Case Report
Clinical, Radiographical and Histological Evaluation of An Immature Permanent Molar with Pulp Necrosis after Revascularization/ Regeneration Procedures-Aase Report
- Marcela Adriana Moya 2
- Gisela Soledad Gualdoni 1
- Ingrid Clarisa Guitelman 2
- Lorena Cabirta 3
- Pablo Rodriguez 3
- Ana Biondi 2
- Romina De Lucca 1
- Cornelis H Pameijer 5*
- Osvaldo Zmener 4
1Department of Histology and Embryology, Faculty of Dentistry, University of Buenos Aires, Argentina.
2Department of Pediatric Dentistry, Faculty of Dentistry, University of Buenos Aires, Argentina.
3Department of Endodontics, Faculty of Dentistry, University of Buenos Aires, Argentina.
4Department of Specialized Endodontics, Faculty of Medical Sciences, Schooled Dentistry, University of El Salvador, Buenos Aires, Argentina.
5Department of Reconstructive Sciences, University of Connecticut, School of Dental Medicine, Farmington, Connecticut,
*Corresponding Author: Cornelis H. Pameijer,Department of Histology and Embryology, Faculty of Dentistry, University of Buenos Aires, Argentina.
Citation: Marcela A. Moya, Gisela S. Gualdoni, Ingrid C. Guitelman, Cabirta L, Cornelis H Pameijer, et al. (2024). Clinical, radiographical and histological evaluation of an immature permanent molar with pulp necrosis after revascularization/regeneration procedures: Case report. Dentistry and Oral Health Care, Biores Scientia Publishers. 2(2):1-9. DOI: 10.59657/2993-0863.brs.24.027
Copyright: © 2024 Cornelis H. Pameijer, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 09, 2024 | Accepted: January 31, 2024 | Published: February 08, 2024
Abstract
Revascularization/regeneration procedures (REPs) in human immature permanent teeth with pulp necrosis have been shown to be a clinical challenge. The aim of this case report was to examine clinically, radiographically and histologically the outcome of REPs in an immature permanent molar with pulp necrosis. An immature permanent mandibular first molar with pulp necrosis in a 9-yr old girl was treated with REPs. At the 3-month follow-up visit the tooth was asymptomatic and functional. Radiographic examination showed that the thickness of the root structure and the root length had slightly increased. After 13 months the tooth fractured and was deemed non-restorable. The tooth was extracted and processed for histological evaluation. Microscopic observation revealed that the root canals were filled with loose fibrous connective tissue resembling periodontal tissue containing many spindle- shaped cells and newly-formed vessels. In the mesiobuccal canal, a mineralized tissue bridge lined by flattened cells was observed at the level of the coronal third. Nerve regeneration was visualized by a silver nitrate impregnation technique. A calcified structure containing irregular spaces filled with fibrous connective tissue was found at the level of the mid root of the distal canal. No calcified tissues were observed at the level of the open apices. The newly formed tissues inside the canals resembled a vascularized periodontal-like fibrous tissue and a cementum-like tissue which are comparable to the histologic findings of previous animal and human case reports.
Significance
This case report suggests that although the newly formed ingrown tissues in the root canals were not true pulp tissues, the tooth treated by regenerative Endodontics regained its vitality and function while also reestablishing its sensory function.
Keywords: immature permanent tooth; pulp necrosis; regenerative endodontics; reinnervation; scaffold
Introduction
Endodontic treatment of immature permanent teeth with pulp necrosis is a clinical challenge since the root canal walls are thinner and prone to fracture during instrumentation, while the apical third has a divergent configuration that complicates root canal obturation procedures [1]. Preservation of the pulp’s vitality is of primary importance for a tooth to be healthy and durable. For this reason, there is a need for a clinical strategy that promotes regeneration of the pulp-dentin complex when these tissues have been lost. Revascularization/regeneration procedures (REPs) is an endodontic alternative to conventional apexification treatment that led to maturogenesis of necrotic immature teeth, with an increase in thickness of the root canal walls and a continuation of root development [2,3]. REPs are recognized as an effective method to treat necrotic immature permanent teeth with or without apical lesions [4,5]. Although this treatment has been successfully used for immature teeth [6-8], there is some evidence that it is also effective in adult teeth with mature apices [9-11]. As defined by the American Association of Endodontists [12], REPs intend to replace damaged tooth structures as well as cells of the pulp-dentin complex by the formation of new vascularized tissues within the root canal space. Further reinnervation may also occur, which is an observation that has been reported by several investigators [13-15]. Although histologic studies have shown that the newly formed tissues did not totally resemble the original pulp-dentin anatomy, teeth treated by REPs can regain vitality, immunology and functionality [16]. In spite of these favorable observations, it has been reported that periapical healing may not occur in a high percentage of cases or may occur without pulp tissue regeneration in the root canal [17-20]. The purpose of this report is to describe clinically, radiographically and histologically a case of a human immature permanent mandibular molar with pulp necrosis that has been treated by revascularization/regeneration procedures.
