Research Article
Conservative Versus Early Surgical Interventions in Treatment of Spondylodiscitis
1Neurosurgeon Specialist, Rizgary Teaching Hospital, Erbil Directorate of Health, Erbil, Kurdistan Region, Iraq.
2Psychiatrist and Mental Health Specialist, Hospital of Treatment Victims of Chemical Weapons, Halabja Directorate of Health, Halabja, Kurdistan Region, Iraq.
*Corresponding Author: Makwan Mohammed Abdulkareem, Psychiatrist and Mental Health Specialist, Hospital of Treatment Victims of Chemical Weapons, Halabja Directorate of Health, Halabja, Kurdistan Region, Iraq.
Citation: Najm M.N., Abdulkareem M.M. (2025). Conservative Versus Early Surgical Interventions in Treatment of Spondylodiscitis, International Journal of Biomedical and Clinical Research, BioRes Scientia Publishers. 3(1):1-16. DOI: 10.59657/2997-6103.brs.25.038
Copyright: © 2025 Makwan Mohammed Abdulkareem, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 22, 2024 | Accepted: December 27, 2024 | Published: January 03, 2025
Abstract
Introduction: Spondylodiscitis is infection of the nucleus pulpous with secondary involvement of cartilaginous endplates then finally vertebral body, and increasingly in incidence post-operatively.
Objective: Assessment of most appropriate treatment for Lumber Post-operative discitis.
Methods: A prospective study conducted in AL-Shaheed Ghazzi AL-Harriri hospital of Baghdad Medical city and Erbil teaching hospitals (Rozhawa and Rozhalat trauma emergency hospital) from October 2019 to March 2021. 32 cases of Post-Operative Discitis were taken who were diagnosed clinically, radiologically, and laboratory investigations. Patients were divided into two groups, the first group which was managed conservatively for post-operative discitis were labeled (conservative) versus the second group who were managed surgically, labeled (surgical).
Results: Comparing to the conservative group, the surgical group had significantly less hospital stay, less duration of bed rest, antibiotic therapy, and discitis symptoms were reduced more with less complication rates. The functional outcome of patients who received operative treatment at the end of 3rd month follow-up was better than the conservative treatment group.
Conclusions: Most patients at early stage of post-operative discitis can be managed conservatively by immobilization and analgesics along with culture guided systemic antibiotic. However, surgery is recommended when complications arise like neurological impairment, severe pain or kyphosis, abscess, spinal instability or failure of conservative management.
Keywords: post-operative discitis; MIS; PLIF
Introduction
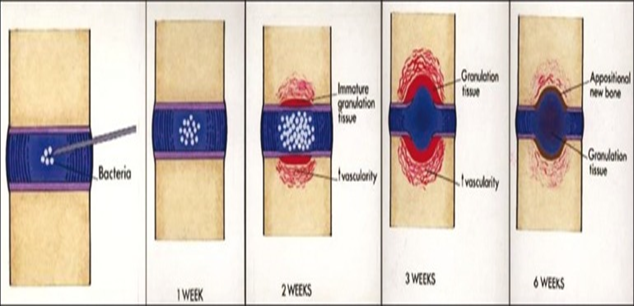
Discitis (disc space infection) is infection of intervertebral disc space or to some degree of the vertebral endplate. Frank Turnbull was the first who described postoperative discitis in 1953. So, it is primarily an infection of the nucleus pulpous with secondarily an involvement of cartilaginous endplates then finally vertebral body. It can also occur following lumbar discectomies. So, this complication may follow open procedures as laminectomy and discectomy, or can follow a minimally invasive spinal procedure as myelography, paravertebral injection and lumbar puncture. It is vital to mention that post-operative discitis can be aseptic or septic, even though that recent data suggest that it is mainly due to bacterial infections (septic) [1-3]. Below illustrated figure shows the chronological progress and evolvement of Post-Operative Discitis.
Figure 1: Pathogenesis of postoperative discitis, (from left to right) [3].
Incidence
Post-operative discitis incidence varies actually varies largely among countries, advancement of neurosurgical interventions, facilities and many other factors. Although there are no clear numbers or accurate neurosurgical follow up nor statistics documentation in our locality but in general the Middle east countries incidence rate of Post-operative Discitis is around 0.2% to 4% [4].
Risk Factors
Risk factors are divided into patient-specific factors, procedure-related factors, and perioperative care. Immunocompromised individuals are at a very high increased risk. Obesity and smoking may also be major contributing factors. Malnutrition, whether prior to the operation or post-operatively is also a major contributing cause to Post-Operative Discitis [5]. Regarding malnutrition, several markers have been stated as serum albumin level lessthan 3.5g/dl, recent weight loss greaterthan 4.5kg, arm muscle circumference lessthan 80% of normal, and lymphocyte count being lessthan 1500/mm [6]. Poorly controlled diabetes mellitus has been documented to have about 17% of postoperative complication rate, two thirds are surgical site infection and including Post-Operative Discitis, the reason behind that is due to macrophages dysfunction, opsonization dysfunction, or immunoglobulins malfunction, resulting in endothelial injury and premature atherosclerosis [7]. Also, worthy to be mentioned that the comorbidities associated with diabetes, such as cardiovascular disease, hypertension, and renal failure will further elevate the infection rate by compromising micro-vascularization and soft tissue status and viability [6]. Rheumatoid arthritis, corticosteroids use, adrenocortical insufficiency, radiation, and co-existing tumors have been described as risk factors, even though hard evidences are lacking [8].
Advances in surgical and instrumentation techniques enhanced and improved outcomes of many spinal diseases. However, many procedural related factors had added to sequelae of Post-Operative Discitis, including pseudo-arthrosis, loss of fixation, implant inducing peri-discal erosion, and spondylodiscitis [6,9]. So, for example the Staged procedures for complex spinal diseases have been associated with a 3-fold increased risk of Post-Operative Discitis due to increased surgical exposure, blood loss, nutritional depletion and length of hospital stay [10]. Also, the long-level instrumented fusions and long segment fixations or multiple level discectomies had contributed to more Post-Operative Discitis, while Lumbar surgeries in close proximity to sacrum/pelvis which are already possible sources of wound contamination and major risk for Post-Operative Discitis. Neuromuscular scoliosis whether congenital, idiopathic or a Disc prolapse temporarily related was also mentioned as an increased risk of Post-Operative Discitis secondary to paralysis, fecal or urinary incontinence, and subsequent implantation of pathogenic bacteria [11].
