Case Report
Circumflex Aortic Artery, A Diagnosis of The DiGeorge Syndrome from An Aortic Malformation in A Prenatal Examination
Faculty of Medicine, Catholic University, Valencia, Spain.
*Corresponding Author: Mar Gimeno Vicente, Faculty of Medicine, Catholic University, Valencia, Spain.
Citation: Mar Gimeno Vicente. (2024). Circumflex Aortic Artery, A Diagnosis of The DiGeorge Syndrome from An Aortic Malformation in A Prenatal Examination, Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(4):1-4. DOI: 10.59657/2993-0871.brs.24.037
Copyright: © 2024 Mar Gimeno Vicente, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 12, 2024 | Accepted: March 02, 2024 | Published: March 25, 2024
Abstract
These abnormalities could be presented isolated or associated to chromosomopathies. The 22q11.2 microdelection, well-known as cause of the DiGeorge syndrome, has been related to aortic arch alterations, such as right aortic arch, subclavian malformations, and aortic arch interruptions. This syndrome affects 1-4 per 6000 alive newborns, and it typically produces problems in the development of the structures of the thoracic midline, facial dysmorphia, T- lymphocytes immunodeficiency, endocrinal disorders. Aortic arch congenital anomalies are a group of malformations caused by an alteration of the aortic and gill arches during the embryogenesis. Their prevalence is close to 2% and their manifestations could be very diverse, from asymptomatic to compression of the thoracic structures, fact that may compromise the respiratory and swallowing function. These abnormalities could be presented isolated or associated to chromosomopathies. The 22q11.2 microdeletion, well-known as cause of the DiGeorge syndrome, has been related to aortic arch alterations, such as right aortic arch, subclavian malformations, and aortic arch interruptions. This syndrome affects 1-4 per 6000 alive newborns, and it typically produces problems in the development of the structures of the thoracic midline, facial dysmorphia, T-lymphocytes immunodeficiency, endocrinal disorders. Left circumflex aortic artery has been associated to this syndrome and it occurs during the third week of gestation due to the regress of the fourth gill arch and the persistence of the sixth, which provoke the development of a left and retroesophagic aortic arch, and a right descending aorta. This alteration of the normal conformation originates a vascular ring around the trachea and the main branches, with the arteriosus ductus located on the right side of the trachea and the pulmonary artery on the anterior part affecting the respiratory function. We expose the case of a patient diagnosed of circumflex aortic artery in the prenatal examinations what lead us to detect a DiGeorge syndrome.
Keywords: second pregnancy; chromosomopathies; DiGeorge syndrome
Introduction
Case Report
19-year-old woman on her second pregnancy, with gestational hyportoroids in the previous gestation as unique personal antecedent. The first pregnancy ended up in cesarean birth because of prolonged delivery labor, with no pathological findings in the first trimester ultrasound. The first trimester combined screening showed a low risk of chromosomopathies and low risk of preeclampsia.
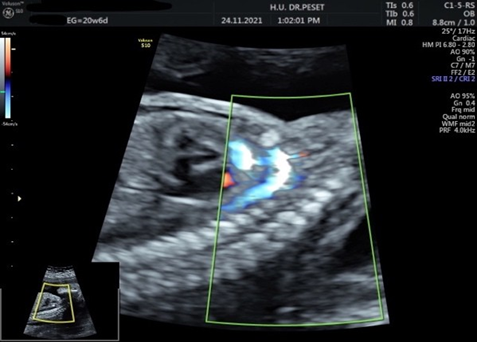
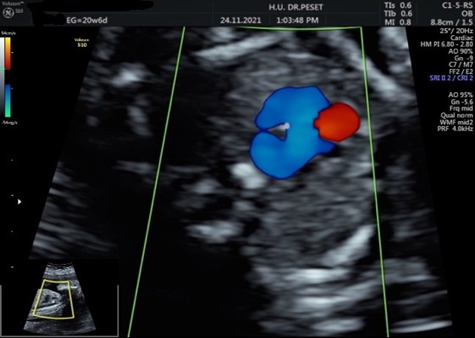
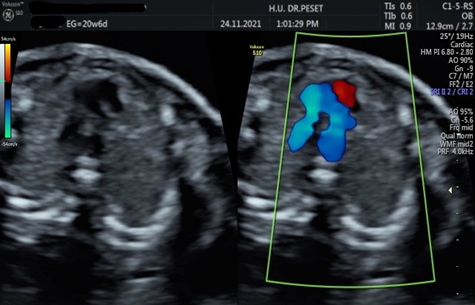
In the morphological ultrasound of the second trimester, an abnormality in the aortic arch was detected. Then, in the echocardiography a left aortic arch, with a retroesophagic course, a right descending aorta artery and right arteriosus ductus (Figure 1, 2), which conform a complete vascular ring, closed by a portion of the pulmonary artery located anterior to the trachea, involving the distal part of the trachea. (Figure 3, 4).