Case report
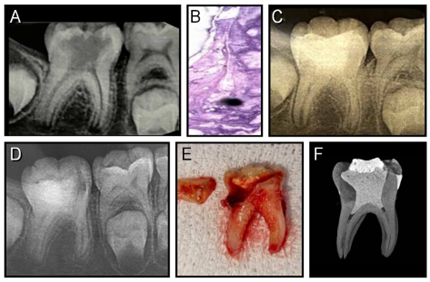
A 9- year-old white female with a non-contributory medical history was referred for evaluation and treatment of her right mandibular first molar. Clinical examination revealed the presence of a deep carious lesion. The tooth was asymptomatic. Periodontal probing and tooth mobility were within normal limits and the tooth was neither tender to percussion nor palpation. Radiographic examination showed roots with immature open apices, thin dentinal walls and no evidence of periapical pathology (Fig.1). Vitality tests were negative while the adjacent teeth responded normally without lingering. From the combined clinical and radiographic examinations, a diagnosis of pulp necrosis was arrived at. Based on the incomplete formation of the roots, REPs were recommended with particular emphasis on the importance of rendering treatment that promoted continued root development. After the risks and benefits of the treatment were explained, the parent of the patient signed an informed consent form.
Figure 1A: Periapical preoperative radiograph of the mandibular right first molar showing an extensive carious lesion.
B: Histologic section of the necrotic tissue removed from the root canals. H&E stain; Original magnification x100.
C: Periapical postoperative radiograph obtained 3 months after REPs.
D: Periapical postoperative radiograph obtained 13 months after REPs. No periapical lesion is present.
E: Photograph of the extracted molar showing a transvers oblique fracture and the fractured coronal piece.
F: Microtomographic picture of the extracted molar. Note the level of the BD plug in the Di and Mb canals.
Treatment procedure
Mandibular block was established with 1.7 mL of 4% Articaine 1:100.000 L-adrenaline (Sidus SA, Buenos Aires, Argentina) and the tooth isolated with rubber dam. After the decay was removed a large pulp exposure was detected. Under copious irrigation with saline, the access cavity was completed, and three canals (one distal and two mesial canals) were identified. The content of the canals was removed with manually operated K-files (Dentsply/Maillefer, Ballaigues, Switzerland) and immediately fixed in 10% neutral buffered formalin. The canals were instrumented manually with K-files (Dentsply/Maillefer) taking care as to not to disturb the weakened dentinal walls. The canals were then irrigated and disinfected for 5 min with1.5% NaOCl followed by 17
Results
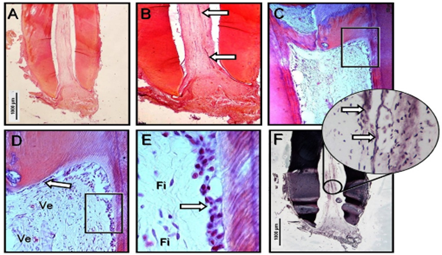
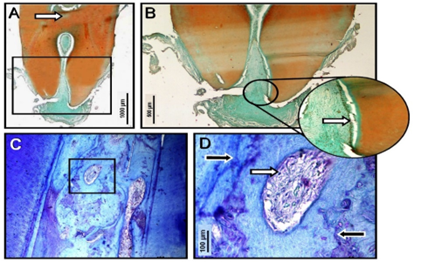
Due to technical problems the mesiolingual canal was lost during histological preparation. The tissue removed from the canals was necrotic which confirmed the clinical diagnosis. The histologic sections of the mesiobuccal (Mb) root were significant for the presence of loose fibrous connective tissue which upon careful analysis resembled periapical tissues that had grown inside the canal up to the BD plug (Fig.2). This tissue was remarkable for spindle-shaped fibroblast-like cells, blood vessels and abundant collagen extracellular matrix. At the level of the BD plug, AR-stained sections showed structures resembling a cementum-like tissue bridge lined with flattened cells that were connected with the dentin walls and gradually changed to dentin-like tissue. Thin black filament structures that were interpreted as nerve fibers were observed in most of the SNi stained sections. In the distal root (Di) a loose periodontal-like tissue without inflammatory cells was also observed in the apical portion (Fig.3). At mid third level, the canal contained newly formed cementum-like structures with different fused areas of calciotraumatic lines and irregular spaces filled with fibrous connective tissue. In both the Mb and Di roots, no calcified tissue was observed at the level of the open apices.
