Research Article
Comparison of the Recurrence Rate in Marsupialization with and Without Peripheral Sectomy in the Treatment of Odontogenic Keratocyte Tumor in Patients Referred to Bahoner Hospital, Kerman
1Resident in the Department of Oral and Maxillofacial Surgery, Bahnar Hospital, Kerman, Iran.
2Assistant Professor, Department of Oral and Maxillofacial Surgery, Bahnar Hospital, Kerman, Iran.
*Corresponding Author: Arian Yeganeh,Resident in the Department of Oral and Maxillofacial Surgery, Bahnar Hospital, Kerman, Iran
Citation: Yeganeh A, Mahmoodi M, Fardisi S. (2023). Comparison of the Recurrence Rate in Marsupialization with and without Peripheral Sectomy in the Treatment of Odontogenic Keratocyte Tumor in Patients referred to Bahoner Hospital, Kerman. Dentistry and Oral Health Care, BioRes Scientia Publishers, 2(3):1-10. DOI: 10.59657/2993-0863.brs.23.013
Copyright: © 2023 Arian Yeganeh, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 19, 2023 | Accepted: August 31, 2023 | Published: September 02, 2023
Abstract
Aim: Odontogenic keratocyte tumor is a developmental cyst with proliferative and invasive nature. which is often observed in the posterior region of the mandible and is commonly seen in the third decade of life. The highest age of prevalence is in the 3rd to 6th decades and the male to female ratio is 2 to 1. Normally, if there is no infection, it is not manifested and it is discovered accidentally in rayograph, but if the size increases, it manifests as an extension in the form of pain, swelling and infection in the dental and bone area if the tooth is hidden. In radiographs, it appears as a radiolucent lesion with distinct ionic or multilocular boundaries and sometimes with a scallop border in the dental area or even extending to the ascending ramus and condylar area. Research shows that the origin of this cyst is the remaining odontogenic epithelium of Ceres in the alveolar region. And it can be syndromic (Gorlin syndrome) or non-syndromic. This cyst has a thin epithelium and has multiple daughter cysts, which causes the risk of recurrence due to incomplete removal of the lesion. Enucleation, marsupialization, Carney’s solution and resection are treatment methods. What is investigated in this project is the comparison of the prevalence of the two therapeutic methods of marsupialization alone and the combination of marsupialization and peripheral sect my in patients with odontogenic keratocytes regardless of whether they are syndromic or sporadic.
Method and Materials: In this study, which is conducted on 10 patients referred to Behoney Hospital in Kerman. First, the patient is selected with clinical examinations and then with the preparation of panoramic radiographs. If there is visible swelling, aspiration is performed with a 10-cc syringe, and then the patient is operated on for a biopsy to definitively diagnose the odontogenic keratocyte of the tumor. In this study, there is no difference between the age and sex of the patient, and whether KOT is syndromic or sporadic; Both are included in the review. The patient is subjected to marsupialization, then the patient undergoes follow-up and periodic x-rays are used to ensure that the lesion shrinks. In the lesions where there is involvement of the surrounding bone in the form of a saucerization, after the lesion is reduced, the patients are treated with peripheral sect my or removal of the bone around the lesion in the form of a curt shape, and in small lesions, the treatment is completed with marsupialization. arrives. Then the patients are followed up and the recovery process and the rate of recurrence are checked by preparing periodical x-rays.
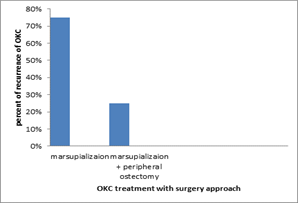
Results: In this study, out of ten patients, 4 patients (40%) had recurrence, and among these 4 patients, 3 patients (75%) were in the first group who were treated with marsupialization. The follow-up of the patients was one year, and after the preparation of OPG, the reduction of cyst dimensions was compared to the size before the operation. The criterion for the recurrence of keratocyte odontogenic lesion is the increase in the size of the lesion according to the qualitative scale and the comparison of the graph prepared before and after marsupialization. Out of 4 patients with recurrence, one case in the second group (25%) is treated with marsupialization and peripheral sitcom, a ten-year-old boy has multiple jaw cysts in the front of the mandible, behind the maxilla on both sides, and behind the mandible on both sides. The maxillary sinus is left. According to the obtained results, the treatment of marsupialization with peripheral sect my has more effectiveness and the results had a significant difference. p value=0.043
Conclusion: According to the obtained results, the treatment of marsupialization with peripheral sitcom has more effectiveness and less recurrence.