Table 1: Major risk factors for Post-Operative Discitis [12].
| Risk Factor Type | Patient-Specific | Surgery-Related |
| Pre-Operative | Advanced Age, Rheumatoid Arthritis, Corticosteroid Therapy, Diabetes Mellitus, Tobacco/Alcohol Use, Obesity, Malnutrition, Immunosuppression Cancer/Chemotherapy, Concomitant Infection (Skin, Visceral Organs) | Recent Hospitalization, Prior Surgery, Trauma, Tumor/Malignancy |
| Intra-Operative | Asa Score, Treatment Timing, Nutritional Status, Severe Trauma, Cardiovascular Disease, Hepatorenal Diseases | Length Of Surgery >5h, Posterior Approach, Number of Levels Operated, Instrumentation Implant Material, (Titanium Vs Stainless Steel), Use of Allograft, Blood Transfusion, Microscope, C-Arm, Open (As Opposed to Minimally Invasive Surgery), Staged Surgery |
| Post-Operative | Urinary/Fecal Incontinence, Catheters, Poor Wound Care, Extended Hospitalization, ICU Stay | CSF Leak |
Clinical Feature of Postoperative Discitis
The most common and most describable patient symptom for discitis is backache that is worse at night and gradually increasing to severe to excruciating pain at or near the surgical site following the relief of the initial postsurgical pain. Such pain might radiate to gluteal, thighs, legs, scrotum, groin or even perineal area. Fever and fatigue were described in 11%-68% of cases. Postoperatively, back pain usually develops (1-6 weeks) and most commonly at 3rd week following the surgery. Regarding the examination positive findings of Post-Operative Discitis, the neurological deficits are uncommon but not rare, while local spinal tenderness is most common finding associated with severely restricted movement range, pseudo-Gower sign (that is difficulty rising from bed), severe paravertebral muscle spasm, and sometimes loss of lumbar lordosis. Therefore, it is vital to have high index of suspicion for patients presenting with backache after spinal surgery to receive early diagnosis and treatment of post-operative discitis; otherwise, morbidity increases [1,3,13,14].
Bacteriology
Staphylococcus aureus is most frequently isolated microorganism but nevertheless there are other causes for Post-Operative Discitis like methicillin-resistant Staphylococcus aureus (MRSA) and gram-negative bacilli as Pseudomonas aeruginosa, E. coli, Acinetobacter, and Enterobacter species. While the Delayed Post-Operative Discitis may be caused by low-virulent organisms, like coagulase-negative Staphylococcus epidermidis, Propionibacterium acnes, Bacillus. Other ways of bacterial seeding like Hematological seeding of spinal instrumentation are rare but regarded as a major complication associated with bacteremia or sepsis for example Staph. aureus and Pseudomonas aeruginosa infections may be seen in intravenous drug abusers. Meanwhile is the isolated microorganism was shown to be E. coli or Enterococcus species then the genitourinary infections should rise the high index of suspicion as the route of transmission, for instance the Patients with history of bowel or bladder incontinence have a higher propensity for Post-Operative Discitis that are been caused by gram-negative aerobic bacilli [4,15]. The major dilemma is the emerging of the New Cephalosporin-resistant strains of staphylococcus that decreased efficacy of intravenous antibiotic prophylaxis by 60% [6].
Table 2: Suspected microorganisms in Post-Operative Discitis based on the Time of presentation [12].
| Etiological Cause | Microorganisms |
| Postoperative <1mo> | Coagulase Negative Methicillin-Resistant Staphylococcus. |
| Coagulase-Negative Methicillin Sensitive Staphylococcus. | |
| Methicillin-Resistant Staphylococcus Aureus. | |
| Methicillin Sensitive Staphylococcus Aureus. | |
| Streptococci. | |
| Gram-Negative Like Pseudomonas Aeruginosa. | |
| Postoperative >1mo | Gram-Negative Rods as Pseudomonas Aeruginosa, Escherichia Coli, Acinetobacter, and Enterobacter. |
| Coagulase-Negative Methicillin-Resistant Staphylococcus. | |
| Coagulase-Negative Methicillin Sensitive Staphylococcus. | |
| Methicillin-Resistant Staphylococcus Aureus. | |
| Methicillin Sensitive Staphylococcus Aureus. | |
| Streptococci. | |
| Postoperative>3mo | Propionibacterium Acnes, Bacillus, or Micrococcus. |
| Coagulase-Negative Methicillin-Resistant Staphylococcus. | |
| Coagulase-Negative Methicillin Sensitive Staphylococcus. |
Diagnosis of Postoperative Spondylodiscitis
Laboratory and Microbiological Tests
Initial blood tests include leukocyte count (WBC) and C-reactive protein (CRP). Although Erythrocyte sedimentation rate (ESR) is often mentioned but it is non-specific [16]. so rather than for diagnosis but to identify the response to antibiotic management can be monitored effectively using CRP and ESR [17]. Peak ESR levels are detected up to 5-7 days after surgery that usually normalize within 4-6 weeks. Typically, CRP values peak at 3 days and rapidly decline within 10-14 days. So, performing repeated readings of ESR/CRP levels may indicate improvement or clinical progression of Discitis so rise of CRP after 10-14 days or failure to normalize is a sensitive indicator of discitis or surgical site infection as a whole, while a negative test result or a normalizing CRP is reassuring that the Post-Operative Discitis is unlikely. Leukocytosis is not necessarily present (30-50% present), while raised CRP is seen in 90%-98% of cases. Jean et al. showed that a raised CRP can shorten the time for diagnosis compared to other laboratory parameters [18].
Procalcitonin (PCT) level plays a small role as an indicator of sepsis in the primary diagnosis of spondylodiscitis, and is more costly and less sensitive than CRP [19]. Regarding to Blood Cultures in Post-Operative Discitis, minimum two blood culture pairs (aerobic/anaerobic) are harvested. The underlying pathogen can be identified in about 40-50% of blood cultures [20], whereas pathogen detection rate can increase to up to 70% if the patient was not on antibiotics [21]. Histopathological Material Sampling can be further obtained by computed tomography-guided fine-needle biopsy or by open surgery. Pathogen detection is 25 percentage accurate when using CT-guided fine-needle biopsy, whereas detection can be achieved in 40% using open surgical histopathological techniques [22]. More recent study showed that microorganism detection can be improved using both magnetic resonance imaging (MRI) and CT involving superimposition of the two combined images data from both CT/MRI prior to fine-needle biopsy obtaining procedure [23]. According to Kim et al., the microorganism detection was 2.28 folds higher following soft tissue biopsy compared to osseous tissue [4,24].
Diagnostic Imaging
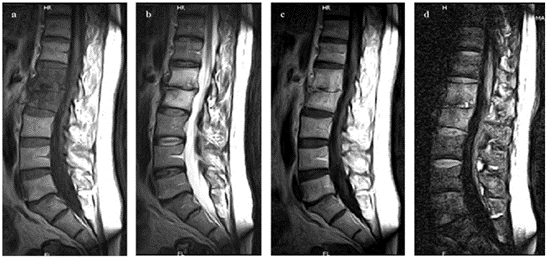
Conventional X-ray imaging is first line of imaging work-up in patients with spinal complains; and generally, both sensitivity and specificity are low [26]. So, the earliest features are Erosion of base and upper plates or increasingly destructive kyphosis can be detected after days or weeks and so the time of presentation and radiological findings are highly dependent on the virulence of the microorganism, the patient’s immune status, or clinical course of disease, therefore, a negative conventional X-ray film does not exclude spondylodiscitis, it is needed to evaluate disease progression as the spondylodiscitis evolves [27]. The second commonly used radiological work-up is the computed tomography (CT) and can be sometimes used as an alternative if there were any contraindications to MRI. Another advantage of CT is that Paravertebral abscesses can be better visualized with contrast-enhanced CT [28]. While the MRI is the gold standard imaging study to detect spondylodiscitis, moreover adding contrast agent will facilitates the differentiation between the features of spondylodiscitis, degenerative medic changes, or neoplasia [29]. Specificity and sensitivity are very high and can reach up to 96% and 92%, respectively [27]. While adding the Gadolinium contrast -enhanced MRI has raised the sensitivity as high as 95.4% [27].