Figure 2A: Photomicrograph of the extracted MB root of revascularized/regenerated tooth. H&E stain; original magnification x20; Bar 1000 µm. The white space is a shrinkage artifact.
B: Detailed view of the apical portion in A. The root canal is filled with newly formed fibrous connective tissue ingrowth. Note the presence of newly formed blood vessels (arrows). H&E stain; original magnification x40.
C: Detailed view of the mid portion of the root showing a mineralized tissue bridge formation resembling cementum tissue lined by flattened cells in direct contact with the dentinal walls. H&E stain; original magnification x100.
D: High magnification of the square area in C. Note that the cementum-like bridge tissue lined by flattened cells (arrow) gradually changed to dentin tissue and that the flattened cells gradually changed to odontoblast cells. Ve: Blood vessels. H&E stain; original magnification x400.
E: High magnification of the square area in D. Note the presence of spindle-shaped fibroblasts (Fi) and odontoblast cells lining the dentinal walls (arrow).
F: Microphotograph of the same MB root stained by silver nitrate impregnation. Original magnification x20; Bar 1000 µm. The inset shows a detail of the area indicated by the circle. Note the presence of nerve fibers (arrows).
Figure3A: Photomicrograph of the extracted Di root of a revascularized/regenerated tooth. White arrow indicates a superposed root structure. Alizarin red stain; original magnification x20; Bar 1000 µm.
B: Detailed view of the square area in A. In the apical third the root canal was filled by a fibrous periodontal-like tissue ingrowth. Alizarin red stain; original magnification x40. Bar 500 µm. The inset shows a high magnification of the area indicated by the circle. At the level of the apical opening, the root canal walls are lined with cementoblasts-like cells. Alizarin red stain; original magnification x400.
C: At the mid portion of the root, the canal was totally filled with a mineralized cementum-like tissue connected to the dentinal walls. Note the presence of different fused hard tissue areas and spaces filled with fibrous tissue. Toluidine blue stain; original magnification x400.
D: Higher magnification from the square area in C showing a space filled by a dense fibrous connective tissue (white arrow). The presence of numerous calciotraumatic lines (black arrows) can be seen. Toluidine blue stain; original magnification x800; Bar 100 µm.
Discussion
The treatment of immature permanent teeth with pulp necrosis has always been an endodontic challenge [18,19]. However, there are many studies reporting a good prognosis after REPs treatment [2-4,6,8]. For REPs, two different clinical procedures have been proposed: The cell transplantation and the cell homing techniques [9,21,22]. In the present case, a cell homing approach was used through the induction of a blood clot after producing bleeding from periapical tissues. According with previous reports [23,24], the blood clot acting as a scaffold plays one of the most important roles in the formation of new tissues in the canal space after REPs in immature necrotic permanent human teeth. Hargreaves et al [23]. and Lovelace et al. [24] suggested that in comparison to blood from the peripheral circulation, blood that originates from periapical tissues contains a high concentration of mesenchymal stem cells markers, platelet-derived growth factors and signaling molecules that are capable of promoting stem cell proliferation and differentiation. In addition to the blood clot, an effective irrigation/disinfection protocol and a plug material that is biocompatible are crucial when using REPs. Furthermore, an adequate coronal seal is mandatory to allow for the survival of stem cells that are needed for generation of new tissues. In this particular case, 1,5% NaOCl and 17
Conclusion
Based on the clinical, radiographic and histologic observations of the case presented here suggest that REPs can be recommended for the treatment of immature permanent teeth with pulp necrosis, especially since recuperation of the sensory functions appears to be possible. However, since this is a single case report with a relatively short follow-up period of 13 months, long-term randomized clinical trials with an adequate number of samples should be conducted before definitive conclusions can be reached. Given the nature of the problem this is a tall task.
