Review Article
Comprehensive Review of Thalassemia Subtypes and Their Adverse Effects: A Deep Dive into Current Literature
1Jefferson Einstein Healthcare Network, Norristown, PA, United States.
2Norton Community Hospital, Norton, Virginia, United States.
3Monmouth Medical Center, Long Branch, NJ, United States.
*Corresponding Author: Supriya Peshin, Norton Community Hospital, Norton, Virginia, United States.
Citation: Shivani S, Peshin S, Masud P, Desai I, Rathod M. (2024). Comprehensive Review of Thalassemia Subtypes and Their Adverse Effects: A Deep Dive into Current Literature, Journal of Hematology Research and Blood Disorders, BioRes Scientia Publishers. 1(1):1-7. DOI: 10.59657/jhrbd.brs.24.003
Copyright: © 2024 Supriya Peshin, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: July 03, 2024 | Accepted: July 17, 2024 | Published: July 22, 2024
Abstract
Thalassemia represents a spectrum of inherited hematologic disorders characterized by aberrant gene function affecting hemoglobin synthesis. Each variant, delineated by its specific hematological manifestation, bears a name indicative of the particular blood constituent impacted. Diagnosis typically involves comprehensive blood and iron level assessments. Complications encompass a broad spectrum, including myelofibrosis, vitamin B12 deficiency, blood-borne infections, Porphyria Cutanea Tarda (PCT), elevated hepatic enzymes, diastolic dysfunction, left ventricular hypertrophy (LVH), chronic thromboembolic pulmonary hypertension (CTEPH), and infections. Management of iron overload necessitates specialized pharmaceutical intervention. Ongoing genetic research offers promising avenues for advancing therapeutic strategies tailored to individuals afflicted by thalassemia. This review delineates the diverse manifestations of thalassemia and their associated clinical implications.
Keywords: thalassemia; hematologic disorders; porphyria cutanea tarda
Introduction
Thalassemia syndromes are genetic disorders that cause an overabundance of a specific type of hemoglobin, leading to its buildup in cells and making them unstable. This instability results in the destruction of red blood cells in the body's periphery and the premature loss of precursor cells involved in making red blood cells, a process called ineffective erythropoiesis. Unlike hemoglobinopathies, most thalassemia doesn’t involve abnormal globin chain structures. Instead, the problem lies in the reduced production of these normal chains, causing a decrease in hemoglobin levels within each red blood cell. This deficiency makes red blood cells smaller, leading to the characteristic appearance of thalassemia with paler coloration and smaller size, similar to other anemias caused by issues in producing heme or globin, the main components of hemoglobin [1,2].
Alpha Thalassemia
Alpha-thalassemia (α-thalassemia) syndromes are hereditary blood disorders that vary in severity. These disorders occur when the body does not produce enough globin chains, which are necessary for making hemoglobin, the protein in red blood cells that carries oxygen. This happens because the genes responsible for making alpha-globin chains on chromosome 16 are dysfunctional, resulting in a decrease in alpha-globin production. As a result, there is an excess of gamma-globin chains in fetuses and newborns, and beta-globin chains in children and adults. Beta-globin chains can form unstable clusters called hemoglobin H (HbH) tetramers, which can damage red blood cell membranes. Additionally, the lack of sufficient hemoglobin content in red blood cells hinders their development in the bone marrow, leading to the production of smaller and paler red blood cells. This condition is medically known as hypochromic and microcytic anemia [3].
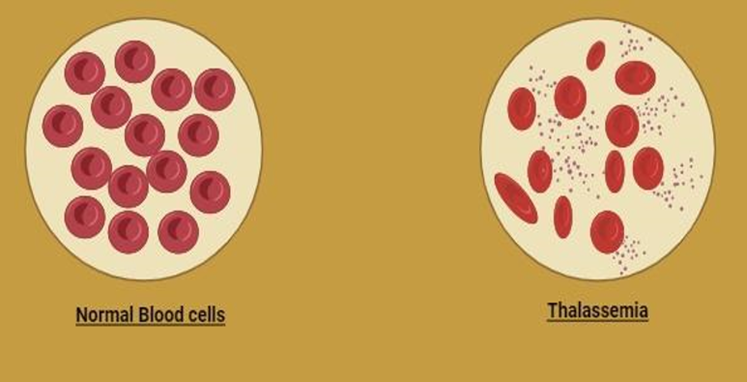
Figure 1: Normal blood cells and thalassemia cells.