STIR, Short-Tau Inversion Recovery
Table 3: Radiological findings on MRI [4].
| MRI Weighting | Radiological Changes |
| T2/STIR | Hyper-intense intervertebral disc, Hyper-intense adjacent vertebral bodies |
| T1 | Hypo-intense intervertebral disc, Hypo-intense adjacent vertebral bodies |
| Regardless of Weighting | Loss of disc height, End plate erosion |
| Signs of paravertebral/epidural inflammation |
STIR-Short-Tau Inversion Recovery.
While some studies advocated the use of the Fluorine-18 fluorodeoxyglucose positron emission tomography/CT (18F-FDG-PET-CT) in diagnosis of spondylodiscitis [30]. PET-CT represents a good alternative in the case of contraindications to contrast-enhanced MRI/CT but it's very expensive and only available in specialized centers [4]. Recent studies have shown another advantage of PET-CT is in the differentiation between degenerative Modic type I changes and inflammatory changes [31] but the other disadvantage aside from its cost, is that the PET-CT is not specific to differentiate neoplasia, spondylodiscitis, and post-traumatic bone marrow edema and hence this PET-CT does have a high sensitivity but low specificity as compared to the MRI [32].
Figure 2: MRI sequences in Spondylodiscitis [12].
Figure 3: MRI and PET-CT and their follow-up in Spondylodiscitis [12].
(MRI and PET/CT imaging in a 38 years old patient with back pain, fever and S. Epidermidis infection of the lumbar spine confirmed by positive microbiology culture of the vertebral biopsy. (A): baseline lumbar MRI, sagittal image showed oedema in the intervertebral disc between L1 and L2, confirmed by fused PET/CT scans (B). After three mounts of therapy, both scans (C, D) showed spondylodiscitis in resolution)
Prevention
The choice of the antibiotics should be a one with cidal (not static) activity against most common infecting bacteria and also must be with adequate tissue availability throughout spinal procedures. First-generation cephalosporins have activity against gram-positive staphylococci and gram-negative bacteria that were one of the most causes of surgical site infections. So as an example of the 1st generation cephalosporin Cefazolin have a long half-life in both serum and bone. Regarding the aminoglycosides, toxicity and poor penetration properties of gentamycin into osseous tissues render the gentamicin as a non-optimal choice for spinal surgical prophylaxis [1]. Newer studies showed that the Intravenous vancomycin prophylactic administration had failed to decrease Post-Operative Discitis as compared with the cephalosporins [12]. Other Intraoperative measures has been included and used, including aseptic field, appropriate hemostasis, restricting traffic of operating room and also closed drainage had led to less and more controlled percentage of Operative Surgical site infections in general and Discitis in specific. Intermittent release of retractors and excessive irrigation of saline or even irrigation of the surgical site with antibiotics reduce local muscle ischemia [10]. Another mode of bone cement application in spinal surgeries is the usage of the Gentamicin, tobramycin, or vancomycin powder mixed with polymethylmethacrylate cement to produce a matrix that allows for persistent penetration and stability of antibiotics [2]. A retrospective study had showed that placement of collagenous sponges containing gentamicin in the disc space were to some degree an effective way in preventing postoperative spondylodiscitis [13]. The new studies had showed that the single and the most effective measure to be taken to decrease the Post-Operative Discitis is the accurate administration of preventive antibiotics throughout the procedure with decreasing both of the blood loss (optimally should be less than1500mL) and decreasing the operative times (optimally less than 4h) [1].
Treatment of Postoperative Discitis
Conservative Treatment for Postoperative Lumbar Spondylodiscitis Without Internal Fixation
The first step in managing spondylodiscitis as the conservative treatment will include antibiotic therapy, immobilization, bed rest and spinal bracing. Once spondylodiscitis is diagnosed, patients are managed by exclusive intravenous administration empirical broad-spectrum antibiotic and immobilization [4].
Surgical Treatment for Postoperative Lumbar Spondylodiscitis Without Internal Fixation
The logical way is that the operative management for postoperative spondylodiscitis without internal fixation is recommended when conservative treatment has failed. One of the techniques is Posterior debridement and fusion with or without instrumentation is widely undertaken for infectious spondylodiscitis because of that most neurosurgeons are familiar with this operative approach and instrumentation techniques [13,24]. Other studies of surgically managing the Postoperative spondylodiscitis using closed-suction irrigation system following surgical debridement, followed by intravenous systemic antibiotics for 3-4 weeks, and further oral antibiotics for 2-3 months [25,28,32]. The aim of this study is to assess the most appropriate treatments options for Lumber Post-operative discitis.
