Research article
Clinical and Immunological Pattern of Systemic Lupus Erythematosus in Men: Cohort Retrospective Study
- Khamrunissa Hussain Sheikh 1
- Israa Musaddif Salman 2
- Nouf Abdulrahman Alghofaili 2*
- Rotan Abdulrahman Baothman 2
1Department of Family and Community Medicine, College of Medicine, Ibn Sina National College, Jeddah, Saudi Arabia.
2Interns, College of Medicine, Ibn Sina National College, Jeddah, Saudi Arabia
*Corresponding Author: Nouf Abdulrahman Alghofaili,Interns, College of Medicine, Ibn Sina National College, Jeddah, Saudi Arabia
Citation: Khamrunissa H. Sheikh, Israa M. Salman, Nouf A. Alghofaili, Rotan A. Baothman. (2023). Clinical and Immunological Pattern of Systemic Lupus Erythematosus in Men: Cohort Retrospective Study. Journal of Clinical Rheumatology and Arthritis, BRS Publishers. 1(1); DOI: 10.59657/jcra.brs.23.003
Copyright: © 2023 Nouf Abdulrahman Alghofaili, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 01, 2023 | Accepted: June 15, 2023 | Published: June 19, 2023
Abstract
Background: Systemic lupus erythematous (SLE) is an autoimmune inflammatory rheumatic disease with multisystemic involvement, it is chronic, systemic, and multisystemic. An individual who is affected by this disease experiences tissue-binding antibodies and immune complexes that cause damage to their organs and cells. The prevalence of neuropsychiatric and renal illnesses in men was greater than in women, as were the rates of peripheral vascular disease, myocardial infarction, and disability.
Objective: This study aimed to improve the understanding of SLE patients by characterizing the different sexes of SLE patients in the inception in male and various clinical manifestations of the disease, disease severity and immunological results and to recognize the different pattern of the disease between male and female patient.
Methods: A retrospective cohort study was conducted among Systemic Lupus Erythematous adult patients from 2020 to 2022 in King Fahad Armed Forces Hospital Jeddah, Ministry of Defense and Aviation (MODA). Data was collected from medical records. Patterns of diseases, clinical manifestations, disease severity and immunological lab results were compared through the mentioned database. Then data was entered and analyzed using SPSS version 23.0.
Results: About 114 of the participants enrolled in the current study. 92 (80.7%) of the participants were females and the rest 22 (19.3%) were males. The mean age was 41.5 with standard deviation of 13.6 (41.5 ± 13.6) and range of (15 - 81) years old. The mean age at time of the diagnosis was 33.3 ± 13.1 (10 - 81) years old. Time between onset of the disease and diagnosis was more than 3 months in 79 (69.3%) of the participants and less than 3 months in 35 (30.7%) of the participants. The most frequently reported co-morbidity was found to be hypertension in (20.2%) of the participants. Hypothyroidism in (14.9%) of the participants, diabetes mellitus in (12.3%) of the participants. Fever and weight loss were not found to be significantly associated with gender (p-value= 0.926 and 0.518 respectively). No statistically significant association found between the following; non-sacaring alopecia, oral ulcers, malar rash, discoid rash, Raynaud phenomenon, photosensitivity and gender (p-value= 0.053, 0.190, 0.254, 0.560, 0.684 and 0.744 respectively). Lupus nephritis was found to be significantly associated with gender (p-value= 0.008) with males tend to develop lupus nephritis more frequently than females. Delirium, psychosis and seizure were not found to be significantly associated with gender. +ve Anti Ro (SSA) was found to be significantly associated with gender (p-value= 0.004) with females having tested positive for anti-Ro (SSA) antibodies more frequently than males. The most common medication used was found to be hydroxychloroquine as reported in 109 (95.6%) of the participants followed by corticosteroids in 75 (65.8%) of the participants.
Conclusion: Lupus nephritis was found to be more frequently reported in males compared to females. Hypertension was the most frequent co-morbidy in patients with SLE. Hydroxychloroquine is the drug of choice which used by the vast majority of respondents.
Keywords: clinical; immunological pattern; systemic lupus erythematous sle in men
Introduction
Systemic lupus erythematosus (SLE) is a chronic autoimmune rheumatic disease that can lead to multiple systemic manifestations. It is serologically characterized by autoantibodies that target self-antigens and result in tissue-binding autoantibodies and immune complexes that can damage organs and cells of affected individuals.
