized to encourage people to undertake an exercise schedule daily [42].
Physical Activity: We need to increase our day-to-day physical activity in addition to the organized exercise schedule. This paragraph is primarily devoted to Physical Activity and should not be banded together with a daily exercise schedule. Physical activity is related to daily household chores or other routine activities. Regular physical activity can reduce the risk of cardiovascular disease. Washing clothes, dressing, bathing, feeding, cleaning, sweeping the floor, climbing the stairs, walking, dancing, and many more can be included in daily physical activities. A sedentary lifestyle increases the risk of heart disorder. Home maintenance involves various physical activities that are beneficial to the heart. Commuting to the workplace daily with minimum use of a vehicle, engaging in outdoor games, doing heavy backyard work, cycling, jogging, gardening, moving briskly, and jumping can help in the healthy functioning of the heart. These activities improve blood flow from and to various body organs, including the myocardium.
Individual Domains: Human beings function broadly into five domains/Spheres, i.e., Natural Domain, Occupational Domain, Family Domain, Social Domain, and Personal Domain. The Natural domain/Environment includes seasonal changes, the impact of sunlight, altitude, unpolluted air, and greenery around [43]. The day/night cycle controls both cardiovascular health and well-being. Heart rate and blood pressure are at their lowest during the night-time and begin to rise before waking up. Sunlight exposure, physical activity, and eating habits change with the season, modifying the rate of metabolism and physiological systems of our body. The blood pressure, cholesterol, and glucose levels are higher in winter than summer. Sunlight exposure favors the cardiovascular system and promotes Vitamin D synthesis, which lowers blood pressure. Noise pollution, foul air, and hard water harm the cardiovascular system. Living in an artificial environment (air conditioners, heaters, false ceilings, etc.) reduces exposure to healthy natural resources, including sunlight, fresh air, animals, and plants. The Occupational domain comprises the work environment, the boss/controlling officer, work culture, office colleagues, organization targets, promotional prospects, and basic amenities like canteen and restroom/wash-room facilities. We spend most of our life in the occupational domain. Therefore, we must have a conducive and healthy environment in the workplace. Almost half of our stress stems from office targets, promotional prospects, and competitive and/or non- competent coworkers. The cooperative boss, supporting office colleagues, and healthy work culture make the occupational domain happy. Job satisfaction strengthens the feeling of well- being and has a favorable impact on overall health. The Family Domain includes spouses, children, parents, in-laws, and other close family members. The other half of life's stress comes from family members' expectations. It takes acrobatic feats, and we are always kept on our toes to maintain a smooth balance between the expectations of close family members and the office boss. A leading cause of a heart attack is a stressful lifestyle. On the other hand, a cooperative and supporting family has a significant role in maintaining a healthy heart and an effective pancreas that goes a long way in preventing heart attacks. The Social Domain includes social networks, relatives, colleagues, neighbors, and the friend circle. Social interaction with friends has a positive impact on cardiovascular health. A healthy and positive friend circle subconsciously helps in solving several personal problems and relieves stress to a large extent. Low socioeconomic status increases mortalities from heart attacks due to lacking basic amenities, essential commodities, and timely help. The Personal Domain includes hygiene, eating and sleeping habits, biological clock/circadian rhythm (disciplined life), hobbies, smoking, indoor and outdoor sports/games, alcohol intake, recreational activities, and choice of music. Listening to soothing music promotes cardiovascular health. One should laugh daily with friends or family to avoid stress because laughter is the best medicine. In brief, staying in the vicinity of nature, under clean and hygienic conditions, with a healthy friend circle and a cheerful disciplined lifestyle nourishes the heart and boosts the effective pumping of oxygenated blood to various parts of the body.