Methodology
This prospective study was carried out in Neurosurgical and Trauma department of Baghdad Medical city (Al-Shaheed Ghazi AL-Hariri hospital) and Erbil teaching hospitals (including Rozhawa and Rozhalat trauma emergency hospital) from October 2019 to March 2021.Inclusion criteria were patients with diagnosed Post-Operative Discitis within 1-6 weeks following single-level lumbar discectomy. Exclusion criteria were patients with spontaneous discitis, patients with multiple-level discectomy, patients with gross spinal instability and patients who lost or missed the scheduled followed up during the first 2 months following surgery, or lost tracks of follow up during the scheduled study research. So total of 32 cases of confirmed diagnosed Post-Operative Discitis were taken as samples and Records of 13 men and 3 women aged 29-58 years who underwent conservative treatment for Post-Operative Lumbar Discitis Group (conservative) after single-level open discectomy at L3-L4 (n=1), L4–L5 (n=12), and L5-S1 (n=3) and 13 men and 3 women aged 26-58 years who underwent operative treatment for diagnosed Post-Operative Discitis Group (surgical) following single-level open discectomy at L3-L4 (n=3), L4-L5 (n=11), and L5-S1 (n=2) were reviewed. Most of the primary discectomies patients had history of two antibiotics (intravenous ceftriaxone 1 gm in 100 cc normal saline infusion plus gentamicin ampule 80mg direct intravenously) given within1 hour before induction, followed by another 5 days of intravenous antibiotics (intravenous ceftriaxone 1 gm twice daily in 100 cc normal saline infusion plus gentamicin ampule 80mg three times daily) and then were discharged on oral antibiotics (oral 3rd generation cephalosporin of cefixime 400mg once daily) and dressing every other day with sterile gauze, povidone iodine 10% and surgical plaster. Above patients were diagnosed clinically, radiologically, and by laboratory parameters as follows:
All patients within 1-6 weeks of presentation encountered constant lumbar pain that was worse at night and gradually increasing to severe or excruciating pain. Such pain was described as continuous and deep along with morning stiffness. The patients also described an accompanying severe excruciating paravertebral muscle spasm radiating to the buttocks, groin, inguinal, leg and even abdomen. The pain was easily exacerbated by any simple motion. While regarding the examination, the patients showed a severe restriction of movements, positive pseudo-Gower sign (difficulty in getting up from supine of sitting position and the relying of upper limbs in getting up), and straight leg raising (SLR) test (a radiculopathy leg pain exacerbated by flexing the hip to up to 60 degrees while keeping the knee extended), as well as monitoring the dynamic lumbar pain (the pain elicited on flexion and extension of lumbosacral spine area). Blood parameters as CBC, ESR, CRP with titer, blood culture, blood sugar, serum albumin, liver and renal function tests were done to these patients with post –operative discitis and were done upon admission and were repeated on 1st week, 2nd week, 1st month, 3rd month and monitored as a response indicator to the specific method of treatment. Radiological imaging as X-rays and lumbosacral dynamic anteroposterior and lateral spine views were done to identify any endplate erosion, cavitation, reduction in disc space, and instability, with the addition of computed tomography (CT) were added if any sign of severe instability or vertebral collapse was to be suspected and the x-ray failed to provide a definitive vertebral body complication, while MRI with gadolinium contrast enhancement was the golden standard method in diagnosing and even sometimes evaluation of response to treatment or detecting any serious cauda equine syndrome complication like epidural abscess or vertebral collapse. In a very few cases a CT-guided aspiration of disc space was performed to identify the causative bacteria.
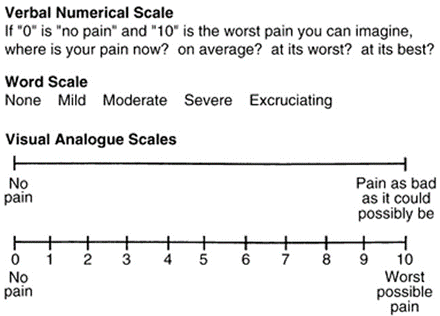
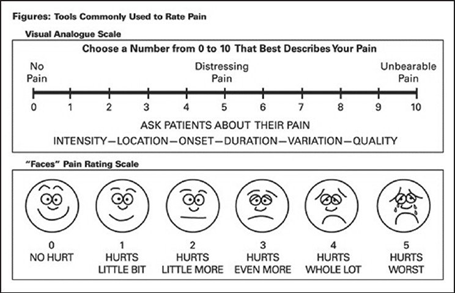
Patients with almost good general health status were classified into two groups, the first group which was managed conservatively for post-operative discitis were labelled (group conservative) versus the second group who were managed surgically for spondylodiscitis and labelled (group surgical). In addition, patients conservative group composed of 16 cases who received conservative treatment for a minimal 4-6 weeks of intravenous antibiotics, followed by minimal 4-6 weeks of oral antibiotics or until backache, ESR, and CRP levels were significantly declined, with full bed rest, dietary nutrition, analgesic agents, lumbar orthosis and physiotherapy. Whereas the surgical group involved 16 cases who received operative management in the form of a combination of discal debridement with posterior lumbar interbody fusion (PLIF), autogenous bone graft intra-discal implantation within the posterior lumbar interbody fusion (PLIF) and stabilization of the affected level by pedicle-screw fixation and rod. After this surgical operation, patients were treated by intravenous antibiotics for 2-3 weeks followed by oral antibiotics for another 3 weeks or until backache, ESR and CRP parameters significantly declined. Immediately after hematological investigations, blood culture, CT and MRI, all patients started empirical intravenous antibiotic therapy (ceftriaxone or meropenem with flucloxacillin or vancomycin, and metronidazole. Later on, the antibiotics were guided according to culture and sensitivity results. Surgical approach for each surgery is dependent on surgeons’ preferences, by which most neurosurgeons included in the study had chosen the fusion approach with posterior elemental fixation and so this type of surgeries was done due to the most familiarity, training and surgical experience according to case situation and the level of the infected lumbar spine. Demographic data, clinical variables, hospital length of stay, duration of antibiotic treatment, tissue culture reports and post-treatment complications were recorded. Preoperative and postoperative pain assessments were performed using Visual Analog scale (VAS).
Figure 4: Visual analog scale (VAS) for lumbar pain assessment.
Figure 5: Visual analogue scale (VAS) and related facial pain expressions.
Statistical analyses conducted using standard statistical software IBM SPSS; version 25. Descriptive statistical results were shown in the form of means and standard deviation for quantitative data and as frequency (%) for categorical data. P-values equal or less than 0.05 were considered as statistically significant. T-test was used to compare qualitative data, and Fisher exact test was used to compare categorical data.
Results
This prospective study was carried out in Neurosurgical and Trauma department of Baghdad Medical city (AL-Shaheed Ghazi AL-Hariri hospital) and Erbil teaching hospitals (including Rozhawa and Rozhalat trauma emergency hospital) from October 2019 to March 2021. The study included a total of 32 cases of confirmed diagnosed Post-Operative Discitis, in which 16 cases were included first group that were managed by conservative treatment and hence labelled group (conservative) versus 16 cases who were managed surgically and hence labelled group (surgical).
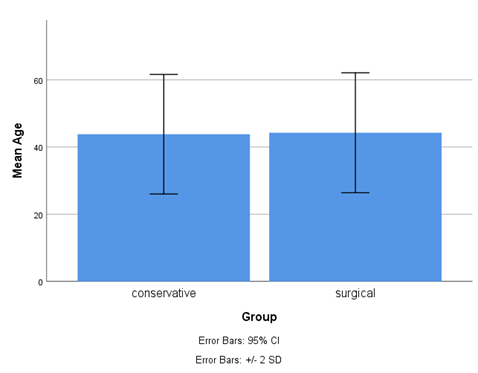
Age
In group (conservative) records of 16 cases age ranged (29-58) years who underwent conservative treatment for Post-Operative Lumbar Discitis, while in group (surgical) records of 16 cases age ranged between (26-58) years who underwent operative treatment for diagnosed Post-Operative Discitis (Group surgical) were reviewed.
Table 4: Mean, number, and standard deviation Age distribution of the patients.
| Group | Mean | N | Std. Deviation |
| Conservative | 43.81 | 16 | 8.894 |
| Surgical | 44.25 | 16 | 8.926 |
| Total | 44.03 | 32 | 8.768 |
Figure 6: Mean age distribution of the patients.