SLE has different clinical presentations between men and women. Men tend to be diagnosed at an older age and have a lower education level. Moreover, they are more likely to experience end-organ damage, such as neuropsychiatric, renal, cardiovascular, peripheral vascular disease, and myocardial infarction. Additionally, men are three times more likely than women to experience other disabilities and lupus nephritis. Although SLE is a women-predominant disease, it is also found in men. However, several studies have revealed no significant differences in clinical and laboratory findings between men and women, except for a higher frequency of renal disease and serositis in men.
In this retrospective study, we conducted a comprehensive analysis of the disease patterns, initial symptoms, clinical manifestations, disease severity, and immunological results in male patients with SLE. The primary objective of this research was to enhance our understanding of SLE by characterizing the differences in clinical outcomes, disease severity, and immunological results between male and female patients with SLE. By identifying and comparing these patterns, we aimed to recognize and establish the distinct disease manifestations in men and women.
Summary
We are comparing clinical manifestation and immunological features through diagnosed SLE patient male and female who are actively following up in rheumatology clinic in our institution.
Methods
Study Design and Population
A retrospective cohort study was conducted among adult patients with SLE from 2020 to 2022 at King Fahad Armed Forces Hospital (KFAFH) in Jeddah, which is under the jurisdiction of the Ministry of Defence and Aviation (MODA). The study involved retrospective analysis of medical record data for 22 male and 97 female patients attending the Rheumatology clinic at KFAFH. The study compared disease patterns, clinical manifestations, disease severity, and immunological laboratory data for male and female adults diagnosed actively following up at the Rheumatology clinic in KFAFH and diagnoses with SLE. The data was collected using a standardized collection sheet from medical records and the electronic OASIS system. The study excluded paediatric age groups and adults who were not diagnosed with SLE. The attached Excel sheet summarizes the details of the collected data.
To protect the personal data of each patient, a registry code was assigned to them in the database. In dealing with missing data, a common default used in statistical software is to exclude study subjects who have incomplete data for any variable of interest from the analysis. However, traditional methods for addressing missing data involve imputing (filling in) the missing values with single estimates of the respective value. These methods may include using the mean value of the observed values, estimating the value from a regression model, or using observed values from a similar subject.
Results
Demographic characteristics
This study enrolled a total of 114 participants, of which 92 (80.7%) were women and 22 (19.3%) were men. The participants had a mean age of 41.5 years with a standard deviation of 13.6 (41.5±13.6) and a range of 15 to 81 years old. The majority of participants (94, 82.5%) were from the Middle Eastern region, while 14 (12.3%) were Asian, five (4.4%) were White, and one (0.9%) was Black or African American. The mean age at the time of diagnosis was 33.3 ± 13.1 (10–81) years old. The duration between disease onset and diagnosis was greater than 3 months in 79 (69.3%) participants and less than 3 months in 35 (30.7%) participants.
Table 1: Socio-demographic data of the study participants (n=114).
| Variable | Overall n (%) |
| Gender: | |
| Male | 22 (19.3) |
| Female | 92 (80.7) |
| Age (in year): mean ± SD (Range) | 41.5 ± 13.6 (15 – 81) |
| Race: | |
| Asian | 14 (12.3) |
| Black or African American. | 1 (0.9) |
| Middle eastern | 94 (82.5) |
| White | 5 (4.4) |
| Age at time of the diagnosis (in year): mean ± SD (Range) | 33.3 ± 13.1 (10 – 81) |
| Time of the onset till diagnosis: | |
| Less than 3 months | 35 (30.7) |
| More than 3 months | 79 (69.3) |
Comorbidities
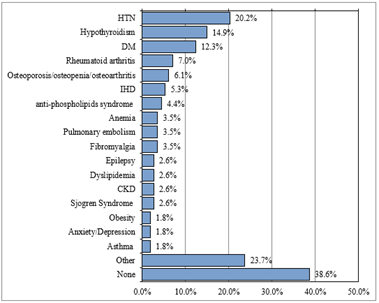
Hypertension was the most frequently reported comorbidity affecting 20.2% of the participants. Hypothyroidism was present in 14.9%, while 12.3% had diabetes mellitus. Rheumatoid arthritis was reported in 7.0% of the participants, and osteoporosis, osteopenia, and osteoarthritis were found in 6.1%. Ischemic heart disease (IHD) was present in 5.3%, antiphospholipid syndrome in 4.4% of the participants. Anaemia, pulmonary embolism, and fibromyalgia were each represented by 3.5% of the participants, while epilepsy and chronic kidney disease (CKD) were each present in 2.6%. and Sjogren’s syndrome and dyslipidaemia were reported in 2.6% of the participants, and obesity, asthma, and anxiety were each found in 1.8%. Additionally, 23.7% of participants had other comorbidities, while the remaining 38.6% had no comorbidities.