Diet: Dietary regimens that promote excellent health emphasize eating various fruits, vegetables, whole grains, lean protein sources, legumes, dairy products, nuts, and seeds while minimizing the consumption of processed meals and foods high in calories. Two dietary approaches can reduce the risk of developing cardiovascular disease, i.e., the DASH (Dietary Approaches to Stop Hypertension) diet and the Mediterranean diet. The DASH diet prioritizes eating whole grains, fruits, vegetables, low-fat dairy, lean meat, fish, poultry, nuts, seeds, and legumes while limiting the consumption of salt (sodium intake), fats, and oils. This diet is low in saturated/trans fats and contains antioxidants, minerals, fiber, and nitrates [40]. The Mediterranean diet emphasizes eating non-refined cereals, fresh fruits, vegetables, nuts, low-fat dairy products, moderate intake of alcohol (red wine), moderate consumption of fish, poultry, potatoes, and eggs, monthly consumption of red meat, and regular physical activity. Olive oil serves as the principal source of lipids in the Mediterranean diet. These functional foods positively impact our health and protect us against developing heart attacks [44].
Smoking: Quit smoking as early as possible to support and strengthen the efficient pumping of oxygenated blood from the heart to various body parts. A well-established risk factor for all forms of cardiovascular diseases is tobacco smoking. The likelihood of survival or death of a person suffering from a heart attack is often decided by this factor, whether the patient had been a chain smoker or not.
Stress: A heart attack is usually a turning point in one’s life, an episode after which one sees the world differently and begins appreciating life much more than ever before. According to WHO, stress can be defined as a state of worry or mental tension caused by a problematic situation. A few decades ago, the word Stress appeared only in physics and mechanical engineering, not in personal life. It was not a part of our English vocabulary. Now, we hear everyone, including school-going children, housewives, youngsters, businesspersons, executives, Govt servants, and elderly persons, talking about stress. Stress is routine and essential for growth in the modern competitive world. Nevertheless, once we label it as routine and indispensable, we accept it and do not attempt to remove it.
Stress is determined as the ratio of Pressure and Resilience (Inner strength). Thus, Stress = Pressure/ Resilience (Inner strength). Therefore, the more the pressure, the more stress and less output since stress is inversely proportional to Efficiency (Performance). In the modern world, the numerator (Pressure) has increased tremendously. For example, there is tremendous pressure from parents, friends, children, spouses, society, peers, teachers, bosses, clients, and employers to perform. Thus, there is immense pressure, so enormous stress, and consequently, the performance is low. We must focus on the denominator (Resilience (Inner strength)). That’s the only thing under our control. If we focus on and increase our inner strength, there will be no stress, and our performance (efficiency) will be very high. Daily walking and self-talk help in combating stress to a large extent. One should spend more time with persons; one is happy with and avoid the company of persons one is unhappy with. One should get involved in activities one likes to consolidate one's strengths. One should not bother about one's weaknesses and leave them alone. Sparing time for hobbies, participating in outdoor/indoor games, and following a cheerful disciplined lifestyle eliminates all life's stress, strengthens cardiovascular function, and boosts complete physical and mental health. A critical risk factor linked to a higher incidence of cardiovascular events is psycho-social stress, also known as mental stress. It triggers the emergence of hypertension, the rapid development of atherosclerotic conditions, increased insulin resistance, and associated obesity. It is essential to give psychological support to people with cardiovascular disorders [45]. Family stress, work stress, social isolation, absence of social support, and a lack of a purpose in life are all known risk factors for the development of CVD. Regular exercise, meditation, and physical activity serve as stress busters [46].
Alcohol Consumption: The incidence of cardiovascular disease and alcohol intake may or may not be related. Regarding alcohol's influence on cardiovascular disease, the quantity consumed appears to be of utmost significance. Overindulgence in alcohol has detrimental effects on health, raising the risk of developing hypertension and death from cardiovascular diseases [40]. However, red wine, which contains alcohol and polyphenols, lowers oxidative stress and guards against the onset of thromboembolic disease. Additionally, it has been demonstrated that consuming 25g of alcohol per week can reduce cardiovascular risk [47]. Too much alcohol consumption elevates triglyceride levels, which combine with LDL and is associated with the deposition of fatty plaques along the artery walls. As a result, the risk of heart failure and stroke increases. Alcohol has been linked to secondary non-ischemic dilated cardiomyopathy, hypertension, atrial/ ventricular arrhythmias, and reduction in myocardial contractility. Alcoholic cardiomyopathy, which causes dilatation and reduced contractility of the left or both ventricles, can appear after years of heavy alcohol consumption [48]. Alcohol may cause swelling and inflammation in the liver. Three stages of liver damage have been observed following heavy alcohol consumption. These stages include fatty liver, alcoholic hepatitis, and liver fibrosis/cirrhosis. Proper liver function is essential for normal heart functioning. Heart attacks occur when liver or kidney function is abnormal. A heart attack may be considered a blessing in disguise, a fantastic opportunity to start living life all over again following a healthy lifestyle.