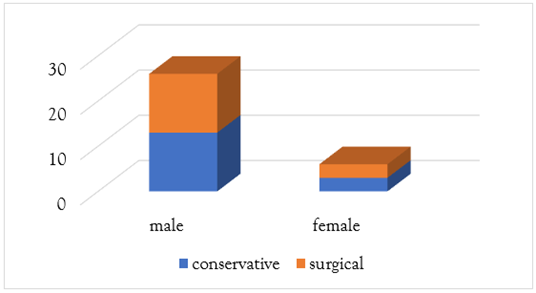
Gender
In group (conservative) records of 13 men and 3 women who underwent conservative treatment for Postoperative lumbar Discitis, while in group (surgical) 13 men and 3 women who underwent operative treatment for diagnosed Postoperative Discitis (Group surgical) were studied.
Table 5: Gender of the patients.
| Gender | Total | |||
| Male | Female | |||
| Group | Conservative | 13 | 3 | 16 |
| Surgical | 13 | 3 | 16 | |
| Total | 26 | 6 | 32 | |
Figure 7: Gender of the patients.
Risk Factors
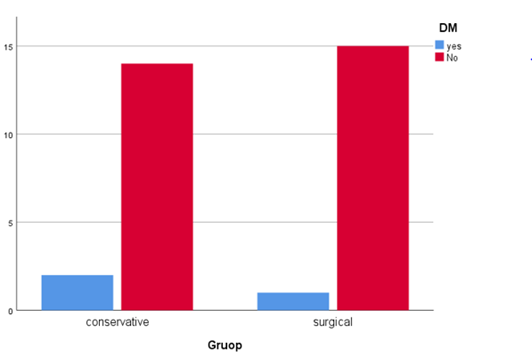
Diabetes Mellitus
One of the most crucial risk factors of surgical site infections as whole and Postoperative discitis as a part is the Diabetes because of the high comorbidities and mortality that is associated with it.
Table 6: Diabetes mellitus and its prevalence among study groups.
| Yes | No | Total | P value (Fisher Exact Test) | ||
| Group | Conservative | 2 | 14 | 16 | 0.5 |
| Surgical | 1 | 15 | 16 | ||
| Total | 3 | 29 | 32 | Not Significant | |
Figure 8: Number of Diabetes mellitus cases among the studied groups.
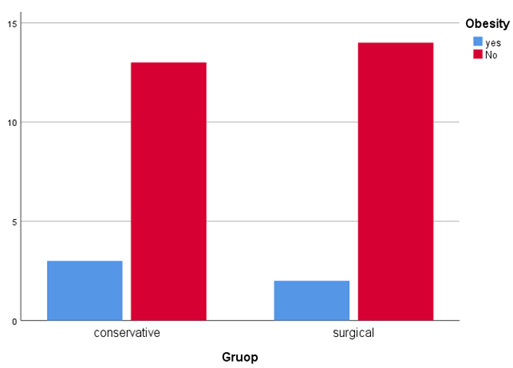
Obesity
Table 7: Number of obese patients and p value between the studied group.
| Obesity | Total | P Value (Fisher Exact Test) | |||
| Yes | No | ||||
| Group | Conservative | 3 | 13 | 16 | 0.5 |
| Surgical | 2 | 14 | 16 | ||
| Total | 5 | 27 | 32 | Not Significant | |
Figure 9: Prevalence of obese patients among the studied groups.
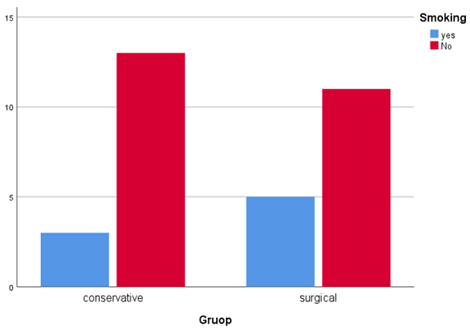
Smoking
Table 8: Number of smokers and p value between the studied group.
| Smoking | Total | P Value (Fisher Exact Test) | |||
| Yes | No | ||||
| Group | Conservative | 3 | 13 | 16 | 0.343 |
| Surgical | 5 | 11 | 16 | ||
| Total | 8 | 24 | 32 | Not Significant | |
Figure 10: Prevalence of smoker patients among the studied groups.
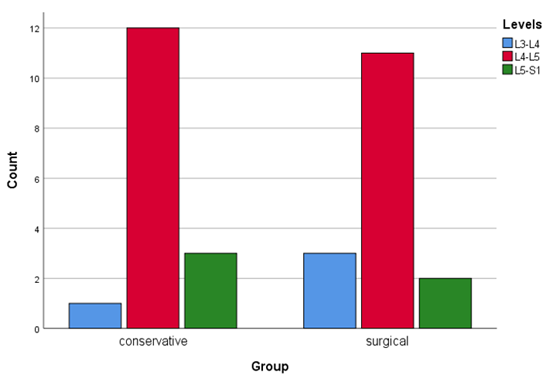
Levels
Among the 32 cases of confirmed diagnosed of Postoperative Discitis, after applying the inclusion criteria, the 16 cases of Group (conservative) distributed as L3-L4 (n=1), L4-L5 (n=12), and L5-S1 (n=3) and among the 16 cases of Group (surgical) distributed as at L3-L4 (n=3), L4-L5 (n=11), and L5-S1 (n=2) were reviewed.
Table 9: level of discitis and p value between the studied group.
| Levels | Total | P Value (Fisher Exact Test) | ||||
| L3-L4 | L4-L5 | L5-S1 | ||||
| Group | Conservative | 1 | 12 | 3 | 16 | 0.524 |
| Surgical | 3 | 11 | 2 | 16 | ||
| Total | 4 | 23 | 5 | 32 | Not Significant | |
Figure 11: Prevalence of the level of discitis in the studied groups.
Clinical Presentation
The clinical features of constant exacerbating back pain, leg pain, and morning stiffness in the form of paravertebral morning muscle spasm were documented in this study as well as examination points of percussion pain (a pain that is elicited or exacerbated with gentle percussing over the involved infected spinal segments that even may trigger sometimes a radicular pain), dynamic pain (in which a pain elicited in the lumbar spine upon active flexion and extension of the Lumbar area) as well as Straight leg raising test of less than 60 degrees. According to table (11), there is no significant difference between the conservative and surgical group regarding the clinical presentation.
Table 10: Clinical presentations of patients with conservative and surgical groups.
| Characteristics | Conservative Group (n=16) | Surgical Group (n=16) | P Values (Fisher Exact Test) |
| Constant Back Pain | 16(100%) | 16(100%) | 1.000ns |
| Leg Pain | 12(75%) | 15(93%) | 0.166ns |
| Morning Stiffness | 13(81%) | 15(93%) | 0.3ns |
| Percussion Back Pain | 12(75%) | 14(87%) | 0.327ns |
| Dynamic Pain | 11(68%) | 13(81%) | 0.343ns |
| SLRT | 7(43%) | 11(68%) | 0.143ns |
Blood Parameters
Blood laboratory parameters such as erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) with titer, were done to these patients with postoperative discitis and were done upon admission and were repeated on 1st week, 2nd week, 1st month, 3rd month and monitored as a response indicator to the specific method of treatment. According to Table (12), There is no statistically significant difference between the surgical and conservative group in the mean ESR and CRP before treatment, while there is statistically significant difference in the mean ESR and CRP after 1st week, 2nd week, 1st month, and 3rd month between the studied group.