Figure 1:Comorbidities.
Clinical manifestations
With regard to the clinical manifestations of SLE, disease severity, immunological results, and their association with sex, among 114 participants, 32 (28.1%) had fever, and 18 (15.8%) had weight loss. Neither fever nor weight loss were not found to be significantly associated with sex (p=0.926 and p=0.518, respectively). Thirty-five (30.7%) had non-scarring alopecia, 29 (25.4%) had oral ulcers, 26 (22.8%) had malar rash, 22 (19.3%) had discoid rash, 10 (8.8%) had Raynaud’s phenomenon, and 13 (11.4%) had photosensitivity. No statistically significant association was found between non-scarring alopecia, oral ulcers, malar rash, discoid rash, Raynaud’s phenomenon, photosensitivity, and sex (p=0.053, p=0.190, p=0.254, p=0.560, p=0.684 and p=0.744, respectively). Arthritis was reported in 83 (72.8%) of the participants, with small joint arthritis found in 32 (38.6%), large joint arthritis in 25 (31.1%), and both small and large joints in 26 (31.3%) of the participants. No sex difference was observed regarding the development of arthritis and joint locations and count (p=0.108 and p=0.390, respectively). Regarding the serositis domain, pleural or pericardial effusion were found in 19 (16.6%) of the participants, and pericarditis was found in nine (7.9%) of the participants. Neither pleural nor pericardial effusions were significantly associated with sex (p=0.052 and p=0.688, respectively). Lupus nephritis was found in 27 (23.7%) of the participants, with males tending to develop this condition more frequently than women (p=0.008). Delirium was found in two (1.8%) of the participants, psychosis in five (4.4%), and seizure in nine (7.0%) of the participants. Delirium, psychosis, and seizure were not significantly associated with sex. Leukopenia was noted in 37 (32.5%) of the participants, lymphopenia was found in 45 (39.5%), thrombocytopenia was found in 19 (16.7%), autoimmune hemolysis was found in (43%), and vascular thrombosis was found in 16 (14%) of the participants. No difference in sex was observed for leukopenia, lymphopenia, thrombocytopenia, autoimmune hemolysis, and vascular thrombosis (p=0.963, p=0.107, p=0.199, p=0.230, and p=0.302, respectively). Twenty-nine (29.3%) of the participants tested positive for anti-Ro (SSA). Positive anti Ro (SSA) was significantly associated with sex (p=0.004), with female patients testing positive for anti-Ro (SSA) antibodies more frequently than male patients.
Table 2: Clinical manifestations of the disease, disease severity and immunological results and its association with gender.
| Variable | Overall (n=114) | Gender | P value | |
| Male (n=22) | Female (n=92) | |||
| n (%) | n (%) | |||
| Constitutional domain: | ||||
| Fever | 32 (28.1) | 6 (27.3) | 26 (28.3) | 0.926 |
| Weight loss | 18 (15.8) | 2 (9.1) | 16 (17.4) | 0.518F |
| Cutaneous domain: | ||||
| Non-scarring alopecia | 35 (30.7) | 3 (13.6) | 32 (34.8) | 0.053 |
| Oral ulcer | 29 (25.4) | 8 (36.4) | 21 (22.8) | 0.190 |
| Malar rash | 26 (22.8) | 3 (13.6) | 23 (25) | 0.254 |