Keywords: odontogenic keratocyte tumor; marsupialization; peripheral sectomy; recurrence
Introduction
Odontogenic keratocyte (OKC) is a benign and rare tumor, but it is usually classified as a locally invasive developmental cyst. This cyst is often in the posterior region of the mandible and commonly manifests in the third decade of life. (1) Odontogenic keratocyte accounts for about 19% of maxillary cysts. And according to the latest World Health Organization (WHO) classification, it is classified as a cyst. This cyst often affects the lower jaw. (2) Odontogenic keratocytes make up about 19% of jaw cysts. In the WHO/IARC classification of head and neck pathology, this clinical entity was known as odontogenic keratocyte for many years. From 2005 to 2017, it was classified as keratocyte odontogenic tumor (KCOT). (3) and (4) returned to its previous name in 2017. Signs and symptoms: Primary odontogenic keratocytes usually show no symptoms. Typically, clinical signs and symptoms appear with bone spread or infection. However, bone expansion is uncommon because odontogenic keratocytes grow due to increased epithelial turnover rather than osmotic pressure. When symptoms are present, they usually appear as pain, swelling, and discharge from secondary infection. Odontogenic keratocytes are usually noted as incidental radiographic findings. Radiographically, they can be seen as single or multi-cavity radiolucency’s. If they are present on a tooth that has not erupted, they may be confused with other cysts such as residual cysts or dentigerous cysts. (5)
Pathogenesis: Odontogenic keratocytes originate from the odontogenic epithelium (dental lamina) in the remaining alveoli from the stages of tooth development. They are thought to originate mainly from other regions of the cereus. (6) OKC originates from remnants of the dental lamina in the mandible and maxilla before odontogenesis is complete. They may also originate from the basal cells of the covering epithelium. (7) The distribution between genders varies from gender equality to a male to female ratio of 1.6:1. Except in children, OKC may occur in any part of the maxilla and mandible, with a majority in the mandible and mostly in the mandibular angle and ramus. (2) OKC comprises approximately 11% of all cysts in the jaw, and can present with impacted third molars. From the point of view of radiography, it appears as single or multi-cavity. (8) From the point of view of radiography, OKCs are well-defined single or multi-cavity radiolucency’s with smooth margins and often with a tendency to grow in the anterior-posterior direction inside the medullary cavity of the bone without creating Clear expansion of the bone and displacement of the teeth adjacent to the cyst occur more often than resorption. (9) OKCs, the upper jaw is smaller compared to the lower jaw. (10) These lesions can also appear as a small, oval radiolucency between the teeth, simulating a lateral periodontal cyst, and can also appear as a residual periapical cyst-like radiolucency.
Genetics: Sporadic (non-syndromic) and syndromic OKCs are associated with mutations in the PTCH gene found on chromosome 9q, which is part of the hedgehog signaling pathway. (4), (11), (12) PTCH is a tumor suppressor gene. Is. Loss of PTCH activity results in cell cycle arrest. One-third of OKCs show mutations in PTCH, resulting in the cyst epithelium undergoing highly proliferative activity. This leads to the growth of the cyst wall and, if removed, causes recurrence if the epithelium is incompletely removed. (13) The PTCH gene is located on chromosome 9q22.3-q31 and probably acts as a tumor suppressor. (14), (4) Studies on sporadic NBCCS and KCOT have been performed. Molecular evidence of a two-hit mechanism in the pathogenesis of these tumors shows allelic loss, at two or more loci, of 9q22 19, leading to bill overexpression. -1 and TP53 in NBCCS. (15) Other genes that can be associated with OKC/KOT are PTCH2 and SUFU. A few authors have also shown its loss, heterozygosity in p16, MCC, TSLC1, LTAS2 and FHIT genes (16) are useful to explain the aggressive behavior of orc.
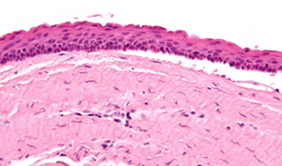
Diagnosis: Diagnosis is usually radiological. However, definitive diagnosis is through biopsy. Aspiration biopsy of odontogenic keratocytes contains oily fluid that is pale in color and has keratotic crusts. (2), (17) The protein content of the cyst fluid is less than 4 grams in the diagnosis of odontogenic keratocytes. (2) Smaller and unilocular lesions. which are similar to other types of cysts, they may need a biopsy to confirm the diagnosis. (6) In CT scan, the radioactive density of keratocyte odontogenic tumor is about 30 Hounsfield units, which is almost equal to ameloblastoma. However, ameloblastoma shows more bony expansion and rarely shows areas of high density. (18) Guerlain syndrome: Guerlain syndrome is a rare genetic disease. In 1894, Janisch and White identified this syndrome with patients with learning disabilities, scoliosis, and BCC of Gorlin and Goltz's classic triad. The diagnosis of this syndrome (19,20) was later made in 1960 by Rayner