Heart and Kidney: The efficient functioning of the heart and kidneys is crucial for a healthy person. Impairment of any of these vital organs results in simultaneous impairment of the other organ. Kidney damage leads to increased blood pressure, enhanced workload of the heart, and heart failure.
Alarming Signs of Heart
Chest pain.
Intense pain in the shoulder and feeling sick.
Back pain or jaw pain.
Choking sensationor tightness in throat or chest.
Burning sensation in the chest or stomach.
Feeling sweaty and hot, along with chest pain.
Cramps in lower limbs signal a peripheral arterial disease.
Swollen ankles
Extreme fatigue
Irregular heartbeat/palpitations of the heart.
Conclusion
A comprehensive strategy must be developed to prevent and manage heart disorders. A heart attack is usually a shocking episode, compelling the victim to modify his lifestyle considerably out of fear of death. There are many ways to reduce the risk of heart disease, although one cannot change some risk factors, such as family history, age, or gender. One of the best things one can do for a healthy heart is to stop active or passive smoking and limit drinking liquor. Chemicals in tobacco damage the heart, constrict blood vessels and reduce the oxygen in the blood. This leads to increased blood pressure and heart rate, thereby enhancing the burden on the heart to work harder to supply enough oxygen to different parts of the body and brain consequently. Interestingly, heart disease risk starts dropping as early as 24 hours after quitting cigarette smoking. The concept of helpful and harmful foods provides a valuable framework for understanding the complex interplay between nutrition and cardiovascular disorders. The risk factors such as serum cholesterol, hypertension, and obesity can be favorably controlled by consuming a heart-friendly diet comprising fruits, vegetables, proteins, and whole cereals. In addition to healthy dietary patterns, lifestyle modifications such as regular physical activity and stress management have been shown to benefit overall cardiovascular health. Physical activity helps to control body weight. It also reduces the chances of developing other conditions that may strain the heart, such as high blood pressure, high cholesterol, and Type- 2 diabetes. Even short bouts of physical activity offer many benefits to the heart. However, one should not exercise strenuously in any case. Being overweight, especially bulging around the tummy and hips, enhances the risk of hypertension, atherosclerosis, and Type-2 diabetes. It is essential to undergo regular check-ups for measuring pre-prandial and postprandial glucose levels, cholesterol levels, lipid profiles, and kidney and liver function. If one is suffering from diabetes, hypertension, or hyperlipidemia, one should consult a physician and take appropriate medicines regularly without fail. An individual, who does not get enough sleep, has a higher risk of developing hypertension, obesity, diabetes, depression, and, consequently, a heart attack. Most adults need at least seven hours of sleep each night. The authors recommend setting up an asleep-wake-up cycle and adhering to it as far as possible by going to bed and waking up at the same time every day. Stress is an essential factor contributing to heart attacks. To counter stress, one should not indulge in over-eating, over-drinking, and/or over-sleeping. The best way of managing stress comprises listening to soothing music, walking in a park, meditating, or spending jolly time with friends. A personalized approach that accounts for individual differences in genes, metabolism, presence of other diseases, and lifestyle is likely the most effective strategy for reducing the risk of developing heart attacks. A heart-friendly diet, regular physical activity, quitting alcohol, smoking cessation, and keeping blood pressure in the normal range are effective measures to prevent heart attacks. If one lives a happy, healthy, and peaceful life while staying young at heart, one need not fear any fatality.
Take Home Message
- Quit smoking and drinking as early as possible.
- Eat a low-salt diet.
- Reduce body weight.
