Case Report
Chorioangioma of Placenta: A Case of Incidental Finding in Cesarean Section
- Nidhi Sapolia *
- Shushma Shetiya
- Samar Qasem
- Sura Salih
- Wael Hosni
Department of Obstetrics and Gynaecology, Al Garhoud Private Hospital, Dubai, UAE.
*Corresponding Author: Nidhi Sapolia, Department of Obstetrics and Gynaecology, Al Garhoud Private Hospital, Dubai, UAE.
Citation: Sapolia N, Shetiya S, Qasem S, Salih S, Hosni W. (2024). Chorioangioma of Placenta: A Case of Incidental Finding in Cesarean Section, Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(2):1-3. DOI: 10.59657/2993-0871.brs.24.029
Copyright: © 2024 Nidhi Sapolia, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 03, 2024 | Accepted: January 26, 2024 | Published: February 07, 2024
Abstract
Background: Chorioangioma is a benign angioma of placenta arising from chorionic tissue. Large chorioangioma are known to have adverse effects on both mother and fetus. The incidence is 1% of all pregnancies. Large chorioangioma can result in polyhydramnios, hydrops fetalis, intrauterine growth retardation, sudden intrauterine fetal death, preterm labor and neonatal death associated with congestive cardiac failure.
Case: We report a case of incidental finding of chorioangioma of placenta in a 42 years old female with intrauterine growth restriction, and fetal distress at 39 weeks gestation that necessitated on emergency lower segment cesarean section at 39 weeks gestation. postpartum period was uneventful.
Conclusion: The high risk of morbidity and mortality associated with large chorioangiomas warrants institutional antenatal care and timely delivery.
Keywords: placenta; intrauterine growth restriction; fetal distress; emergency lower segment cesarean section
Introduction
Chorangioma placentae is considered a rare tumor of placenta. Chorangiomas are benign vascular tumors of the placenta arising from chorionic tissue. The rate of their occurrence rises almost linearly with maternal age over 30 years old. Primipara, twin pregnancies, hypertension, diabetes are found more often in combination with chorangiomas [2]. Large placental chorioangioma has adverse effects on both mother and fetus.
Case Presentation
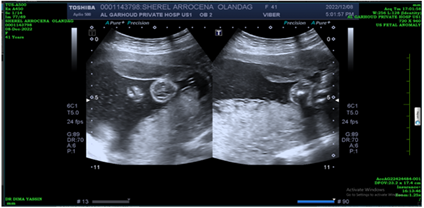
A 42-year-old female, gravida 3 with two living children that were delivered vaginally presented to us at 39 weeks gestation with labor pains. Her first antenatal visit to the hospital was at 36 weeks of gestation. On examination, blood pressure was 111/61 mm Hg, pulse 84 b/m, afebrile, abdominal examination: uterus 38 weeks size, cephalic presentation, fetal parts were palpable, and fetal heart sounds audible 130-140b/m. Vaginal examination: Cervical os 3-4cm dilated, effacement 60%, high presenting part, and the membranes were intact. She was neither hypertensive nor diabetic nor anemic. No history of reduced fetal movements. Ultrasound at 22 weeks of gestation showed a, subchorionic hematoma (Figure 1), measuring 64 x 12.7mm in the anterior wall. No obvious gross congenital abnormalities were detected.
Figure 1: Ultrasound image in 22 weeks of pregnancy. no any signs of abnormality.
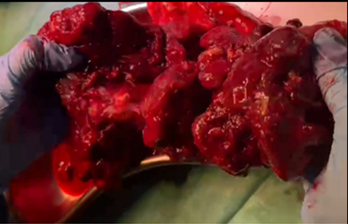
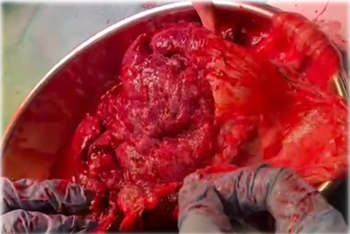
Normal amniotic fluid index. There were no gross structural abnormalities. Placenta was located on the posterior wall upper segment. During the course of labour, Patient went into fetal distress was delivered through emergency cesarean section, A male baby weighing 2.065 Kg with Apgar scores 9 and 10 at 1 and 5 minutes, respectively was delivered. Placenta weighed 500g. On gross examination of the placenta A piece of macerated placenta was seen (Figure 2), placental tissue measures 15.5x15x3.5cm, umbilical cord measures 15cm in length, located eccentrically 1.5cm away from the placental margin. Histopathology of placenta revealed edematous membranes and parenchymal chorangiosis infarction. Umbilical cord was trivascular (Figure 3). The gross examination of the placenta revealed placental tissue measuring 15cm x 20cm, eccentrically located umbilical cord and a piece of macerated placenta (Figure 2).