et al. with diagnostic criteria including falx calcification. The pits on the palms and feet were corrected. (21,22) In radiographs, odontogenic keratocytes show well-defined radiolucent areas with well-defined rounded or scalloped margins. (17) These areas can be multi-cavity or single-cavity. The growth pattern of the lesion is very distinct from which it can be recognized as the growth is present and extends anteriorly and posteriorly along the medullary cavity with little extension. No analysis is seen in the lower teeth or dental canals, and minimal displacement of the teeth is seen. Due to the non-expansion of odontogenic keratocyte, the lesion can be very large if detected radiographically. Extensive waste. In more than 40% of cases, it is associated with the remaining tooth crown. (24) It rarely appears as a radiolucent interradicular image or radicular circumambulation and is associated with vital teeth. - Clear and thin borders, with or without peripheral sclerotic halo. (25, 26) In some cases, when it is associated with tooth retention, they look like dentigerous cysts on radiographs. Multi-cavity lesions resemble ameloblastoma, and smaller lesions resemble residual cysts, lateral periodontal cysts, and radicular cysts. (27) Histology Odontogenic keratocytes have a diagnostic histological appearance. Under the microscope, OKCs vaguely resemble keratinized squamous epithelium; (28) However, they lack re-protrusions and often have artificial separation from their basement membrane. (2) Histologically, OKC presents two broad types. The first is Para keratinized orc, with a thin stratified surface epithelium, usually 8-10 layers thick, and a Para keratinized, wavy surface. It also has a flat epithelium-connective tissue interface, i.e., no dermal-epithelial depression, where basal cells have hyperchromatic, polarized nuclei arranged in rows. The second type, Ortho keratinized cyst, is less common and has a thin, granular epithelial lining and a thicker, undulating orthoceratid lining, with a keratinized lumen and basal cells that are difficult to distinguish. (29,30) Some lesions show both parakeratotic and orthokeratosis areas. (27), (31), (32) Both types of histology show different clinical behaviors. Ortho keratin cysts have a lower growth potential and recurrence rate and are often associated with residual teeth. From the point of view of radiography, they are often single-cavity and are located in the maxillary or anterior region of the mandible (33). The fibrous wall of the cyst is usually thin and without inflammation. The thin epithelial lining is uniform in thickness and is Para keratinized with columnar cells in the basal layer that have focal reverse polarity (nuclei are located at the opposite pole of the cell). (17) Basal cells are indicative of odontogenic origin because they resemble pre-ameloblasts. are. The epithelium can detach from the wall, resulting in epithelial islands. These can form "satellite" or "daughter" cysts, leading to an overall multipoint cyst. (6) The presence of daughter cysts is especially seen in patients with NBCCS. Inflammatory cysts show hyperplastic epithelium that is no longer characteristic of OKCs and can instead resemble radicular cysts. Due to the areas of focal inflammation, a larger biopsy is required for the correct diagnosis of odontogenic keratocytes. (6).
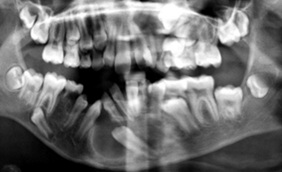
Figure 1: Odontogenic Keratocyte in Anterior Mandible, 10 Years Old Patient
Figure 2: Odontogenic Keratocyte, Incisional Biopsy, Histologic Show
Treatment: Because this disease is so rare, experts have different opinions on how to treat OKC. A 2015 Cochrane review found that there is currently no high-quality evidence to demonstrate the effectiveness of specific treatments for odontogenic keratocytes. (5) Treatment depends on the degree of multilocularity of the cyst. Small multilocular and unilocular cysts can be treated more conservatively by enucleation and curettage. Treatment options for KTOC may vary depending on its size, extent, location, and adjacent structures.
Treatment options (4,5,6) Surgical drainage: surgical removal of the entire epithelial lining of the cyst. Marsupialization followed by enucleation: This procedure is performed by surgeons for larger cysts. Cartage involves simple removal and scraping of the cavity. Carney’s fixative solution (ethanol, chloroform, and acetic acid), which is usually used with oxygen and curettage. The cavity wall can be treated with a fixator or added to the bony walls before drainage to remove the wall covering or after curettage and remove the remaining epithelial cells to a depth of 1-2 mm. It is used with caution near the mandibular canal and the neurovascular bundle inside it. Marsupialization, which involves surgically opening the cyst cavity and creating a sac-like cavity. This allows the cavity to be in contact with the outside of the cyst for a long time. Marceau leads to a slow contraction of the cyst, allowing for subsequent evacuation. However, regression can take up to 20 months and patients must have the open cavity cleaned and irrigated.