- Exercise regularly.
- A Heart-friendly diet (low in saturated fats, reduced intake of carbohydrates, and sweetened beverages) can help reduce the risk of cardiovascular disease.
- Eat garlic daily.
- Focus on eating more fruits, vegetables, nuts, whole grains, berries, avocados, etc.
- 40 - 75 years old, individuals should periodically check their B.P. & ECG.
- It is essential to get regular check-ups done with your healthcare provider.
- Kidney and Liver functions be tested once a year by all senior citizens.
- HbA1c Test for optimum blood glucose levels is recommended.
- A lipid Profile Test measures good and bad cholesterol levels.
- Adhere to the medication provided by the physician.
References
- (2023) National Center for Health Statistics. Multiple Cause of Death 2018–2021 on CDC WONDER Database.
Publisher | Google Scholor - Tsao CW, Aday AW, Almarzooq ZI, Beaton AZ, Bittencourt MS, et al. (2023) Heart disease and Stroke Statistics—2023 Update: A Report from the American Heart Association. Circulation. 147: e93–e621.
Publisher | Google Scholor - Kundu J, Kundu S. (2022) cardiovascular disease (cardiovascular disorder) and Its Associated Risk Factors among Older Adults in India: Evidence from LASI Wave 1. Clin Epidemiol Glob Health. 13: 100937.
Publisher | Google Scholor - Zhao CN, Meng X, Li Y, Li S, Liu Q, et al. (2017) Fruits for Prevention and Treatment of Cardiovascular Diseases. Nutrients. 9(6); 598.
Publisher | Google Scholor - Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, et al. (2020) Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J Am Coll Cardiol. 76(25): 2982–3021.
Publisher | Google Scholor - Ho, M. Y., & Wang, C. Y. (2021). Role of irisin in myocardial infarction, heart failure, and cardiac hypertrophy. Cells, 10(8), 2103.
Publisher | Google Scholor - Tyrovola D, Soulaidopoulos S, Tsioufis C, Lazaros G. (2023) The Role of Nutrition in Cardiovascular Disease: Current Concepts and Trends. Nutrients. 15(5):1064.
Publisher | Google Scholor - Golovinskaia O, Wang CK. (2021) Review of Functional and Pharmacological Activities of Berries. Molecules. 26: 3904
Publisher | Google Scholor - Yang H, Tian T, Wu D, Guo D, Lu J. (2019) Prevention and treatment effects of edible berries for three deadly diseases: cardiovascular disease, cancer, and diabetes. Crit Rev Food Sci Nutr. 59(12): 1903-1912.
Publisher | Google Scholor - Casas R, Castro-Barquero S, Estruch R, Sacanella E. (2018) Nutrition and Cardiovascular Health. Int. J. Mol. Sci. 19: 3988.
Publisher | Google Scholor - Soliman G A. (2019) Dietary Fiber, Atherosclerosis, and cardiovascular disease. Nutrients, 11 (5): 1155
Publisher | Google Scholor - Wehrli F, Taneri PE, Bano A, Bally L, Blekkenhorst LC, et al. (2021) Oat Intake and Risk of Type 2 Diabetes, Cardiovascular Disease, and All-Cause Mortality: A Systematic Review and Meta-Analysis. Nutrients 13: 2560.
Publisher | Google Scholor - Baynham R, Veldhuijzen van Zanten JJCS, Johns PW Pham QS, Rendeiro C. (2021) Cocoa Flavanols Improve Vascular Responses to Acute Mental Stress in Young Healthy Adults. Nutrients 13 (4): 1103.
Publisher | Google Scholor - Lin X, Zhang I, Li A, Manson JE, Sesso HD, et al. (2016) Cocoa flavanol intake and biomarkers for cardiometabolic health: a systematic review and meta‐analysis of randomized controlled trials. J Nutr. 146: 2325–2333.
Publisher | Google Scholor - Cao S, Weaver CM. (2022) Bioactives in the Food Supply: Effects on cardiovascular disorder Health. CurrAtheroscler Rep. 24 (8): 655–661.