| Discoid rash | 22 (19.3) | 3 (13.6) | 19 (20.7) | 0.560F |
| Raynaud phenomenon | 10 (8.8) | 1 (4.5) | 9 (9.8) | 0.684F |
| Photosensitivity | 13 (11.4) | 2 (9.1) | 11 (12) | 0.744F |
| Arthritis domain: | ||||
| Arthritis | 83 (72.8) | 13 (59.1) | 70 (76.1) | 0.108 |
| Joint location and count: | ||||
| Small joint | 32 (38.6) | 3 (23.1) | 29 (41.4) | 0.390F |
| Large joint | 25 (30.1) | 4 (30.8) | 21 (30) | |
| Small & large joints | 26 (31.3) | 6 (46.2) | 20 (28.6) | |
| Serositis domain: | ||||
| Pleural or pericardial effusion | 19 (16.7) | 7 (31.8) | 12 (13) | 0.052F |
| Pericarditis | 9 (7.9) | 1 (4.5) | 8 (8.7) | 0.688F |
| Renal domain: | ||||
| Lupus nephritis | 27 (23.7) | 10 (45.5) | 17 (18.5) | 0.008* |
| Lupus nephritis class: | ||||
| Class 1 | 1 (3.7) | 0 (0) | 1 (5.9) | 0.099F |
| Class 2 | 4 (14.8) | 0 (0) | 4 (23.5) | |
| Class 3 | 5 (18.5) | 2 (20) | 3 (17.6) | |
| Class 4 | 11 (40.7) | 7 (70) | 4 (23.5) | |
| Class 5 | 6 (22.2) | 1 (10) | 5 (29.4) | |
| Neurologic domain: | ||||
| Delirium | 2 (1.8) | 2 (9.1) | 0 (0) | 0.036F |
| Psychosis | 5 (4.4) | 2 (9.1) | 3 (3.3) | 0.246F |
| Seizure | 9 (7.9) | 4 (18.2) | 5 (5.4) | 0.068F |
| Hematologic domain: | ||||
| Leukopenia | 37 (32.5) | 7 (31.8) | 30 (32.6) | 0.943 |
| Lymphopenia | 45 (39.5) | 12 (54.5) | 33 (35.9) | 0.107 |
| Thrombocytopenia | 19 (16.7) | 6 (27.3) | 13 (14.1) | 0.199F |
| Autoimmune haemolysis (Direct antiglobulin test + ve) (n=100) | 43 (43) | 7 (31.8) | 36 (46.2) | 0.230 |
| Vascular thrombosis | 16 (14) | 5 (22.7) | 11 (12) | 0.302F |
| Immunological manifestation: | ||||
| +ve ANA | 110 (96.5) | 20 (90.9) | 90 (97.8) | 0.167F |
| +ve Anti ds-DNA (n=109) | 69 (63.3) | 14 (63.6) | 55 (63.2) | 0.971 |
| +ve Anti smith (n=98) | 19 (19.4) | 3 (13.6) | 16 (21.1) | 0.551F |
| +ve Anti Ro (SSA) (n=99) | 29 (29.3) | 1 (4.5) | 28 (36.4) | 0004* |
| +ve Anti LA (SSB) (n=99) | 12 (12.1) | 0 (0) | 12 (15.4) | 0.065F |
| +ve Anti cardiolipin (n=93) | 20 (21.5) | 4 (18.2) | 16 (22.5) | 0.774F |
| +ve Anti glycoprotein (n=91) | 16 (17.6) | 3 (13.6) | 13 (18.8) | 0.752F |
| +ve Lupus anticoagulant (n=99) | 24 (24.2) | 8 (364) | 16 (20.8) | 0.133 |
| C3: (n=113) | ||||
| Low | 47 (41.2) | 13 (59.1) | 34 (37.4) | 0.124F |
| Normal | 64 (56.1) | 9 (40.9) | 55 (60.4) | |
| High | 2 (1.8) | 0 (0) | 2 (2.2) | |
| C4: (n=113) | ||||
| Low | 55 (48.2) | 12 (54.5) | 43 (47.3) | 0.767F |
| Normal | 56 (49.1) | 10 (45.5) | 46 (50.5) | |
| High | 2 (1.8) | 0 (0) | 2 (2.2) | |
P-values were calculated using Fisher's exact test (F) and the chi-square test. * Significant p value < 0>
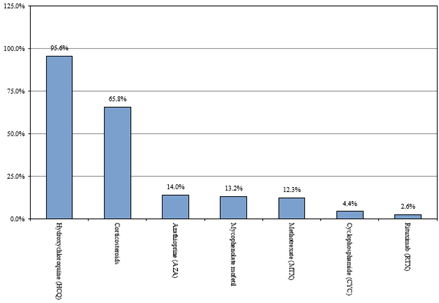
Medication
The most commonly used medication was hydroxychloroquine, reported by 109 (95.6%) of the participants. Corticosteroids were the most commonly utilized medication, reported by 75 (65.8%) of the participants, followed by azathioprine (16 participants, 14%), mycophenolate mofetil (15 participants, 13.2%), methotrexate (14 participants, 12.3%), cyclophosphamide (five participants, 4.4%), and rituximab (three participants, 2.6%).