Beta Thalassemia
Beta (β) thalassemia is primarily associated with a point mutation in the β globin gene. However, large deletions affecting the β gene and possibly the neighboring δ gene have been observed. Four new mutations, three of which involve the δ gene, were discovered in French patients, resulting in the absence of Hb A2. Distinguishing this condition from the hereditary persistence of fetal hemoglobin (HPFH) is crucial, particularly in prenatal and newborn hemoglobinopathy screening. In severe forms like β thalassemia major, excessive free α chains, due to β chain deficiency, lead to the destruction of red blood cell precursors in the bone marrow, causing ineffective erythropoiesis [4].
Table 1: Classification and Types of Thalassemia.
| Type of Thalassemia | Genetic Cause | Hematologic Manifestation | Key Characteristics |
| Alpha Thalassemia | Deletion of alpha-globin genes on chromosome 16 | Hypochromic and microcytic anemia | Excess gamma-globin in fetuses/newborns; excess beta-globin in children/adults; formation of HbH tetramers |
| Beta Thalassemia | Point mutation in the beta-globin gene | Ineffective erythropoiesis, anemia | Excess free alpha chains leading to red cell precursor destruction |
| Thalassemia Intermedia | Combination of alpha and beta gene mutations | Moderate anemia | Less severe symptoms compared to thalassemia major |
| Thalassemia Major | Severe beta-globin gene mutations | Severe anemia, requiring regular transfusions | Severe symptoms from infancy, frequent transfusions necessary |
How to Identify Thalassemia
The diagnostic process for thalassemia typically begins with a blood profile and iron studies. To confirm the diagnosis, hemoglobin analysis and genetic testing are necessary. Hemoglobin analysis is commonly done through techniques like high-performance liquid chromatography (HPLC) and various hemoglobin electrophoresis methods. HPLC, in particular, is increasingly used in resource-rich settings and can be conducted on a blood spot, similar to newborn screening. Genetic testing can involve gene sequencing or various other methods. The Chinese Gγ(Aγδβ)0-thal beta gene variant is common in southern China, and caution is necessary to prevent misdiagnosis. A Gap Polymerase Chain Reaction (Gap-PCR) system has been developed for the accurate and rapid detection of this mutation, making it a valuable tool with the potential for extended applications due to its simplicity and speed [5]. In distinguishing between iron deficiency anemia (IDA) and beta-thalassemia trait carriers, specific blood parameters, including reticulocyte hemoglobin concentration (CHr), Mean Corpuscular Volume of reticulocytes (MCVr), and detection of beta thalassemia trait (DI-BTT), reveal distinct differences. CHr, MCVr, and DI-BTT exhibit unique distributions in beta-thalassemia trait carriers, making DI-BTT a highly accurate method for differentiation. Simultaneously measuring and analyzing CHr and MCVr indices, along with DI-BTT, enables the effective identification of beta-thalassemia carriers from IDA patients [6]. Preimplantation genetic testing (PGT-M) is a valuable method for gene mapping in beta-thalassemia and sickle cell anemia. Unlike linkage-based methods, PGT-M can identify nearly all beta chain mutations, minimizing the requirement for additional family DNA samples, a significant drawback of linkage-based approaches [7].