Table 11: Blood parameters of patients with conservative and surgical groups.
| Blood Parameters | Measurement Time | Conservative Group Mean± STD | Surgical Group Mean± STD | P Value (t Test) |
| ESR | Pretreatment | 65.06±10.6 | 64.94±11.7 | 3.95ns |
| 1st Week Posttreatment | 61.94±5 | 50.31±8 | 0.00s | |
| 2nd Week Posttreatment | 53.69±5.1 | 36.63±4.7 | 0.00 s | |
| 1st Month Posttreatment | 42.94±4 | 26±3.1 | 0.00 s | |
| 3rd Month Posttreatment | 25.81±2.31 | 19.88±3.05 | 0.00 s | |
| CRP | Pretreatment | 69.44±10.5 | 68.81±12.4 | 0.88 ns |
| 1st Week Posttreatment | 65.88±4.6 | 46±6.4 | 0.00 s | |
| 2nd Week Posttreatment | 58.06±3.37 | 33.06±3.5 | 0.00 s | |
| 1st Month Posttreatment | 44±3.7 | 22.6±2.7 | 0.00 s | |
| 3rd Month Posttreatment | 24.25±2.3 | 13.31±1.92 | 0.00 s |
ns-not significant, s-significant.
Clinical and Functional Outcome Assessment by Visual Analogue Scale (VAS)
Table 12: Clinical and functional outcome assessment by VAS.
| VAS | Measurement Time | Conservative Group Mean± STD | Surgical Group Mean± STD | P Value (t Test) |
| Back pain | Pretreatment | 7.51±0.6 | 7.38±0.58 | 0.536 ns |
| Posttreatment | 2.39±0.29 | 1.41±0.188 | 0.001 s | |
| Leg pain | Pretreatment | 6.49±1.55 | 6.79±1.7 | 0.599 ns |
| Posttreatment | 2.39±0.29 | 1.41±0.18 | 0.001 s |
ns-not significant, s-significant.
There is no statistically significant difference between the surgical and conservative group in the mean VAS back pain and VAS leg pain before treatment, while there is statistically significant difference in the mean VAS back pain and VAS leg pain after treatment between the studied groups.
Post-Treatment Complications
Table 13: Post-treatment complication prevalence.
| Characteristics | Conservative Group (n=16) | Surgical Group (n=16) | P values (Fisher Exact Test) |
| Superficial Site Infection | 4(25%) | 1(6%) | 0.166 ns |
| Persistent Back Pain | 5(31%) | 1(6%) | 0.086 ns |
| Leg Pain | 2(12.5%) | 0(0%) | 0.242 ns |
| Urinary Incontinence | 1(6%) | 0(0%) | 0.5 ns |
ns-not significant.
There is statistically significant difference between the surgical and conservative group regarding after treatment superficial site infection, persistent back pain, leg pain, and urinary incontinence.
Discussion
Postoperative Spondylodiscitis is a serious complication of spine surgeries, with marked morbidity, mortality and increase in health care costs. Intervertebral discs can be regarded as largely avascular structures and hence will derive their nutrition from adjacent vertebral endplates. This avascular nature makes it prone to iatrogenic bacterial infection during interventional procedures. Also, aseptic discitis may occur secondary to traumatization of the disc during surgery. While many recent studies showed that post-operative discitis are due to bacterial causes [1]. Most patients at an early stage of pyogenic post-operative discitis can be managed conservatively with immobilization and analgesic drugs along with an appropriate culture guided systemic intravenous antibiotic therapy without the need for surgical intervention. However, surgery is recommended when complications arise like neurological impairment, severe pain or kyphosis, abscess, spinal instability or failure of conservative management [1]. In current study no significant association was detected with age, prevalence was nearly same in both Conservative and surgical group with mean of 43 vs. 44 years respectively. Which is slightly similar to incidence of Stengel et al. and Glassman et al [8,9]. Moreeover, 4:1-5:1 male/female ratio has been demonstrated in studies of Dick and Sponsellar et. al [10,11]. In this study that included 32 patients with male: female ratio was 4:1 in conservative and surgical group. Current study stated that there is a highly significant relationship between gender and outcome. Females have better prognosis according to Chen SH [9], despite the indication for surgery in presence of neurological deficits, age and presence of medical health issues may affect surgical decision [12]. According to Yoshimoto et al. [13], in current study the age less than 40 years/more than 40 years ratio was 9:16 (36%:64%). The study shows that there is statistically highly significant relationship between age and outcome. Age less than 40 years have better prognosis.
Regarding the risk’s factors for POD, there are no significant differences by (fisher exact test) between conservative and surgical group for the risk factors that include DM, smoking, level of discitis, and obesity.
Diabetes Mellitus as a risk factor was seen in 2 cases (12.5%) of conservative group with 1 case (6%) of surgical group and the result was similar to results conducted by Kapsalaki E. et al [17]. The obesity risk factor was seen in 3 cases (18%) of conservative group with 2 cases (12.5%) of surgical group and the result was similar to results conducted by Kapsalaki E. et al [17]. The smoking on the other hand as risk factor was seen 3 cases (18%) of conservative group with 5 cases (31%) of surgical group and the result was similar to results conducted by Kapsalaki E. et al [17]. This research shows a statistically significant relationship between risk factors of discitis and outcome. Other studies that were conducted showed a similar result was done by Rawlings et al. and Yoon et al [5,16]. Regarding the most involved lumbar vertebra in POD, this study showed that L4-L5 was the most involved level with 12 cases (75%) in conservative group versus 11 cases (68%) in surgical group followed by L5-S1 with 3 cases (18%) in conservative group versus 2 cases (12%) in surgical group, while L3-L4 only 1 case (6%) were involved in conservative group versus 3 cases (18%) were affected in surgical group. This level involvement relation indicates that the hypermobile segment was the more risk of POD as well as L4-L5 being the most Discectomies lumbar level. These results were similar to the results of other studies that were reviewed like Stengel D. and glassman et al [8,9].
In addition, current study the presenting history was showing that in conservative versus surgical group that there was not any statistical significant difference between the two groups as it showed that the constant back pain was in 16 cases (100%) in both group, leg radiculopathy 12 cases (75%) versus 15 cases (93%), morning stiffness: 13 cases (81%) versus 15 cases (93%), Lumbar percussion 12 cases (75%) versus 14 cases (87%), the dynamic lumbar pain upon Flexion/ Extension 11 cases (68%) versus 13 cases (81%) and Straight leg raising test: 7 cases (43%) versus 11 cases (68%). The result of this study was similar to other studies that were conducted as Gouliouris et al [14].