Figure 2: Dark red tan cut surface of chorioangioma.
Figure 3: Chorioangioma oedematous membranes.
Discussion and pathogenesis
Placental chorioangioma is known to be a common benign tumor of the placenta. It is thought to develop as a malformation of the primitive angioblastic tissue of the placenta. The angiomas get their blood supply by the fetal circulation and thus, when they develop large, they may significantly impede the growth of the fetus and the fetal cardiac activity. Grossly Placental chorangioma can often appear like infarct or intervillous thrombus. Most authors classify them as benign neoplasms, while others consider them as hamartomas, due to their composition of mostly native placental tissue and their inability to metastasize. There can be significant variations in size. Most lesions tend to be small and asymptomatic whereas lesions less than 5 cm are rare. Large angiomas when present can however, be associated with degenerative changes like, calcification, hyalinisation, necrosis or myxomatous degeneration. Tumors of less than 5 cm are usually asymptomatic and accidental findings; these are mostly not associated with maternal and fetal complications. Large tumors on the other hand act as arteriovenous shunts of feto-maternal circulation and may cause complications.
Maternal complications commonly associated with chorioangioma are polyhydramnios, preterm labor, preeclampsia and placental abruption. Of the above associated clinical complications, the correlation of chorioangioma with polyhydramnios and preterm delivery is significant, latter being caused due to hydramnios [6-7]. The increased blood flow through the low resistance vascular channels in the chorioangioma acting as an arteriovenous shunt can cause Fetal congestive heart failure. Other complications associated with large chorioangiomas are hydrops fetalis, hemolytic anemia, congenital anomalies, fetal thromocytopenia, cardiomegaly and intrauterine growth retardation. Large chorioangioma associated with polyhydramnios can lead to high perinatal morbidity and mortality. Postpartum hemorrhage is a well-known complication in mother. In our case the chorioangioma was associated with intrauterine growth Restriction and intrapartum fetal distress. No episode of post-partum hemorrhage was noted.
Conclusion
The high risk for morbidity and mortality that is associated with large chorioangiomas warrants institutional and timely delivery. Diagnosis is by antenatal ultrasound. Doppler is necessary to assess the fetomaternal circulation and to rule out arteriovenous shunts. Regular follow up examinations are of paramount importance for patients with chorangiomas.
References
- Amer HZ, Heller DS. (2010). Chorangioma and related vascular lesions of the placenta--a review. Fetal Pediatr Pathol, 29 (4):199-206.
Publisher | Google Scholor - Guschmann M, Henrich W, Entezami M, Dudenhausen JW. (2003). Chorangioma – new insights into a well-known problem I. Results of a clinical and morphological study of 136 cases. J Perinat Med, 31:163-169.
Publisher | Google Scholor - Batukan C, Holzgreve W, Danzer E, et al. (2001). Large placental chorioangioma as a cause of sudden intrauterine fetal death. A case report. Fetal Diagn Ther, 16:394-397.
Publisher | Google Scholor - Ozer EA, Duman N, Kumral A, et al. (2008). Chorioangiomatosis presenting with severe anemia and heart failure in a newborn. Fetal Diagn Ther, 23:5-6.
Publisher | Google Scholor - D'Ercole C, Cravello L, Boubli L, et al. (1996). Large chorioangioma associated with hydrops fetalis: prenatal diagnosis and management. Fetal Diagn Ther, 11:357-360.
Publisher | Google Scholor - Asadourian LA, Taylor HB. (1968). Clinical significance of placental hemangiomas. Obstet Gynecol, 31:551-555.
Publisher | Google Scholor - Leonidas JC, Beaty EC, Hall RT. (1975). Chorangioma of the placenta: a cause of cardiomegaly and heart failure in the newborn. Am J Roent Rad Ther and Nuc Med, 23:703-707.
Publisher | Google Scholor - Entezami M, Albig M, Knoll U et-al. (2003). Ultrasound Diagnosis of Fetal Anomalies. Thieme.
Publisher | Google Scholor - Jaffe R, Siegal A, Rat L et-al. (1985). Placental chorioangiomatosis--a high risk pregnancy. Postgrad Med J, 61 (715): 453-455.
Publisher | Google Scholor