Easy removal Enucleation and cryotherapy. (34) It has been shown that decompression followed by enucleation is more successful with the lowest rate of recurrence. (35) Local application of 5FU after enucleation (36) Ostectomy or block removal: In addition to the above treatments, treatment may be required due to disease recurrence. Ostectomy is removal of peripheral bone. Removing the block means removing the cyst with the surrounding tissue. Extensive cysts may require bone grafting after bone removal and reconstruction of the area. Follow up: Annual radiographic examination is recommended. (17) Long-term clinical follow-up is also recommended due to recurrences that occur several years after treatment. (2) Recurrence and neoplastic nature: Malignant transformation to squamous cell carcinoma may occur, but is uncommon. (37) The incidence of OKC recurrence has varied from 2.5% to 62%. (28) The large degree of variability in these reports is mainly because some of the series of cysts in patients with novia basal cell carcinoma syndrome (NBCCS), while other reasons for this variation could be due to the length of the follow-up period and the treatment method used. (28) In 1976, Brannon (34) Three mechanisms have been proposed for OKC recurrence: incomplete removal of the cyst lining, growth of a new OKC from satellite cysts or odontogenic breaks after surgery, and development of a new OKC in an adjacent area. Histopathological features predict recurrence. Recurrence is likely when treated with simple enucleation. Factors involved are: thin and fragile epithelium leading to incomplete removal, extension of the cyst to the cancellous bone, satellite cysts found in the wall, experience of the surgeon, formation of new cysts more than other remnants of the dental epithelium. With current treatments, the recurrence rate is about 2-3%, but can be as high as 50%. Recurrence can occur as early as 5 years and as late as 40 years after resection. Recurrence is usually observed within 5 years after treatment. Early findings of recurrence can be easily treated with minor surgery and curettage. (6) Any piece of cyst that remains has the potential to survive and grow. Therefore, the success of enucleation depends on how well the cyst is removed. Larger cysts are more likely to recur after drainage because they are more difficult to remove.
Methods and Materials
Cross-sectional descriptive research is conducted on patients referred to Bahonar Hospital in this city. Verbal consent was obtained from patients with odontogenic keratocyte tumors who are willing to be treated and cooperate in the research to participate in the research, and the research protocol will be reviewed and approved by the ethics committee in medical research of Kerman University of Medical Sciences. After obtaining the necessary permits and inviting patients to attend the examinations, and examinations by the resident of the final year of oral, maxillofacial and facial surgery under the supervision of the faculty member of the Faculty of Dentistry who has received the necessary training and the reliability of the results of his calculations before the implementation Research and it has been confirmed in the experimental investigation, it is done. In this study, which is conducted on patients referred to Behoney Hospital in Kerman. First, the patient is selected by clinical examination and then radiography. In case of visible swelling, aspiration is performed with a 10-cc syringe, and then the patient is operated on for a biopsy to definitively diagnose odontogenic keratocytes. In this study, the patient's age and sex do not differ, and whether OKC is syndromic or sporadic is both included in the study. Then, based on the size of the lesion and the extent of destruction and its progress, after receiving the definitive result of the biopsy by the pathology laboratory of the Kerman School of Dentistry, the patient is subjected to marsupialization. and after exposure of the bone involved in the cyst using a medium-sized fissure bur, a cavity is created in the bone after the discharge of a yellow, cheesy liquid, if there are septa in the lesion, the septa are connected to each other and the bone walls are burred with a bur It is removed between the holes in the multilocular type. Then the area is completely washed with sterile normal saline and a drain is made using the end of the suction tube, 4 to 5 mm long depending on the depth of the cavity. The reason for using a suction tube or a similar device is the rigidity of the device. After that, a 0-3 drain is sutured to the walls of the cyst and oral mucosa with a silk thread so that the cavity has a way to drain the substance and wash it. And the rest of the cut area is also sutured. Then, an acrylic fit cap is installed in the head of the drain so that the food does not contaminate the cavity when the patient eats. Then, the patient undergoes follow-up and periodic x-rays are used to ensure that the lesion shrinks. In lesions where there is involvement of the surrounding bone in the form of a saucerization, after the lesion is reduced, the patient is re-created with a drain and from the same place, and a subperiosteal dissection is performed, and with a medium-sized fissure bur, they are treated with peripheral ostectomy or removal of the surrounding bone. Lesions are curt-shaped, and in small lesions, the treatment is completed with marsupialization. Then the patients are followed up and the recovery process and the rate of recurrence are checked by preparing periodical x-rays. For this purpose, 10 patients were selected from the patients who referred to the outpatient clinic of Bahonar Hospital and divided into two groups randomly and without restrictions. Gender and age were selected. In