Publisher | Google Scholor - Yamagata K. (2018) Endothelial Protective Effects of Dietary Phytochemicals: Focus on Polyphenols and Carotenoids. Studies in Natural Products Chemistry. 55: 323–350.
Publisher | Google Scholor - Kura B, Parikh M, Slezak J, Pierce GN. (2019) The Influence of Diet on MicroRNAs That Impact Cardiovascular Disease. Molecules. 24(8): 1509.
Publisher | Google Scholor - Zhao CN, Meng X, Li Y, Li S, Liu Q, et al. (2017) Fruits for Prevention and Treatment of Cardiovascular Diseases. Nutrients. 9 (6): 598.
Publisher | Google Scholor - Costa-Rodrigues J, Pinho O, Monteiro PRR. (2018) Can lycopene be considered an effective protection against cardiovascular disease? Food Chem. 245: 1148–1153.
Publisher | Google Scholor - Summerhill V, Karagodin V, Grechko A, Myasoedova V, Orekhov A. (2018) Vasculoprotective Role of Olive Oil Compounds via Modulation of Oxidative Stress in Atherosclerosis. Front Cardiovasc Med. 5: 188.
Publisher | Google Scholor - Khedir SB. (2018) Effects of Minor Components of Olive Oil on Health. Journal of Complementary Medicine & Alternative Healthcare. 5 (2): 555658.
Publisher | Google Scholor - Guasch-Ferré M, Liu X, Malik VS. Sun Q, et al. (2017) Nut Consumption and Risk of Cardiovascular Disease. J Am Coll Cardiol. 70 (20): 2519–2532.
Publisher | Google Scholor - Xiao Y, Xia J, Ke Y, Cheng J, et al. (2018) Effects of Nut Consumption on Selected Inflammatory Markers: A Systematic Review and Meta-nalysis of Randomized Controlled Trials. Nutrition, 54: 129–143.
Publisher | Google Scholor - Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, et al. (2019) Marine N−3 Fatty Acids and Prevention of Cardiovascular Disease and Cancer. New England Journal of Medicine. 380 (1): 23–32.
Publisher | Google Scholor - Burke MF, Burke FM, Soffer DE. (2017) Review of cardiometabolic effects of prescription Omega-3 fatty acids. Curr. Atheroscler. Rep. 19(12): 60.
Publisher | Google Scholor - Golanski J, Szymanska P, Rozalski M. (2021) Effects of Omega-3 Polyunsaturated Fatty Acids and Their Metabolites on Haemostasis—Current Perspectives in Cardiovascular Disease. International Journal of Molecular Sciences. 22 (5): 2394.
Publisher | Google Scholor - Shahidi F, Ambigaipalan P. (2018) Omega-3 Polyunsaturated Fatty Acids and Their Health Benefits. Annu Rev Food Sci Technol. 9: 345-381.
Publisher | Google Scholor - Sun YE, Wang W, Qin J. (2018) Anti-hyperlipidemia of garlic by reducing the level of total cholesterol and low-density lipoprotein: A meta-analysis. Medicine (Baltimore). 97(18): 255.
Publisher | Google Scholor - Ansary J, Forbes-Hernández TY, Gil E, Cianciosi D, Zhang J. (2020) Elexpuru-Zabaleta M, Simal[1]Gandara J, Giampieri F, Battino M. Potential Health Benefit of Garlic Based on Human Intervention Studies: A Brief Overview. Antioxidants. 9 (7): 619.
Publisher | Google Scholor - Sethi N, Kaura S, Dilbaghi N, Parle M, Pal M. (2014) Garlic: A pungent wonder from nature. Int. Res. J. Pharm. 5(7): 523-529.
Publisher | Google Scholor - Isha D, Parle M. (2012) Eat til and protect dil. Int. Res. J. Pharm. 3(11): 54-57.
Publisher | Google Scholor - Laka K, Makgoo L, Mbita Z. (2022) Cholesterol-Lowering Phytochemicals: Targeting the Mevalonate Pathway for Anticancer Interventions. Front Genet. 13: 628.