Figure 1
Figure 2
Figure 3
Figure 4
In view of these findings, an amniocentesis was practiced. The FISH study allowed to detect the gender of the fetus, it being female, but it had no pathological findings. However, thanks to the ARRAY study, the 22q11.2 microdeletion CATCH 22, which causes DiGeorge syndrome, was able to be detected. After the explanation of the diagnosis and its prognostic to the patient, she decides not to continue with the pregnancy, thus a legal abort is practiced by the administration of mifepristone and misoprostol. Then, the delivery happens in asystole situation of the fetus. A transvaginal ultrasound is performed to check uterine vacuity and the patient is discharged.
Introduction
Case Report
19-year-old woman on her second pregnancy, with gestational hyportoroids in the previous gestation as unique personal antecedent. The first pregnancy ended up in cesarean birth because of prolonged delivery labor, with no pathological findings in the first trimester ultrasound. The first trimester combined screening showed a low risk of chromosomopathies and low risk of preeclampsia.
In the morphological ultrasound of the second trimester, an abnormality in the aortic arch was detected. Then, in the echocardiography a left aortic arch, with a retroesophagic course, a right descending aorta artery and right arteriosus ductus (Figure 1, 2), which conform a complete vascular ring, closed by a portion of the pulmonary artery located anterior to the trachea, involving the distal part of the trachea. (Figure 3, 4).
Figure 1
Figure 2
Figure 3
Figure 4
In view of these findings, an amniocentesis was practiced. The FISH study allowed to detect the gender of the fetus, it being female, but it had no pathological findings. However, thanks to the ARRAY study, the 22q11.2 microdeletion CATCH 22, which causes DiGeorge syndrome, was able to be detected. After the explanation of the diagnosis and its prognostic to the patient, she decides not to continue with the pregnancy, thus a legal abort is practiced by the administration of mifepristone and misoprostol. Then, the delivery happens in asystole situation of the fetus. A transvaginal ultrasound is performed to check uterine vacuity and the patient is discharged.
Discussion
Vascular rings are less than 1% of all the cardiovascular congenital anomalies. They are vascular structures that involve the trachea, esophagus, or both, causing obstruction on the airway and impeding the swallowing. Their prognostic depends on the obstruction, which also determinates the need for surgical correction, releasing stenosis [7]. In this case report, the left aortic arch and the right descending aortic artery, with the right arteriosus ductus, involve the trachea, and is seen in ultrasound as a vascular ring. In 2012, a similar case was reported: a right aortic arch and a left descending aortic artery was described, the opposite of the abnormality described in our patient. Therefore, the circumflex aortic artery can be developed with a left or right aortic arch, and can be seen in ultrasound as a mediastinal tumor [7], however in both morphologies, the trachea is involved by the vascular ring. This alteration is very unusual, affecting 0.01-0.1% of the population [8]. The prenatal diagnosis of these alterations is based on the morphological ultrasound of the second trimester, which includes an examination of the cardiac anatomy and the outlet of large vessels by the Yagel system. To detect vascular rings, the best plane is the one of the three great vessels and the trachea, in which the pulmonary artery (the most anterior structure), the descending portion of the aorta artery, the superior cava vein (the most posterior structure), and the trachea can be seen. In this plane it is mandatory to evaluate the size of each vessel. In physiological conditions, there is a progressive reduction of the diameter of the vessels, thus, the pulmonary artery is the biggest one, followed by the aortic artery and then the cava vein. Furthermore, the relation of the vessels between each other, the conformation and how they are related to the trachea must all be noticed [9].