This research shows a statistically high significant relationship between presentation of discitis and outcome. Radiculopathy, Claudication, sphincter involvement and fever associated with better prognosis. Known risk factors are previous spine surgery, infectious focus, diabetes mellitus, older age, intravenous drug users, HIV infection, immunosuppression, renal failure, Rheumatologic diseases and liver cirrhosis [20,21]. Controversy arises when there are minor neurological deficits [22-24]. According Pigrau et al., only 13 % patients needed surgery, even though that around 29.7 % of the patients had some neurological symptoms. Pigrau believed that the conservative approach in above scenario is desirable provided that the spine is stable. When neurological symptoms are minor, it's expected to improve with antibiotic-based therapy [22]. Surgical treatment must be performed in presence of sepsis or neurological deficits [25]. Absolute indications of surgery also involve spinal instability due to severe bone destruction, extensive kyphosis, canal spinal lesion with mass effect, active tumours, and failure of conservative management [7,26]. In addition, other authors recommend surgery treatment when there is epidural abscess even in the absence of neurological deficits, especially of cervical and thoracic regions [27]. Regarding the blood serological parameters, according to our study and as compared to other studies, there is no statistically significant difference between the surgical and conservative group in the mean ESR and CRP before treatment, while there is statistically significant difference in the mean ESR and CRP after 1st week, 2nd week,1st month, and 3rd month between the studied group. The ESR mean in 1st week was about (61) in conservative vs. (50) in surgical group, while faster decline was already noticed in 1st month (42) in conservative vs. (26) in surgical group which draws a cut line in improvement around 3-4 weeks' post-treatment.
While CRP, showed a faster and more precise response in management plans than the ESR, as CRP was (65) in conservative vs. (46) in surgical group and almost rapid decline was noted around end of 1st month in CRP as (44) in conservative vs. (22.6) in surgical group, which draws a rapid cut-line in CRP response around 1-2 weeks' post-management. So, the studies came to conclusion that with a microorganism detection rate reaches of up to 65%-95%. The most reliable method remains surgical biopsy [15]. To be more exact Using species-specific PCR as according to, Choi et al. found that it was able to detect around 46,7% of spondylodiscitis cases, whereas about 26,7% could be detected by the use of conventional PCR [15]. This was also evidenced in a retrospective study in which 62.9% could be made using species-specific rather than conventional PCR [25]. while the drawback to PCR whether species specific or conventional PCR, is that I cannot detect nor identify the specificity or sensitivity of microorganism to antibiotics [1]. A large systematic review was conducted on 6701 patients collected from 16 studies to assess the adverse effects on patients underwent intraoperative application of vancomycin powder, the review had concluded with 23 side effects (0.3%) including culture-negative seroma, transient ototoxicity, nephropathy and super-therapeutic exposure. A single case of anaphylactic shock had been reported after application of intra-wound vancomycin [20]. Regarding to the clinically applied Visual Analogue Score, there is no statistically significant difference between the surgical and conservative group in the mean VAS back pain and VAS leg pain before treatment, while there is statistically significant difference in the mean VAS back pain and VAS leg pain after treatment between the studied groups.
Regarding the Post-Treatment Complications, there is statistically significant difference between the surgical and conservative group regarding post-treatment superficial site infection, persistent back pain, leg pain, and urinary incontinence, in which persistent back pain was noticed in 5 cases (31%) in conservative group vs. 1 case (6%) in surgical group, while leg radiculopathy was noticed in 2 cases (12.5%) in conservative group vs. zero case (0%) in surgical group, with one case of urine incontinence registered in conservative group. The strength of my study was in that the lack of similar study to be conducted in the regional area, the duration of the follow up for the cases, the diverse follow up categories for the cases including VAS, Clinical presentations and serological parameters that were used in this study. The limitation of the study is the appropriate but not large of cases that were involved in the study, the difficulty in keeping in touch and following up the cases in which some of them lost connections with the study, the financial status of the patients which delayed or obstructed some of the investigations to be sent.
Conclusion
Most patients at an early stage of pyogenic post-operative discitis can be managed conservatively with immobilization and analgesic drugs along with an appropriate culture guided systemic intravenous antibiotic therapy without the need for surgical intervention. However, surgery is recommended when complications arise like neurological impairment, severe pain or kyphosis, abscess, spinal instability or failure of conservative management.
Recommendations
A vigilant and rapid early diagnosis of post-operative discitis is essential followed by culture-guided administration of prolonged antibiotic treatment. Appropriate monitoring of serial CRP, ESR, clinical state of the patients. Any unresponsive to conservative treatment, may require a rapid surgical intervention which vary from simple debridement to though debridement with Posterior Lumbar Interbody Fusion (PLIF) filled with autogenous cancellous bone grafts and posterior instrumentation of pedicle-screws, that on the contrary to the common belief, will not increase the risk of infections according to many studies.
Declarations
Acknowledgements
None.
Authors' Contributions
Both authors contributed equally in writing and approving this manuscript.
Conflict of Interest
None.
Ethical Approval
Ethical approvals were granted from The Council of Arab Board of Health Specializations in Iraq, AL-Shaheed Ghazzi AL-Harriri hospital of Baghdad Medical city, Erbil teaching hospitals (Rozhawa and Rozhalat trauma emergency hospital) and Erbil Health Department. The study was conducted in accordance with the ethical standards of the Helsinki Declaration of 1975, as revised in 2008.
Informed Consent
Ethically taken in advance.
Funding
None.
References
- Ahsan K, Hasan S, Khan SI, Zaman N, Almasri SS, et al. (2020). Conservative Versus Operative Management of Postoperative Lumbar Discitis. Journal of Craniovertebral Junction and Spine. 11(3):198-209.
Publisher | Google Scholor - Tali ET, Gültekin S. (2005). Spinal Infections. Eur Radiol. 15(3):599-607.
Publisher | Google Scholor - Basu S, Ghosh JD, Malik FH, Tikoo A. (2012). Postoperative Discitis Following Single-Level Lumbar Discectomy: Our Experience of 17 Cases. Indian J Orthop. 46(4):427-433.
Publisher | Google Scholor - Herren C, Jung N, Pishnamaz M, Breuninger M, Siewe J, et al. (2017). Spondylodiscitis: Diagnosis and Treatment Options. Dtsch Arztebl Int. 114(51-52):875-882.
Publisher | Google Scholor - Yao R, Zhou H, Choma TJ, Kwon BK, Street J. (2018). Surgical Site Infection in Spine Surgery: Who Is at Risk? Global Spine J. 8(4 Suppl):5S-30S.
Publisher | Google Scholor - Massie JB, Heller JG, Abitbol JJ, McPherson D, Garfin SR. (1992). Postoperative Posterior Spinal Wound Infections. Clin Orthop Relat Res. (284):99-108.
Publisher | Google Scholor - Abdallah DY, Jadaan MM, McCabe JP. (2013). Body Mass Index and Risk of Surgical Site Infection Following Spine Surgery: A Meta-Analysis. Eur Spine J. 22(12):2800-2809.
Publisher | Google Scholor - Stengel D, Bauwens K, Sehouli J, Ekkernkamp A, Porzsolt F. (2001). Systematic Review and Meta-Analysis of Antibiotic Therapy for Bone and Joint Infections. Lancet Infect Dis. 1(3):175-188.