Figure 2:Medications.
Discussion
Studying the clinical and immunological patterns of SLE in men is crucial for intervening during disease progression. There may be differences in patterns between males and females, and understanding the patterns in each sex is key for developing appropriate intervention that can result in better treatment outcomes [12].
The aim of this study was to improve the comprehension of patients with SLE by characterizing the disease’s various clinical manifestations, disease severity, and immunological results in both male and female patients. This research also aimed to recognize the distinctive patterns of the disease between the two sexes.
The mean age was 41.5 years old. The vast majority (80.7%) of the participants were females, while the remaining 19.3% were males. For over two-thirds of the participants (69.3%), the time between disease onset and diagnosis exceeded three months. The mean age at the time of diagnosis was 33.3 years old, which corresponds to the results of a parallel study conducted by Merola, where the mean age at diagnosis was found to be 35 years [13].
In terms of comorbidities present in patients with SLE, hypertension was the most frequently reported comorbidity, with approximately one-fifth (20.2%) of the participants experiencing it. This was followed by hypothyroidism, which was reported by 14.9% of the participants, diabetes mellitus by 12.3%, rheumatoid arthritis by 7.0%, and osteoporosis, osteopenia, and osteoarthritis by 6.1% of the participants. Similar findings were reported in a study conducted by Gergianaki et al., which found that thyroid disease and hypertension were the most commonly reported comorbidities in patients with SLE [14].
In relation to the clinical manifestations of SLE, disease severity, immunological results, and their association with sex, it was observed that fever and weight loss were not significantly associated with sex, which is in line with the findings of a similar study conducted by Blazickova et al., which reported that all patients experienced constitutional symptoms without any sex difference [15]. Additionally, no statistically significant associations were observed between non-scarring alopecia, oral ulcers, malar rash, discoid rash, Raynaud’s phenomenon, photosensitivity, and sex. However, there was a significant association between positive anti-Ro (SSA) antibodies and sex, with women testing positive for these antibodies more frequently than men. Lupus nephritis was also significantly associated with sex, with men showing a higher frequency of this condition compared to women, and this was consistent with previous studies that reported nephritis as a more common feature of the disease among males [16–18].
With respect to the medications administered to patients with SLE, hydroxychloroquine was the most commonly used medication, as reported by the vast majority (95.6%) of the participants, followed by corticosteroids, which were used by more than two-thirds (65.8%) of the participants. Azathioprine was found to be used by 14% of the participants, mycophenolate mofetil by 13.2%, and methotrexate by 12.3% of the participants. Similar findings were reported in a parallel study conducted by Kariburyo et al., in which the most frequently prescribed drugs for the treatment of SLE were hydroxychloroquine and corticosteroids [19].
Conclusion
The incidence of lupus nephritis was found to be higher in male patients with SLE compared to females. In terms of immunological markers, anti-Ro (SSA) was significantly more prevalent in females than in males. Furthermore, hypertension was identified as the most common comorbidity in patients with SLE. Among the medications used to manage SLE, hydroxychloroquine was the most commonly prescribed drug, according to the majority of respondents. The possibility of lupus nephritis should be carefully considered in male patient with SLE. Timely identification and treatment of this condition could potentially improve patient outcomes. Further research is required to validate the current findings and gain a deeper understanding of the immunological aspects of SLE.
References
- Dey, D. Ofori, E. Hutton-Mensah, K. A. Akutek, M. L. K. Okine, R. Amoaba, I. ... & Kwarko, H. (2019). Clinical characteristics of males with systemic lupus erythematosus (SLE) in an inception cohort of patients in Ghana. Ghana Medical Journal, 53(1):2-7.
Publisher | Google Scholor - Lu, L. J. Wallace, D. J. Ishimori, M. L. Scofield, R. H. & Weisman, M. H. (2010). Male systemic lupus erythematosus: a review of sex disparities in this disease. Lupus, 19(2):119-129.
Publisher | Google Scholor - Ding, Y. He, J. Guo, J. P. Dai, Y. J. Li, C. Feng, M. ... & Li, Z. G. (2012). Gender differences are associated with the clinical features of systemic lupus erythematosus. Chinese medical journal, 125(14):2477-2481.