Once vascular rings are diagnosed, pre or postnatal, it is recommended to practice a genetical study that includes karyotype, FISH and Array. Our case is not the only one published regarding a diagnosis of the DiGeorge syndrome due to a cardiovascular malformation. In 2020, a case of a 6-month-old child with a right aortic arch and left braquicephalic artery caused by the 22q11.2 microdelection was reported [10]. In addition, another similar case was published in 2019, this time concerning a 2- month-old child with a persistent arteriosum trunk and a double aortic arch. After the genetical examination, he was diagnosed with DiGeorge syndrome [11]. A study published in 2021 showed the relation between the prenatal detection of a right aortic arch with 22q11.2 microdelection, by demonstrating that the incidence of the DiGeorge syndrome is significantly higher in fetus with a right aortic arch [12].
Conclusion
Alterations on the aortic arch are a rare group of malformations, however they could potentially be life threating. It is convenient to recognize and diagnose them as soon as possible since they are associated to systemic disorders. On most occasions, this finding let us detect other abnormalities and genetical syndromes. That is why when a malformation of the aortic arch is detected on the prenatal ultrasound, it is recommended to practice a genetic study of the fetus. Its only possible treatment nowadays is the surgical correction, and its prognosis is uncertain.
References
- Priya S, Thomas R, Nagpal P, Sharma A, Steigner M. (2018). Congenital anomalies of the aortic arch. Cardiovasc Diagn Ther. 8(Suppl 1): S26-S44.
Publisher | Google Scholor - Hanneman K, Newman B, Chan F. (2017). Congenital variants and anomalies of the Aortic Arch. Radio Graphics. 37:1, 32-51.
Publisher | Google Scholor - Goldmuntz E. (2020). 22q11.2 deletion syndrome and congenital heart disease. Am J Med Genet C Semin Med Genet. 184(1):64-72.
Publisher | Google Scholor - Fernandez J. (2019). Síndrome de DiGeorge. MSD manual.
Publisher | Google Scholor - Baird CW, Prabhu S, Buchmiller TL, Smithers C, Jennings R. (2016). Direct Tracheobronchopexy and Posterior Descending Aortopexy for Severe Left Mainstem Bronchomalacia Associated with Congenital Pulmonary Airway Malformation and Left Circumflex Aortic Arch. Ann Thorac Surg. 102(1): e1-4.
Publisher | Google Scholor - Russell HM, Rastatter JC, Backer CL. (2013). The aortic uncrossing procedure for circumflex aorta. Operative Techniques in Thoracic and Cardiovascular Surgery. 18(1):15- 31.
Publisher | Google Scholor - Caicedo LM. (2012). ssCircumflex retroesophageal right aortic arch with left arterial ligament: an infrequent variety of complete vascular ring. Report of case. Rev. Colomb. Cardiol. 19 (1):47-53.
Publisher | Google Scholor - Law MA, Mohan J. (2021). Right Aortic Arches. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
Publisher | Google Scholor - Guías Prácticas. (2013). ISUOG: evaluación ecográfica de tamizaje del corazón fetal. Ultrasound Obstet Gynecol, 41: 348–359.
Publisher | Google Scholor - Malakan Rad E, Momtazmanesh S. (2021). DiGeorge syndrome and anomalous right aortic arch with arch-on-arch and figure-of-eight configurations: Aortic sac maldevelopment and left brachiocephalic artery abnormal remodeling. Ann Pediatr Cardiol. 14(1):125-127.
Publisher | Google Scholor - Moghadam EA, Mirzaaghayan MR, Zeinaloo A, Mohebbi A, Ghamari A. (2019). Truncus arteriosus associated with double aortic arch in a patient with DiGeorge syndrome: A rare case report. Ann Pediatr Cardiol. 12(2):185-186.
Publisher | Google Scholor - Petrescu AM, Ruican D, Tudorache S, Cernea N, Dobrescu MA, et al. (2021). Associated Chromosomal Abnormalities in Fetuses Diagnosed Prenatally with Right Aortic Arch. Curr Health Sci J. 47(2):170-176.
Publisher | Google Scholor