the first group, which included three men aged 30 to 40 years and two women aged 25 and 31 years, were selected. And in these patients, by confirming the presence of keratocytes odontogenic lesion by biopsy and preparing a panoramic radiograph of the said lesion, which was located in the mandible in the angle region (distal third molar) up to half of the ascending ramus, and the discharge of cheesy fluid from the gingival sulcus of the 8 semi-implanted tooth was observed under were treated with marsupialization. The second group, which includes a woman with an average age of 42 years and a boy with the age of ten years who has the symptoms of Guerlain's syndrome (cerebral sickle - heart valve insufficiency), who has a KOT lesion in the mandibular region on the right side of the tooth alignment. The first premolar to the first molar, and in the boy, there are numerous cysts in the front of the mandible and behind the mandible on two sides and behind the maxilla on both sides. And two men with an average age of 40 years and one man with an average age of 36 years were selected with a lesion in the front of the mandible in the alignment of the 2 lower left to 2 lower right teeth and behind the right mandible from the alignment of the second premolar to the distal first molar. In this group, marsupialization was performed after confirming the existence of the lesion with biopsy, and after 6 months of initial treatment and drainage, peripheral sitcom treatment including removal of the bone surrounding the lesion along with the lesion was performed in those two patients. And all the patients in both groups started their treatment about a year ago and are under follow-up. And every 6 months, a panoramic radiograph is taken. The criterion of recurrence of the lesion in this study is the enlarging of the cyst dimensions in the X-ray and the discharge of cheesy liquid from the gum and the observation of swelling after recovery. Considering that after removing the lesion for about 6 months and going through the process of bone calcification and its appearance in the graph and the formation of fetal bone and then adult bone, the size of the radiolucency does not change significantly in this research due to the expansion of the lesion and the outflow of fluid and increase Swelling size is treated as a variable as a symptom of recurrence and lack of improvement. In this study, attention will be paid to the percentage of lesion recurrence and how much progress has been observed in each group. Data extraction tools: 1- Clinical examinations: All patients are examined in the maxillofacial outpatient clinic in Bahnaz Hospital by the operator of the examination plan and the graphs prepared by him. 2- OPG (panoramic) radiography is obtained from all patients in the radiology department of Behoney Hospital, and the radiology staff prepares the radiography. A fixed device with certain settings is used in the radiology department of Bahonar Hospital to perform the radiography. 3- Biopsy of the lesion and then marsupialization and peripheral ostectomy treatments are performed by the oral and maxillofacial surgeon, who is the project manager and supervisor, in the operating room of Bahonar Hospital under general anesthesia. 4- Radiographic examination of the lesion and follow-up of the patients in the follow-up periods and comparison of the panoramic graphs obtained to check the recovery of the lesion and the creation or non-spreading of the lesion and the effectiveness of the treatment by the oral and maxillofacial surgery resident who is a project collaborator and student. is done and the creation of bias is avoided as much as possible. The sample size is the patients who referred to the maxillofacial surgery outpatient clinic with the diagnosis of odontogenic keratocytes tumor. 10 patients at the discretion of the supervisor who is the project manager and according to whether the patients live in the city and the surrounding villages of Kerman and if the sample size increases, it was not possible to access all the patients and some of them due to lack of treatment costs or The presence of family problems or surgery phobia were excluded from the study, they were selected in two groups without age and gender restrictions, for this purpose, 10 patients were selected from the patients who referred to the outpatient clinic of Bahonar Hospital and were randomly divided into two groups. It was selected without gender and age restrictions. In the first group, which included three men aged 30 to 40 years and two women aged 25 and 31 years, were selected. And in these patients, by confirming the presence of keratocytes odontogenic lesion by biopsy and preparing a panoramic radiograph of the said lesion, which was located in the mandible in the parasite region (distal third molar) up to half of the ascending ramus, and the discharge of cheesy fluid from the gingival sulcus of the 8 semi-implanted tooth was observed under were treated with marsupialization. The second group, which includes a woman with an average age of 42 years and a boy with the age of ten years who has symptoms of Guerlain syndrome (cerebral sickle - heart valve insufficiency) and has an orc lesion in the mandibular region on the right side of the tooth alignment. The first premolar to the first molar, and in the boy, there are numerous cysts in the front of the mandible and behind the mandible on two sides and behind the maxilla on both sides. And two men with an average age of 40 years and one man with an average age of 36 years were selected with a lesion in the front of the mandible in the alignment of the 2 lower left to 2 lower right teeth and behind the right mandible from the alignment of the second premolar to the distal first molar.