Thalassemia-Associated Complications
In cases of thalassemia minor, a blood profile may not always reveal a deficiency in cobalamin (B12), even if it is present. Administering B12 to a thalassemia minor patient with symptoms like leukopenia, hypochromia, and microcytosis can lead to an increase in reticulocyte count and an improvement in anemia symptoms. Thalassemia can conceal the laboratory indications of B12 deficiency. Evidence from bone marrow aspirates is a critical factor in detecting and confirming these observations [8]. Adolescent thalassemia major patients are at higher risk for blood-borne infections, including Hepatitis C (HCV). Detecting HCV in these patients can be challenging. While most patients have Anti HCV RNA antibodies and detectable HCV-RNA in their plasma, some may be HCV seropositive but have negative plasma HCV-RNA. This condition is referred to as occult HCV infection, and in such cases, HCV-RNA can be found in peripheral blood mononuclear cell (PBMC) specimens [9]. Sofosbuvir-based generic direct-acting antivirals (DAAs) are the most effective among the drugs used to treat Hepatitis C. A significant reduction was observed in alanine aminotransferase levels, HCV RNA load, and ferritin levels three months after completing [10]. For beta-thalassemia major patients diagnosed with Hepatitis C and unresponsive to interferon treatment, a 24-week regimen of sofosbuvir (SOF) and daclatasvir (DAC) offers an alternative. During this treatment, liver enzymes decrease, and there is also a reduction in ferritin levels, all with minimal adverse effects [11].
Table 2: Thalassemia-associated Complications.
| Complications | Description | Details |
| B12 Deficiency Concealment | Thalassemia minor can mask B12 deficiency symptoms | Administering B12 can improve anemia symptoms and reticulocyte count; bone marrow aspirates are crucial for detection [8]. |
| Blood-Borne Infections | Higher risk for infections like Hepatitis C (HCV) | Occult HCV infection is detected in PBMCs when plasma HCV-RNA is negative; Sofosbuvir-based DAAs are effective, reducing HCV RNA load and liver enzyme levels [9][10]. |
| Iron Overload | Common in thalassemia treatment, causing multiple complications. | Leads to short stature, pubertal delay, growth hormone deficiency, glucose disorders, subclinical hypothyroidism, and adrenal insufficiency [12]. |
| Myelofibrosis | Increased transfusion needs in thalassemia intermedia | Managed with low-dose steroids, Thalidomide, iron chelation, and potentially splenectomy in severe cases [13]. |
| Porphyria Cutanea Tarda (PCT) | Triggered by iron overload. | Elevated liver enzymes seen in latent PCT; managed with Chloroquine and chelation therapy [14][15]. |
| Cardiac Issues | Diastolic dysfunction, left ventricular hypertrophy, and oxidative stress-induced cardiac injury. | Influenced by genetic factors (GSTM1 null allele, ApoE E-2 allele); iron overload exacerbates risk; chelation therapy improves cardiac T2* and liver iron levels [16]. |
| Pulmonary Artery Hypertension | Elevated vascular endothelial growth factor (VEGF) levels in children with β-thalassemia major. | VEGF levels correlate with pulmonary artery pressure and serum ferritin; indicates presence of pulmonary artery hypertension [17]. |
| Chronic Thromboembolic Pulmonary Hypertension (CTEPH) | Increased risk due to hemolysis, iron overload, hypercoagulable state | Traditional treatments have limited success; balloon pulmonary angioplasty shows promise [18]. |
Iron overload is a serious complication in thalassemia treatment, leading to various adverse effects. Common complications include short stature and pubertal delay. Additionally, issues such as growth hormone deficiency, glucose regulation disorders, subclinical hypothyroidism, and adrenal insufficiency can also arise [12]. Myelofibrosis and hypersplenism contribute to the increased need for transfusions in thalassemia intermedia. Tissue hypoxia and excessive iron deposition are believed to trigger myelofibrosis in these patients. Low-dose steroids, Thalidomide, and iron chelation therapy are effective in managing myelofibrosis. In severe cases, where transfusion frequency remains high, splenectomy may be considered as a last-resort option [13]. Iron overload can be a trigger for Porphyria Cutanea Tarda (PCT). Elevated liver enzymes are commonly seen in latent PCT, as porphyrins gradually accumulate in the liver cells. When treatment with Chloroquine is initiated, there is a temporary increase in porphyrin levels in the blood. Acquired PCT generally has a favorable outcome, with biochemical remission typically achieved within a year [14]. Chelation therapy is used to treat iron overload. When the combination of deferasirox and deferiprone is employed, adherence may be challenging due to side effects like arthralgia and gastrointestinal symptoms. However, after 12 to 18 months of therapy, notable improvements in cardiac T2* and liver iron levels are observed [15].