Publisher | Google Scholor - Glassman SD, Dimar JR, Puno RM, Johnson JR. (1996). Salvage of Instrumental Lumbar Fusions Complicated by Surgical Wound Infection. Spine (Phila Pa 1976). 21(18):2163-2169.
Publisher | Google Scholor - Dick J, Boachie-Adjei O, Wilson M. (1992). One-Stage Versus Two-Stage Anterior and Posterior Spinal Reconstruction in Adults. Comparison of Outcomes Including Nutritional Status, Complications Rates, Hospital Costs, and Other Factors. Spine (Phila Pa 1976). 17(8 Suppl):S310-S316.
Publisher | Google Scholor - Sponseller PD, LaPorte DM, Hungerford MW, Eck K, Bridwell KH, et al. (2000). Deep Wound Infections After Neuromuscular Scoliosis Surgery: A Multicenter Study of Risk Factors and Treatment Outcomes. Spine (Phila Pa 1976). 25(19):2461-2466.
Publisher | Google Scholor - Chen, S. H., Chen, W. J., Wu, M. H., Liao, J. C., Fu, C. J. (2018). Postoperative Infection in Patients Undergoing Posterior Lumbosacral Spinal Surgery: A Pictorial Guide for Diagnosis and Early Treatment. Clinical Spine Surgery, 31(6):225-238.
Publisher | Google Scholor - Rawlings CE, Wilkins RH, Gallis HA, Goldner JL, Francis R. (1983). Postoperative Intervertebral Disc Space Infection. Neurosurgery. 13(4):371-376.
Publisher | Google Scholor - Gouliouris T, Aliyu SH, Brown NM. (2010). Spondylodiscitis: Update on Diagnosis and Management. J Antimicrob Chemother. 65(Suppl 3):11-24.
Publisher | Google Scholor - Choi SH, Sung H, Kim SH, Lee SO, Lee SH, et al. (2014). Usefulness of A Direct 16S rRNA Gene PCR Assay of Percutaneous Biopsies or Aspirates for Etiological Diagnosis of Vertebral Osteomyelitis. Diagn Microbiol Infect Dis. 78(1):75-78.
Publisher | Google Scholor - Yoon SH, Chung SK, Kim KJ, Kim HJ, Jin YJ, et al. (2010). Pyogenic Vertebral Osteomyelitis: Identification of Microorganism and Laboratory Markers Used to Predict Clinical Outcome. Eur Spine J. 19(4):575-582.
Publisher | Google Scholor - Kapsalaki E, Gatselis N, Stefos A, Makaritsis K, Vassiou A, et al. (2009). Spontaneous Spondylodiscitis: Presentation, Risk Factors, Diagnosis, Management, and Outcome. Int J Infect Dis. 13(5):564-569.
Publisher | Google Scholor - Jean M, Irisson JO, Gras G, Bouchand F, Simo D, et al. (2017). Diagnostic Delay of Pyogenic Vertebral Osteomyelitis and Its Associated Factors. Scandinavian Journal of Rheumatology. 46(1):64-68.
Publisher | Google Scholor - Maus U, Andereya S, Gravius S, Ohnsorge JA, Miltner O, Niedhart C. (2009). Procalcitonin (PCT) As Diagnostic Tool for The Monitoring of Spondylodiscitis. Z Orthop Unfall. 147(1):59-64.
Publisher | Google Scholor - Cheung WY, Luk KD. (2012). Pyogenic Spondylitis. Int Orthop. 36(2):397-404.
Publisher | Google Scholor - Nolla JM, Ariza J, Gómez-Vaquero C, Fiter J, Bermejo J, et al. (2002). Spontaneous Pyogenic Vertebral Osteomyelitis in Nondrug Users. Semin Arthritis Rheum. 31(4):271-278.
Publisher | Google Scholor - Sehn JK, Gilula LA. (2012). Percutaneous Needle Biopsy in Diagnosis and Identification of Causative Organisms in Cases of Suspected Vertebral Osteomyelitis. Eur J Radiol. 81(5):940-946.
Publisher | Google Scholor - Foreman SC, Schwaiger BJ, Gempt J, Jungmann PM, Kehl V, et al. (2017). MR and CT Imaging to Optimize CT-Guided Biopsies in Suspected Spondylodiscitis. World Neurosurg. 99:726-734.e7.
Publisher | Google Scholor - Kim CJ, Kang SJ, Choe PG, Park WB, Jang HC, et al. (2015). Which Tissues Are Best for Microbiological Diagnosis in Patients with Pyogenic Vertebral Osteomyelitis Undergoing Needle Biopsy? Clin Microbiol Infect. 21(10):931-935.
Publisher | Google Scholor - Morel AS, Dubourg G, Prudent E, Edouard S, Gouriet F, et al. (2015). Complementarity Between Targeted Real-Time Specific PCR and Conventional Broad-Range 16S rDNA PCR In the Syndrome-Driven Diagnosis of Infectious Diseases. Eur J Clin Microbiol Infect Dis. 34(3):561-570.
Publisher | Google Scholor - Grados F, Lescure FX, Senneville E, Flipo RM, Schmit JL, et al. (2007). Suggestions for Managing Pyogenic (Non-Tuberculous) Discitis in Adults. Joint Bone Spine. 74(2):133-139.
Publisher | Google Scholor - Cornett CA, Vincent SA, Crow J, Hewlett A. (2016). Bacterial Spine Infections in Adults: Evaluation and Management. J Am Acad Orthop Surg. 24(1):11-18.
Publisher | Google Scholor - Enoch DA, Cargill JS, Laing R, Herbert S, Corrah TW, et al. (2008). Value of CT-Guided Biopsy in The Diagnosis of Septic Discitis. J Clin Pathol. 61(6):750-753.
Publisher | Google Scholor - Sharif HS. (1992). Role of MR Imaging in The Management of Spinal Infections. Am J Roentgenol. 158(6):1333-1345.
Publisher | Google Scholor - Prodromou ML, Ziakas PD, Poulou LS, Karsaliakos P, Thanos L, et al. (2014). FDG PET Is a Robust Tool for The Diagnosis of Spondylodiscitis: A Meta-Analysis of Diagnostic Data. Clin Nucl Med. 39(4):330-335.
Publisher | Google Scholor - Ohtori S, Suzuki M, Koshi T, Yamashita M, Yamauchi K, et al. (2010). 18F-Fluorodeoxyglucose-PET For Patients with Suspected Spondylitis Showing Modic Change. Spine (Phila Pa 1976). 35(26):E1599-E1603.
Publisher | Google Scholor - Schmitz A, Risse JH, Grünwald F, Gassel F, Biersack HJ, et al. (2001). Fluorine-18 Fluorodeoxyglucose Positron Emission Tomography Findings in Spondylodiscitis: Preliminary Results. Eur Spine J. 10(6):534-539.
Publisher | Google Scholor