| Number | Variables | Scientific Definition | Variable type Quantities/Qualitive Dependent/ Independent | Measurement | Measurement Unit |
| 1 | Recurrence of Lesion | Qualitive / Dependent | Clinical Examinations | Qualitive | |
| 2 | Percent of Recurrence of Lesion | Quantities / Dependent | OPG Exploration | Quantities |
Table 1: Table of variables
Results
In this study, 10 patients including 6 men in the age range of 30-40 years and three women aged 25, 31 and 42 years without any problems and systemic disease and ASA1 and a ten-year-old boy with Guerlain syndrome with heart failure including mitral valve prolapse in ASA2 category were investigated. In all patients, clinical examinations were performed by the supervisor, and after taking OPG radiographs and, if necessary, preparing a CT scan, the pre-clinical examination form was completed. Then the patients were subjected to marsupialization treatments in one round to perform biopsy and then after confirmation of odontogenic keratocytes and another group underwent marsupialization treatment along with peripheral sitcom. In this study, out of ten patients, 4 patients (40%) had recurrence, and among these 4 patients, 3 patients (75%) were in the first group who were treated with marsupialization. The follow-up of the patients was one year, and after the preparation of OPG, the reduction of cyst dimensions was compared to the size before the operation. The criterion for the recurrence of keratocytes odontogenic lesion is the increase in the size of the lesion according to the qualitative scale and the comparison of the graph prepared before and after marsupialization. 3 patients in whom recurrence occurred, including a 32-year-old male patient in the left mandibular area in the distal tooth 8, which can be considered as the cause of the recurrence due to lack of access to the area, the mucosal section of the area was not complete, and it was not possible to completely suture the epithelial wall. There were no cysts in the oral mucosa. Drainage in that area was not completely successful, and the drain had to be changed twice due to lose connections with the mucosa and its exit. Also, after repeated weeks of checking and the absence of cheesy discharge from the drain, according to the patient's own report, the drain was diagnosed as non-functional and had to be replaced. Another patient in whom recurrence is observed is a 40-year-old man who has an odontogenic lesion of keratocytes in the region of the parasite to the ascending half of the right ramus. The lesion was swollen with expansion in the right parasite area, in this case, after cutting the area and exposing the cyst, two septa that were seen in the radiograph were seen in the cyst area. But in this area too, due to the lack of access and the inability to wash the patient, the drain did not have enough function. And had to change. And after a one-year follow-up, the size and dimensions of the lesion had expanded and the tendency to expansion in the parasite area had increased. And the patient reported the discharge of cheesy secretions from more areas. The next case was a 25-year-old woman with a lesion in the area of the second premolar to the right second molar. The patient had cancer phobia, and according to the explanation about the disease and the type of cyst, the patient's fear of surgical procedures decreased, but it still persisted. The lesion had bone destruction and thinned the cortical bone of the buccal plate. Due to the size of the lesion and the invasion of the cortex, two drains were placed in the area and the teeth involved in the lesion had preserved their vitality. And their vitality was confirmed by cold and heat test. However, in the follow-up of the patient and the preparation of radiographs, the enlargement of the lesion was evident, and one of the two drains did not discharge secretions. But in the other 2 patients treated with marsupialization (40%), the treatment was successful and the size of the lesion was reduced and the effects of embryonic bone formation and adult bone formation were evident after one year of treatment. The discharge of cheesy secretions had disappeared and the swelling had decreased in expansive cases. Out of 4 patients with recurrence, one case in the second group (25%) is treated with marsupialization and peripheral sitcom, a ten-year-old boy has multiple jaw cysts in the front of the mandible, behind the maxilla on both sides, and behind the mandible on both sides. The maxillary sinus is left. First, marsupialization treatment was performed and drainage was performed. The patient was 7 years old at the time of the treatment and the child's cooperation was low. Drain washing training was given to the patient's mother and the patient himself. Due to his young age, the patient had to change the drain several times. On the other hand, the patient had a heart condition and had to go to Tehran for additional cardiovascular examinations during the treatment period. And after returning to the outpatient maxillofacial clinic of the hospital and examining the patient's lesions by preparing OPG and CBCT and the appearance of a new lesion in the maxillary sinus area, the patient underwent follow-up. In other areas, the shrinking of the lesion and the reduction of the size of the cyst were evident, and then with the shrinking of the lesions, a decision was made to remove the cysts and remove the bone around them. Then the patient underwent follow-up, and unfortunately, the recurrence of the lesion was seen in the posterior region of the left maxilla in the X-ray. And maybe the reason for recurrence was the lack of access to the lesion to remove the cyst, as well as the involvement of the sinus in that area. Also, due to the young age of the patient, the patient's mother preferred not to bring the child to the clinic for examination. 4 other patients in the second group (80%) treated with marsupialization and peripheral sitcom have been fully treated and recovered. The lesions were completely removed and the secretions stopped. According to the obtained results, the treatment of marsupialization with peripheral sitcom has more effectiveness and the results had a significant difference. P-value =0.043.