Conflict of interest
There is no conflict of interest related to this case report.
References
- Wigler R. Kaufman AY, Lin S et al. (2013). Revascularization: a treatment for permanent teeth with necrotic pulp and incomplete root development. J Endod, 39:319-326.
Publisher | Google Scholor - Awies A, Ghoniem A, El-Baz A. (2017). Comparative study between revascularization (Regeneration) and MTA apexification for necrotic immature permanent anterior teeth with open apex: A randomized controlled trial. Int Adv Res, 5:903-912.
Publisher | Google Scholor - Jadhav G, Shah N, Logani A. (2012). Revascularization with and without platelet-rich plasma in non-vital immature, anterior teeth: A pilot clinical study. J Endod, 38:1581-1587.
Publisher | Google Scholor - Iwaya SL, Ikawa M, Kubota M. (2001). Revascularization of an immature permanent tooth with apical Periodontitis and sinus tract. Dent Traumatol, 17:185-187.
Publisher | Google Scholor - Kim SG, Malek M, Sigurdsson A et al. (2018) Regenerative endodontics: a comprehensive review. Int Endod J, 51:1367-1388.
Publisher | Google Scholor - Ding RY, Cheung GS, Chen J et al. (2009). Pulp revascularization of immature teeth with apical periodontitis: A clinical study. J Endod, 35:745-749.
Publisher | Google Scholor - Li L, Pan Y, Mei L, Li J. (2017). Clinical and radiographic outcomes in Immature permanent necrotic evaginated teeth treated with regenerative endodontic procedures. J Endod, 43:246-251.
Publisher | Google Scholor - Shimizu E, Jong G, Patridge N, et al. (2012). Histologic observation of a Human immature permanent tooth with irreversible pulpitis after revascularization/regeneration procedure. J Endod; 38:1293-1297.
Publisher | Google Scholor - Yan H, De Deus G, Kristoffersen IM et al. (2023). Regenerative Endodontics by cell homing: a review of recent clinical trials. J Endod, 49: 4-17.
Publisher | Google Scholor - Garrido-Parada S, Castelo-Bag P, Feijoo-Pato N et al. (2022) Endodontic regenerative procedures in necrotic adult teeth. Appl Sci; 12: 4212.
Publisher | Google Scholor - Paryam K, Kim SG. (2013). Regenerative endodontic treatment of permanent teeth after completion of root development: a report of 2 cases. J Endod, 39:929-934.
Publisher | Google Scholor - AAE. AAE Clinical considerations for a regenerative procedure. Revised 2028. Available (accessed on 14 august 2023).
Publisher | Google Scholor - Wei Y, Lyu P. Bi R et al. (2022). Neural regeneration in regenerative endodontic treatment: An overview and current trends. Int J Mol Sci, 2315492.
Publisher | Google Scholor - Austah O, Joon R, Fath WM et al. (2018). Comprehensive characterization of 2 immature teeth treated with regenerative endodontic procedures. J Endo, 44:1802-1811.
Publisher | Google Scholor - Schmalz G, Widbiller M, Galler KM. (2020). Clinical perspectives of pulp regeneration. J Endod, 46:S161-S174.
Publisher | Google Scholor - Lin LM, Huang GT-J, Sigurdsson A et al. (2021). Clinical cell-based versus cell-free regenerative endodontics: Clarification of concept and term. Int Endod J, 54:887-901.