In beta thalassemia, diastolic dysfunction and left ventricular hypertrophy are observed, influenced by specific genes. The Glutathione S-transferase Mu 1 (GSTM1) null allele and apolipoprotein E (ApoE) E-2 allele are significantly linked to diastolic dysfunction. Serum Glutathione S-transferase (GST) levels also positively correlate with e/a and e/e' ratios. Individuals with the Glutathione S-transferase M1 allele and Apolipoprotein E E2 allele are at a higher risk of experiencing oxidative stress-induced cardiac injury. Cardiomyocytes are highly vulnerable to iron-related complications in Thalassemia major, which is challenging to prevent. Apolipoprotein E and Glutathione S-transferase function as free radical scavengers, combating the excess iron-induced oxidative stress. Variants of Apolipoprotein E (ApoE) and Glutathione S-transferase (GST) may contribute to oxidative damage-related cardiomyopathy. Both iron overload and genetic factors play significant roles in developing cardiac issues in thalassemia patients [16]. In children with β-thalassemia major, those with pulmonary artery hypertension exhibit elevated levels of vascular endothelial growth factor compared to those without this condition. Vascular endothelial growth factor levels are positively correlated with pulmonary artery pressure and serum ferritin, and negatively correlated with the duration of chelation therapy. Elevated vascular endothelial growth factor levels can indicate the presence of pulmonary artery hypertension in children with β-thalassemia major [17].
β-thalassemia, along with other blood disorders, increases the risk of chronic thromboembolic pulmonary hypertension (CTEPH). Hemolysis, iron overload, and a hypercoagulable state play a role in its development. Traditional treatments such as pulmonary endarterectomy and medications have had limited success, but balloon pulmonary angioplasty shows promise as a potential treatment for CTEPH [18].
Thalassemia intermedia (TI) falls between β thalassemia major (TM) and β thalassemia trait in terms of disease severity. Both conditions are associated with osteoporosis, which is linked to hypogonadism and elevated erythropoietin (EPO) levels. Annual intravenous zoledronic acid treatment has proven to be more effective, cost-effective, and less prone to side effects compared to the traditional three-month treatment regimen [19]
Treatment
Genetic advancements present promising treatment options, including the precise DNA base editor CRISPR-Cas9. To mitigate unintended mutations, an engineered enzyme called APOBEC3A, along with its eA3A domain, can be employed. Further research is required to implement these options effectively. In contrast to the BE-3 fusion, the eA3A-BE3 fusion shows comparable editing abilities in cytidines within T Cell (TC) motifs but significantly reduces editing in other sequence contexts. It corrects a human β-thalassemia promoter mutation with over 40-fold higher precision than BE3. This novel technique holds great promise for improving thalassemia treatment [20]. Using fludarabine instead of cyclophosphamide in allogenic stem cell transplants can offer a safer and more effective way to achieve thalassemia-free survival in beta-thalassemia major patients, especially those at high risk. Fludarabine also significantly reduces the chances of transplant rejection [21].
The ATRX protein, which interacts with DAXX, is involved in depositing the replication-independent histone variant H3.3 and plays a crucial role in preserving chromatin integrity. Inherited mutations in ATRX lead to syndromal mental retardation (ATR-X Syndrome), while acquired mutations are linked to myelodysplasia, acute myeloid leukemia (ATMDS syndrome), and various solid tumors [22]. The ATRX gene is situated on the q arm of the X chromosome and is associated with various cancers, including gliomas and neuroendocrine cancers like pancreatic cancer. Monoclonal antibody AMab-6 effectively binds to ATRX, particularly through glycine 2368 (Gln2368), as confirmed by Western blot, enzyme-linked immunosorbent assay (ELISA), and immunohistochemical staining. Utilizing Gln2368 may offer a promising approach for treating alpha thalassemia caused by ATRX gene mutations [23].