| Groups | Patient /Percent of recurrence OKC | Recurrence Rate Qualitatively |
| Marsupialization | 75%/3 | High |
| Marsupialization + Peripheral Ostectomy | 25%/1 | Low |
Table 2
Chart 1
Discussion and Conclusion
What we have discussed in this research and the results revealed that the treatment of OKC is controversial. Treatments are generally classified as conservative and aggressive. Odontogenic keratocytes is one of the studied cysts in oral pathology due to its aggressive behavior, high recurrence and histopathological characteristics. It is one of the most common odontogenic cystic lesions (approximately 10-15%). (27) Histologically, when they arise from remnants of the dental lamina and are not associated with teeth, they can be of primary origin (60% of cases) and in 40% of cases it is of dentigerous origin, arising from a reduced enamel organ and it is associated with the remaining teeth. (38) Most OKC reported in the literature show a male preference of 1:1.6. (23,38) They can appear at any age, but most often appear in the third decade of life. They generally involve the posterior region of the mandible at the level of the third molar (27,29,24,23). Conservative treatment generally includes simple enucleation, with or without curettage, using spoon curettage and marsupialization therapy, aggressive treatment generally includes circumferential sitcom, chemical curettage with Carno solution, and resection. Some surgeons believe that the cyst can be properly treated by enucleation if the intact lesion is removed. However, complete removal of OKC can be difficult due to thin and fragile epithelium, limited access to surgery, surgeon's skill and experience, perforation of the cortex, and the desire to preserve adjacent vital structures are the goals of treatment but in eliminating the possibility of recurrence. At the same time, there is no consensus on minimizing surgical complications. (6) Recurrence occurs for the following reasons. The first reason includes the incomplete removal of the epithelial lining of the cyst. Second, it involves the growth of a new OKC from the remaining odontogenic epithelial satellite cysts. A third reason for incomplete surgical treatment involves the development of an unrelated OKC in an adjacent area of the jaws, which is interpreted as a recurrence. Marks and Stern believe that two common reasons for recurrence are incomplete removal of the primary cyst and the formation of a new cyst. (6) Most cases of recurrence occur in the first 5 years after treatment. Due to the problematic nature of these cysts, many attempts have been made to reduce them. High recurrence rates have been improved with surgical techniques. Bramley suggests the use of radical surgery with bone removal and grafting. Decompression or marsupialization appear to be more conservative options in the treatment of OKC. The high recurrence rate associated with OKCs is the result of satellite cysts Cysts confined to the fibrous walls of OKCs It should be emphasized that no satellite cyst will serve as a nucleus for recurrence if the fibrous capsule is completely removed. Due to the possibility of recurrence of cysts caused by the proliferation of basal cells and due to the fragility of the cyst wall and the presence of satellite cysts, the bony walls of the defect are removed with surgical or coarse acrylic burs to ensure the peripheral residual cystic tissue. Enucleation is not always easy because the epithelium may be very thin and fragile, and access deep into the mandible may be limited. Multilocular cysts with specific bony trabeculae are as difficult as removing the epithelium in unilocular. (39) Enucleation by cutting the soft tissue covering OKCs in an attempt to reduce the incidence of its recurrence has been suggested by a number of authors using Carney’s solution (absolute alcohol, chloroform, glacial acetic acid, and iron chloride) are suggested before draining the cysts by removing the covering mucosa in continuity with the lesion. 39) The results of research and investigation showed that the complementary treatment includes marsupialization along with the removal of the surrounding bone. Involved or peripheral ostectomy can be the best treatment solution with the lowest recurrence rate. And patients will be satisfied with the treatment.
References
- MacDonald-Jankowski DS. (2011).
Publisher | Google Scholor - Crispian S. (2008). Oral and maxillofacial medicine: the basis of diagnosis and treatment (2nd ed.). Edinburgh: Churchill Livingstone.
Publisher | Google Scholor - Barnes L, Eveson JW, Reichart P, Sidransky D, eds. (2005). World Health Organization Classification of Tumours: Pathology and Genetics of Head and Neck Tumours World Health Organization Classification of Tumours. Lyon,France: IARC Press.
Publisher | Google Scholor - Madras J, Lapointe H. (2008).
Publisher | Google Scholor - Sharif FN, Oliver R, Suite C, Sharif MO. (2015).
Publisher | Google Scholor - Odell EW, Cawson RA (2017). Cawson's Essentials of Oral Pathology and Oral Medicine (Ninth ed.). Edinburgh.
Publisher | Google Scholor - Philipsen HP, Reichart PA. (2006). Classification of odontogenic tumours. A historical review. J Oral Pathol Med, 35:525‑529.
Publisher | Google Scholor - Borges LB, Fechine FV, Mota MR, Sousa FB, Alves AP. (2012).
Publisher | Google Scholor - Tae GI, Hoe-Kyung H. (2006). Diagnostic ability of differential diagnosis in ameloblatoma and odontogenic keratocyst by imaging modalities and observers. Korean J Oral Maxillofac Radiol, 36:177-82.
Publisher | Google Scholor - Webb JD, Brockbank J. (1984). Treatment of the odontogenic keratocyst by combined enucleation and cryosurgery. Int J Oral Surg, 3:506-510.
Publisher | Google Scholor -
Publisher | Google Scholor - Ren C, Amm HM, DeVilliers P, Wu Y, Deatherage JR, Liu Z, MacDougall M. (2012).
Publisher | Google Scholor - Pogrel MA, Schmidt BL. (2003). The odontogenic keratocyst. Oral Maxillofac Surg Clin North Am, 15:311‑315.
Publisher | Google Scholor - Barnes L, Eveson JW, Reichart P, Sidransky D. (2005). Pathologyand genetics of head and neck tumours. Lyon: IARC Press.
Publisher | Google Scholor - Lo Muzio L, Staibano S, Pannone G, Bucci P, Nocini PF, Bucci E, et al. (1999). Expression of cell cycle and apoptosis‑related proteins in sporadic odontogenic keratocysts and odontogenic keratocystsassociated with the nevoid basal cell carcinoma syndrome. J Dent Res, 78:1345‑1353.
Publisher | Google Scholor - Li TJ. (2011). The odontogenic keratocyst: A cyst, or a cystic neoplasm, J Dent Res, 90:133‑142.