Publisher | Google Scholor - Font, J. Cervera, R. Navarro, M. Pallares, L. Lopez-Soto, A. Vivancos, J. & Ingelmo, M. (1992). Systemic lupus erythematosus in men: clinical and immunological characteristics. Annals of the rheumatic diseases, 51(9):1050-1052.
Publisher | Google Scholor - Agrawaal, K. K. & Dhakal, S. S. (2014). Systemic lupus erythematosus in males: a case series. Saudi Journal of Kidney Diseases and Transplantation, 25(3), 638.
Publisher | Google Scholor - Faezi, S. T. Hosseini Almodarresi, M. Akbarian, M. Gharibdoost, F. Akhlaghi, M., Jamshidi, A., ... & Davatchi, F. (2014). Clinical and immunological pattern of systemic lupus erythematosus in men in a cohort of 2355 patients. International journal of rheumatic diseases, 17(4):394-399.
Publisher | Google Scholor - Garcia, M. A., Marcos, J. C., Marcos, A. I., Pons-Estel, B. A., Wojdyla, D., Arturi, A., ... & Alarcon-Segovia, D. (2005). Male systemic lupus erythematosus in a Latin-American inception cohort of 1214 patients. Lupus, 14(12):938-946
Publisher | Google Scholor - Aranow, C. Del Guidice, J. Barland, P. & Weinstein, A. (2002). Systemic lupus erythematosus disease severity in men and women: a case-control study. J Rheumatol, 29(8):1674-1677
Publisher | Google Scholor - Gutbi, H. A. Elagib, E. M. Essa, M. E. A. Ahmed, N. I. & Saadelnour, M. A. I. (2022). Pattern and clinical phenotype of systemic lupus erythematosus among male patients: Hospital‐based study. Clinical and Translational Discovery, 2(4):148
Publisher | Google Scholor - Gui, Y. Bai, W. Xu, J. Duan, X. Zhan, F. Zhao, C. ... & Zeng, X. (2022). Sex differences in systemic lupus erythematosus (SLE): an inception cohort of the Chinese SLE Treatment and Research Group (CSTAR) registry XVII. Chinese Medical Journal, 10-1097
Publisher | Google Scholor - Boodhoo, K. D. Liu, S. & Zuo, X. (2016). Impact of sex disparities on the clinical manifestations in patients with systemic lupus erythematosus: a systematic review and meta-analysis. Medicine, 95(29)
Publisher | Google Scholor - do Socorro Teixeira Moreira Almeida M, da Costa Arcoverde J, Barros Jacobino MN, Coimbra Neto AR. (2011). Male systemic lupus erythematosus, an overlooked diagnosis. Clin Pract, 1(4):103.
Publisher | Google Scholor - Merola JF, Bermas B, Lu B, Karlson EW, Massarotti E, Schur PH, Costenbader KH. (2014). Clinical manifestations and survival among adults with (SLE) according to age at diagnosis. Lupus, 23(8):778-784.
Publisher | Google Scholor - Gergianaki I, Garantziotis P, Adamichou C, Saridakis I, Spyrou G. et.al. (2021). High Comorbidity Burden in Patients with SLE: Data from the Community-Based Lupus Registry of Crete. J Clin Med, 10(5):998.
Publisher | Google Scholor - Blažíčková S RJ. (2017). Systemic Lupus Erythematosus Detected in Males in the Population of Slovakia. J Nephrol urol, 1:6.
Publisher | Google Scholor - Juan Liu FY, Sui Dianjing, Guo Qiaoyan, Dong Changqing, Wang Jing. et.al. (2017). Clinical and pathological characteristics of male patients with systemic lupus erythematosus from northeast China: a ten-year retrospective study. Int J Clin Exp Pathol, 10:6082-6091.
Publisher | Google Scholor - Molina JF, Drenkard C, Molina J, et al. (1996). Systemic lupus erythematosus in males. A study of 107 Latin American patients. Medicine (Baltimore), 75:124-130.
Publisher | Google Scholor - Blum A, Rubinow A, Galun E. (1991). Predominance of renal involvement in male patients with systemic lupus erythematosus. Clinical and experimental rheumatology, 9:206-207.
Publisher | Google Scholor - Kariburyo F, Xie L, Sah J, Li N, Lofland JH. (2020). Real-world medication uses and economic outcomes in incident systemic lupus erythematosus patients in the United States. J Med Econ, 23(1):1-9.
Publisher | Google Scholor