In a mouse model, the human β-globin gene (HBB) IVS2-654C >T mutation was introduced and targeted using TALENs vectors to create double heterozygous TALENs+ /β654 mice. Sequencing analysis revealed that the HBB IVS2-654C >T point mutation was eliminated in over 50% of the TALENs+ /β654 mice. Normal β-globin expression in these mice was confirmed through RT-PCR and Western blot. This not only improved hematologic parameters but also reduced the proportion of nucleated cells in the bone marrow. TALENs+ /β654 mice exhibited reduced spleen enlargement, extramedullary hematopoiesis, and iron buildup. These findings strongly support the potential for effectively treating the anemia in TALENs+/β654 mice by eliminating the mutation site using TALENs. This demonstrates a straightforward and promising approach for future gene therapy in β654-thalassemia [24].
An intricate examination of bone marrow transplantation in cases of beta thalassemia major dispels the notion that a combined transplantation approach involving cord blood (derived from a human leukocyte-identical sibling) and granulocyte colony-stimulating factor-primed bone marrow (G-BM) offers notably diminished risks of acute and chronic graft-versus-host disease, accelerates neutrophil recovery, and significantly enhances the likelihood of achieving thalassemia-free survival, in contrast to G-BM transplantation alone [25].
Table 3: Promising Treatments for Thalassemia.
| Treatment Option | Description | Benefits |
| CRISPR-Cas9 and eA3A-BE3 Fusion | Genetic editing tool with precise DNA base modification. The eA3A-BE3 fusion shows high editing precision in specific motifs and corrects β-thalassemia promoter mutation efficiently. | High precision in mutation correction, over 40-fold higher than BE3, especially effective in β-thalassemia. |
| Fludarabine in Allogenic Stem Cell Transplants | Fludarabine used as an alternative to cyclophosphamide in stem cell transplants for beta-thalassemia major patients. | Safer and more effective transplant process, significantly reduces transplant rejection risk, especially beneficial for high-risk patients. |
| ATRX Protein and Monoclonal Antibody AMab-6 | Monoclonal antibody targeting ATRX gene mutations, effectively binding through Gln2368 for treating alpha thalassemia caused by ATRX mutations. | Specific targeting of ATRX, confirmed effective by various assays (Western blot, ELISA, immunohistochemical staining). |
| TALENs for β654-Thalassemia | Gene editing using TALENs to correct HBB IVS2-654C >T mutation in a mouse model. Improved hematologic parameters and reduced spleen enlargement, extramedullary hematopoiesis, and iron buildup. | Effective correction of β654-thalassemia mutations, improved hematologic health in preclinical mouse models. |
| Bone Marrow Transplantation with Combined Cord Blood and G-BM | Combined transplantation approach using cord blood and G-BM for beta thalassemia major. Reduced risks of graft-versus-host disease and enhanced neutrophil recovery | Diminished risks of acute and chronic graft-versus-host disease, faster neutrophil recovery, higher survival rates. |
Conclusion
The advancements in gene therapy have opened up new possibilities for managing thalassemia. While we have achieved impressive milestones in this field, our current focus should be on refining genetic methodologies. This will help us move closer to our ultimate goal of completely eradicating thalassemia with precision and comprehensiveness. By doing so, we can not only improve the prognosis for individuals living with thalassemia but also alleviate the burden of its complications on their lives.
In this review, we have explored the complex landscape of thalassemia, including its various subtypes and their clinical implications. The diverse genetic mutations that cause alpha and beta thalassemias contribute to the complexity of this condition, resulting in a range of hematological abnormalities and systemic complications. We have also discussed the diagnostic and therapeutic advancements in this field, such as the potential of CRISPR-Cas9, TALENs, and innovative approaches to stem cell transplantation. These developments highlight the ever-evolving treatment options that aim to address both the genetic and symptomatic aspects of thalassemia.