Publisher | Google Scholor - Coulthard P, Heasman PA, Horner K, Sloan P, Theaker ED. (2013). Master dentistry. Volume 1, Oral and maxillofacial surgery, radiology, pathology and oral medicine (Third ed.). Edinburgh.
Publisher | Google Scholor - Ariji Y, Morita M, Katsumata A, Sugita Y, Naitoh M, Goto M, et al. (2011).
Publisher | Google Scholor - Ljubenovi M, Ljubenovi D, Bini I, Jovanovi D, Stanojevi M. (2007). Gorlin-Goltz syndrome. Acta Dermatovenerol Alp Pannonica Adriat, 16(4):166-169.
Publisher | Google Scholor - Ortega García de Amezaga A, García Arregui O, Zepeda Nuño S, Acha Sagredo A, Aguirre Urizar JM. (2008). Gorlin-Goltz syndrome: Clinicopathologic aspects. Med Oral Patol Oral Cir Bucal, 13:E338-E343.
Publisher | Google Scholor - Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, DiGiovanna JJ, et al. (1997). Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet, 69(3):299-308.
Publisher | Google Scholor - Santana N, Yashodha Devi BK, Jatti D. (2011). Gorlin Goltz syndrome– A case report. J Indian Dent Assoc, 5(4):521.
Publisher | Google Scholor - Kahraman D, Gunhan O, Celasun B. (2018). A series of 240 odontogenic keratocysts: Should we continue to use the terminology of ‘keratocystic odontogenic tumour’ for the solid variant of odontogenic keratocyst, J Craniomaxillofac Surg, 46(6):942-946.
Publisher | Google Scholor - Kebede B, Dejene D, Teka A, Girma B, Aguirre EP, Guerra NEP. (2016). Big Keratocystic Odontogenic Tumor of the Mandible: A Case Report. Ethiop J Health Sci, 26(5):491-496.
Publisher | Google Scholor - Kodali R, Guttikondaleela N, Chintada K. (2014). Conservative Management of a Massive Keratocystic Odontogenic Tumour of Mandible: A Case Report and Review. J Res Adv Dent, 1:960-101.
Publisher | Google Scholor - Bello IO. (2016). Keratocystic odontogenic tumor: A biopsy service’s experience with 104 solitary, multiple and recurrent lesions. Med Oral Patol Oral Cir Bucal, 21(5):538-546.
Publisher | Google Scholor - Pazdera J, Kolar Z, Zboril V, Tvrdy P, Pink R. (2014). Odontogenic keratocysts/ keratocystic odontogenic tumours: biological characteristics, clinical manifestation and treatment. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 158(2):170-174.
Publisher | Google Scholor - Thompson LD. (2006). Goldblum JR (ed.). Head and Neck Pathology. Foundations in Diagnostic Pathology. Churchill Livingstone.
Publisher | Google Scholor - Philipsen HP. (2006). Keratocystic odontogenic tumour. In: Barnes L, Evenson JW, Reichart P, Sidransky D. Pathology and genetics of head and neck tumours. Lyon: IARC Press, 306-307.
Publisher | Google Scholor - Deyhimi P, Hashemzadeh Z. (2014). Study of the biologic behavior of odontogenic keratocyst and orthokeratinaized odontogenic cyst using TGF-alpha and P53 markers. Pathol Res Pract, 210(4):201-214.
Publisher | Google Scholor - Wright JM, Vered M. (2017). Update from the 4th edition of the World Health Organization classification of head and neck tumours: Odontogenic and maxillofacial bone tumors. Head Neck Pathol, 11(1):68-77.
Publisher | Google Scholor - Menon S. (2015). Keratocystic Odontogenic Tumours: Etiology, Pathogenesi and Treatment Revisited. J Maxillofac Oral Surg, 14(3):541-547.
Publisher | Google Scholor - de Molon RS, Verzola MH, Pires LC, Mascarenhas VI, da Silva RB, Cirelli JA, et al. (2015). Five years follow-up of a keratocyst odontogenic tumor treated by marsupialization and enucleation: A case report and literature review. Contemp Clin Dent, 6(1):106-110.
Publisher | Google Scholor - Schmidt BL, Pogrel MA. (2001).
Publisher | Google Scholor - de Castro MS, Caixeta CA, de Carli ML, Ribeiro Júnior NV, Miyazawa M, Pereira AA, et al. (2018).
Publisher | Google Scholor - Ledderhof NJ, Caminiti MF, Bradley G, Lam DK. (2017).
Publisher | Google Scholor - Piloni MJ, Keszler A, Itoiz ME. (2005).
Publisher | Google Scholor - Alchalabi NJ, Merza AM, Issa SA. (2017). Using Carnoy’s Solution in Treatment of Keratocystic Odontogenic Tumor. Ann Maxillofac Surg, 7(1):51-56.
Publisher | Google Scholor - Anwar BB, Mansour AA. (1998). Treatment of mandibular odontogenic keratocysts. OOOE, 86:42-7.
Publisher | Google Scholor