Publisher | Google Scholor - Wikström A, Brudin M, Vestman NR et al. (2022). Endodontic pulp revitalization in traumatized necrotic immature permanent incisors: Early failures and long-term outcomes-A longitudinal cohort study. Int Endod J, 55: 630-645
Publisher | Google Scholor - Lee C, Song M. (2022). Failure of regenerative endodontic procedures: Case analysis and subsequent treatment options.J Endod, 48:1137-1145.
Publisher | Google Scholor - Nostrat A, Homayounfar N, Oloomi K. (2012). Drawbacks and unfavorable outcomes of regenerative endodontic treatments of necrotic immature teeth: a literature review and report of a case. J Endod, 38:1428-1434
Publisher | Google Scholor - Nostrat A, Li KL, Vir K et al. (2013). Is pulp regeneration necessary for root maturation? J Endo, 39:1291-1295.
Publisher | Google Scholor - Sui B, Chen C, Kou X et al. (2019). Pulp stem cell-mediated functional pulp regeneration. J Dent Res, 98:27-35.
Publisher | Google Scholor - Tirez E, Pedano MS. (2022). Regeneration of the pulp tissue: Cell homing versus cell transplantation approach: A systematic review. Materials (Basel), 15:8603.
Publisher | Google Scholor - Hargreaves KM, Geisler T, Henry MA et al. (2008). Regeneration potential of the young permanent tooth: what does the future hold? J Endod, 34:S51-56.
Publisher | Google Scholor - Lovelace TW, Henry MA, Hargreaves KM et al. (2011). Evaluation of the delivery teeth after clinical regenerative endodontic procedures. J Endod,; 37:133-138.
Publisher | Google Scholor - Trevino EG, Patwardhan AN, Henry MA et al. (2011). Effects of irrigants on the survival of human stem cells on the apical papilla in a platelet-rich plasma scaffold in human root tips. J Endod; 37:1109-1115.
Publisher | Google Scholor - El Ashry SH, Abu-Seida AM, Bayoumi AA et al. (2016). Regenerative potential of immature permanent non-vital teeth following different dentin surface treatments. Exp Toxicol Pathol; 68:181-190.
Publisher | Google Scholor - Galler K, D´Souza R, Federlin M. (2011.) Dentine conditioning codetermined cell fate in regenerative endodontics. J Endod,37:1536-1541.
Publisher | Google Scholor - Mori GG, Teixeira LM, de Oliveira DL, et al. (2014). Biocompatibility evaluation of Biodentine in subcutaneous tissue of rats. J Endod, 40:1485-1488.
Publisher | Google Scholor - Ranjan M. (2014). Review on Biodentine – a bioactive dentin substitute. J Dent Med Sci, 13:13-17.
Publisher | Google Scholor - Laurent P, Camps J, About I. (2012). BiodentineTM induces TGF-ẞ1 release from human pulp cells and early dental pulp mineralization. Int Endod J, 45:439-448.
Publisher | Google Scholor - Grech L, Mallia B, Camilleri J. (2013) Investigation of the physical properties of tricalcium silicate cement-based root-end filling materials. Dent Mater, 29:20-28.
Publisher | Google Scholor - Rajasekharan S, Martens LC, Cauwels RGEC et al. (2014). BiodentineTM material characteristics and clinical applications: a review of the literature. Eur Arch Paediatr Dent; 15:147-158
Publisher | Google Scholor - Wang X, Thibodeau B, Trope M et al. (2010). Histologic characterization of regenerated tissues in canal space after the revitalization/revascularization procedure of immature dog teeth with apical periodontitis. J Endod, 36:56-63.
Publisher | Google Scholor - Nostrat A, Kolahdouzan A, Hossein F. et al. (2015) Histologic outcomes of uninfected human immature teeth treated with regenerative Endodontics: 2 case reports. J Endod, 41:1725-1729.
Publisher | Google Scholor - Sonoyama W, Liu Y, Yamaza T et al. (2008). Characterization of the apical papilla and its residing cells from human immature permanent teeth: a pilot study. J Endod; 34: 166-171.
Publisher | Google Scholor - Tziafas D, Kodonas K. (2010). Differentiation potential of dental papilla, dental pulp and apical papilla progenitor cells. J Endod; 36:781-789.
Publisher | Google Scholor