Publisher | Google Scholor - DiNicolantonio JJ, Lucan SC, O’Keefe JH. (2016) The Evidence for Saturated Fat and for Sugar Related to Coronary Heart Disease. Prog Cardiovasc Dis. 58(5): 464–472.
Publisher | Google Scholor - Wang Z, Bergeron N, Levison BS, Li XS, Chiu S, et al. (2019) Impact of chronic dietary red meat, white meat, or non-meat protein on trimethylamine N-oxide metabolism and renal excretion in healthy men and women. Eur Heart J. 40(7):583-594.
Publisher | Google Scholor - On-Nom N, Khaengamkham K, Kettawan A, Rungruang T, Suttisansanee U, et al. (2023) Parboiled Germinated Brown Rice Improves Cardiac Structure and Gene Expression in Hypertensive Rats. Foods. 12: 9.
Publisher | Google Scholor - Gadiraju T, Patel Y, Gaziano J, Djoussé L. (2015) Fried Food Consumption and Cardiovascular Health: A Review of Current Evidence. Nutrients. 7(10): 8424–8430.
Publisher | Google Scholor - Szczepańska, E., Białek-Dratwa, A., Janota, B., & Kowalski, O. (2022). Dietary Therapy in Prevention of Cardiovascular Disease (CVD)—Tradition or Modernity? A Review of the Latest Approaches to Nutrition in CVD. Nutrients, 14(13), 2649.
Publisher | Google Scholor - Cosmi F, Di Giulio P, Masson S. (2015) Regular wine consumption in chronic heart failure: Impact on outcomes, quality of life, and circulating biomarkers. Circulation: Heart Failure. 8(3): 428–437.
Publisher | Google Scholor - Pan A, Lin X, Hemler E, Hu FB. (2018) Diet and Cardiovascular Disease: Advances and Challenges in Population-Based Studies. Cell Metab. 27(3): 489–496.
Publisher | Google Scholor - Wickman, B. E., Enkhmaa, B., Ridberg, R., Romero, et al. (2021). Dietary management of heart failure: DASH diet and precision nutrition perspectives. Nutrients, 13(12), 4424.
Publisher | Google Scholor - Perez-Terzic, C. M. (2012). Exercise in cardiovascular diseases. PM&R, 4(11), 867-873.
Publisher | Google Scholor - Ciumărnean, L., Milaciu, M. V., Negrean, V., Orășan, O. H., et al. (2022). Cardiovascular risk factors and physical activity for the prevention of cardiovascular diseases in the elderly. International Journal of Environmental Research and Public Health, 19(1), 207.
Publisher | Google Scholor - Bhatnagar A. (2017) Environmental Determinants of Cardiovascular Disease. Circ Res. 121(2):162-180. doi 10.1161/CIRCRESAHA.117.306458. PMID: 28684622; PMCID: PMC5777598.
Publisher | Google Scholor - Finicelli, M., Di Salle, A., Galderisi, U., & Peluso, G. (2022). The Mediterranean Diet: An Update of the Clinical Trials. Nutrients, 14(14), 2956.
Publisher | Google Scholor - Sara, J. D. S., Toya, T., Ahmad, A., Clark, M. M., Gilliam, W. P., et al. (2022). Mental stress and its effects on vascular health. In Mayo Clinic Proceedings (Vol. 97, No. 5, pp. 951-990). Elsevier.
Publisher | Google Scholor - Popovic, D., Bjelobrk, M., Tesic, M., Seman, S., Jayasinghe, S., et al. (2022). Defining the importance of stress reduction in managing cardiovascular disease-the role of exercise. Progress in cardiovascular diseases, 70, 84-93.
Publisher | Google Scholor - Zhang, X., Liu, Y., Li, S., Lichtenstein, et al. (2021). Alcohol consumption and risk of cardiovascular disease, cancer, and mortality: a prospective cohort study. Nutrition Journal, 20, 1-10
Publisher | Google Scholor - Gallucci G, Tartarone A, Lerose R, Lalinga AV, Capobianco AM. (2020) Cardiovascular risk of smoking and benefits of smoking cessation. J Thorac Dis. 12(7): 3866–3876.
Publisher | Google Scholor