Moreover, we have delved into the complications associated with thalassemia, such as iron overload, B12 deficiency concealment, and the increased risk of blood-borne infections. These challenges underscore the multifaceted nature of thalassemia and emphasize the importance of managing these complications through targeted therapies and diligent monitoring. By effectively addressing these issues, we can improve patient outcomes and enhance their quality of life.
In conclusion, while we have made significant progress, our journey towards eradicating thalassemia completely requires continued research and collaboration within the scientific and medical communities. By building upon our existing knowledge and embracing innovative treatment strategies, we can transform the landscape of thalassemia care, providing renewed hope and better health prospects for patients globally.
Declarations
Ethical Approval
No ethical approval is required.
Competing Interests
There are no competing interests of any nature.
Authors' Contributions
S.P., SM wrote the first draft, and S.P, S.M., P.M rearranged and edited the manuscript. P.M, I.D, M.R made tables. M.R, P.M made figure (applicable for submissions with multiple authors).
Funding
No funding is required. This study did not receive any funding in any form.
Availability of Data and Materials
No dataset is required; references are added below for facts used in the manuscript.
References
- Schrier SL. (2002). Pathophysiology of thalassemia. Curr Opin Hematol. 9:123-126.
Publisher | Google Scholor - Ali MAM. (1976). The Hypochromic Anemias. Canadian Family Physician. 22:42-46.
Publisher | Google Scholor - Harewood J, Bhimji SS. (2018). Alpha Thalassemia (Hemoglobin H Disease). StatPearls. StatPearls, Treasure Island (FL).
Publisher | Google Scholor - Day ME, Rodeghier M, DeBaun MR. (2018). Children with HbSβ0 thalassemia have higher hemoglobin levels and lower incidence rate of acute chest syndrome compared to children with HbSS. Pediatr Blood Cancer. e27352.
Publisher | Google Scholor - Zhang Q, Zhang Y, Xu H, Xu M, Wen X, Xu X, et al. (2018). Genetic and phenotypic analysis of a rare case with homozygous Chinese Gγ (Aγδβ)0-thal deletion. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 35:553-556.
Publisher | Google Scholor - Vicinanza P, Vicinanza M, Cosimato V, et al. (2017). Mean reticolocyte hemoglobin content index plays a key role to identify children who are carriers of β-thalassemia. Transl Med UniSa, 17:34-39.
Publisher | Google Scholor - Sock-Myer S, Johnson M. (2018). A big step forward for PGT-M? Reprod Biomed Online. 37:126-127.
Publisher | Google Scholor - Kurdi B, Mezei ZA, Kellner Á, Egyed M. (2018). Pernicious anemia in a thalassemic patient - difficulties of the diagnosis. Orv hetil. 159:1368-1371.
Publisher | Google Scholor - Kahyesh-Esfandiary R, Sadigh ZA, Esghaei M, et al. (2018). Detection of HCV Genome in Peripheral Blood Mononuclear Cells of Iranian Seropositive and HCV RNA negative in Plasma of Patients with Beta-thalassemia Major: Occult HCV Infection. J Med Virol.
Publisher | Google Scholor - Nagral A, Jhaveri A, Sawant S, Parikh NS, Nagral N, Merchant R, et al. (2019). Treatment of Chronic Hepatitis C Infection with Direct Acting Antivirals in Adolescents with Thalassemia Major. Indian J Pediatr.
Publisher | Google Scholor - Zamani F, Ajdarkosh H, Safarnezhad-Tameshkel F, Azarkeivan A, Keyvani H, et al. (2018). The effectiveness of sofosbuvir and daclatasvir in the treatment of hepatitis C in thalassaemia major patients and their effect on haematological factors. Indian J Med Microbiol, 36:224-229.
Publisher | Google Scholor - Dhouib NG, Ben Khaled M, Ouederni M, Besbes H, Kouki R, et al. (2018). Growth and Endocrine Function in Tunisian Thalassemia Major Patients. Mediterr J Hematol Infect Dis. 10:e2018031.
Publisher | Google Scholor - Nirupam N, Maheshwari A, Rath B, Chandra J, Kumar P, et al. (2012). Myelofibrosis: a cause of increased transfusion requirement in a child with β-thalassemia intermedia. J Pediatr Hematol Oncol. 34:143-145.
Publisher | Google Scholor - Stockenhuber F, Kurz R, Grimm G, Moser G, Balcke P. (1990). Successful treatment of hemodialysis-related porphyria cutanea tarda with deferoxamine. Nephron. 55:321-324.
Publisher | Google Scholor - Elalfy MS, Adly AM, Wali Y, Tony S, Samir A, et al. (2015). Efficacy and safety of a novel combination of two oral chelators deferasirox/deferiprone over deferoxamine/deferiprone in severely iron overloaded young beta thalassemia major patients. Eur J Haematol, 95:411-420.
Publisher | Google Scholor - Singh MM, Kumar R, Tewari S, Agarwal S. (2018). Association of GSTT1/GSTM1 and ApoE variants with left ventricular diastolic dysfunction in thalassaemia major patients. Hematology. 10:1-6.
Publisher | Google Scholor - Alkholy UM, Mohamed SA, Elhady M, Attar SE, Abdalmonem N, Zaki Aet al. (2019). Vascular endothelial growth factor and pulmonary hypertension in children with beta thalassemia major. J Pediatr.
Publisher | Google Scholor - Karyofyllis P, Tsiapras D, Papadopoulou V, Diamantidis MD, Fotiou P, et al. (2018). Balloon pulmonary angioplasty is a promising option in thalassemic patients with inoperable chronic thromboembolic pulmonary hypertension. J Thromb Thrombolysis.
Publisher | Google Scholor - Darvishi-Khezri H, Kosaryan M, Akbarzadeh R, Aliasgharian A, Fazli M. (2018). Administration of Intravenous Zoledronic Acid Every 3 Months vs. Annually in β-thalassemia Patients with Low Bone Mineral Density: A Retrospective Comparison of Efficacy. Med Arch. 72:170-173.
Publisher | Google Scholor - Wattanapanitch M, Damkham N, Potirat P, et al. (2018). One-step genetic correction of hemoglobin E/beta-thalassemia patient-derived iPSCs by the CRISPR/Cas9 system. Stem Cell Res Ther. 9:46.
Publisher | Google Scholor - Gehrke JM, Cervantes O, Clement MK, et al. (2018). An APOBEC3A-Cas9 base editor with minimized bystander and off-target activities. Nat Biotechnol.
Publisher | Google Scholor - Truch J, Telenius J, Higgs DR, Gibbons RJ. (2018). How to Tackle Challenging ChIP-Seq, with Long-Range Cross-Linking, Using ATRX as an Example. Methods Mol Biol. 1832:105-130.
Publisher | Google Scholor - Kaneko MK, Yamada S, Itai S, et al. (2018). Epitope mapping of an anti-alpha thalassemia/mental retardation syndrome X-linked monoclonal antibody AMab-6. Biochem Biophys Rep. 15:76-80.
Publisher | Google Scholor - Ma N, Liao B, Zhang H, et al. (2013). Transcription activator-like effector nuclease (TALEN)-mediated gene correction in integration-free β-thalassemia induced pluripotent stem cells. J Biol Chem. 288:34671-34679.
Publisher | Google Scholor - Wen J, Haque Q, Pei F, et al. (2018). Transplant Outcomes in Beta-Thalassemia Major Patients Receiving Combined Granulocyte Colony-Stimulating Factor-Primed Bone Marrow and Cord Blood Graft Compared to Granulocyte Colony-Stimulating Factor-Primed Bone Marrow Alone. Acta Haematol. 140:20-29.
Publisher | Google Scholor