Case Report
Choked for Over a Decade: A Rare Case of Huge Esophageal Fibro-vascular Polyp Causing Dysphagia
1General and Cardio-thoracic Surgeon, Associate professor of Surgery, Department of Surgery, School of Medicine, College of Health Sciences, Addis Ababa University. Addis Ababa. Ethiopia.
2Health Officer, Head of the Operation Theater, Hallelujah General Hospital. Addis Ababa. Ethiopia.
*Corresponding Author: Seyoum kassa, General and Cardio-thoracic Surgeon, Associate professor of Surgery, Department of Surgery, School of Medicine, College of Health Sciences, Addis Ababa University. Addis Ababa. Ethiopia.
Citation: kassa S., Ayalew D. (2023). Choked for Over a Decade: A Rare Case of Huge Esophageal Fibro-vascular Polyp Causing Dysphagia. Clinical Case Reports and Studies, BioRes Scientia Publishers. 2(6):1-4. DOI: 10.59657/2837-2565.brs.23.051
Copyright: © Seyoum kassa, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: June 26, 2023 | Accepted: July 10, 2023 | Published: July 17, 2023
Abstract
Introduction: Esophageal fibro-vascular polyps (EFVPs) are rare benign tumors that can arise from the submucosa of the esophagus. They are usually asymptomatic but can cause obstruction and dysphagia in some cases. The diagnosis of EFVPs can be challenging due to their rarity and nonspecific symptoms. Delayed diagnosis can result in significant morbidity, as in the case of our patient who suffered from difficulty swallowing for over a decade before being accurately diagnosed. We present a case of a 42-year-old male patient with a 12-year history of difficulty swallowing, who was eventually diagnosed with a huge fibro-vascular polyp after undergoing thoracotomy esophagostomy and excision of the polyp.
Case Presentation: A 42-year-old male patient presented to Hallelujah General Hospital, with a 12-year history of difficulty swallowing, associated with symptoms such as weight loss, fatigue, and asphyxiation while vomiting. The patient had visited several health centers but was unable to receive an accurate diagnosis or effective treatment. Initial investigations revealed a large, smooth, and mobile mass in the mid-esophagus, which was obstructing the lumen and causing difficulty swallowing. A CT scan of the chest and abdomen showed a large polypoid mass in the upper and mid-esophagus, measuring 25 cm in length and 10 cm in diameter, which was confirmed to be an esophageal fibro-vascular polyp upon surgical excision and biopsy.
Conclusion: EFVPs are rare, benign tumors of the esophagus that can cause significant morbidity if not diagnosed and treated promptly. The diagnosis of EFVPs can be challenging, and imaging studies such as CT scans, MRI, and endoscopic ultrasound can be helpful in diagnosing the condition. However, a definitive diagnosis usually requires histological examination of the excised mass. Surgical excision is the treatment of choice for EFVPs, and the prognosis is usually excellent. This case report highlights the importance of considering rare conditions in the differential diagnosis of common symptoms, particularly if the patient does not respond to initial treatment. It also emphasizes the importance of early diagnosis and prompt surgical intervention in preventing complications and improving outcomes for patients with EFVPs.
Keywords: esophageal fibro-vascular polyps; dysphagia; esophagostomy; benign tumors
Introduction
Fibro-vascular polyps are rare benign tumors that can occur in the gastrointestinal tract, most commonly in the esophagus. They are usually asymptomatic, but in some cases, they can cause obstruction and difficulty swallowing. The diagnosis of esophageal fibro-vascular polyps can be challenging, as they can be mistaken for other esophageal masses, such as leiomyomas or esophageal carcinomas. Delayed diagnosis can result in significant morbidity, as in the case of our patient who suffered from difficulty swallowing for over a decade. We present a case of a 42-year-old male patient with a 12-year history of difficulty swallowing, who was eventually diagnosed with a huge fibro-vascular polyp after undergoing thoracotomy esophagostomy and excision of the polyp.
Case Presentation
A 42-year-old male patient presented to our clinic with a 12-year history of difficulty swallowing, associated with symptoms such as weight loss, fatigue, and asphyxiation while vomiting. He had visited several health centers but was unable to receive an accurate diagnosis or effective treatment. His past medical history was significant for gastroesophageal reflux disease (GERD) and hypertension, which were managed with omeprazole and amlodipine, respectively. He denied a family history of gastrointestinal or other malignancies. Upon examination, the patient appeared thin and malnourished. His vital signs were within normal limits. Physical examination was unremarkable.
Initial investigations included a complete blood count, liver and renal function tests, and thyroid function tests, which were all within normal limits. An upper gastrointestinal endoscopy revealed a large, smooth, and mobile mass in the mid-esophagus, which was obstructing the lumen. The surface of the mass was covered by normal mucosa. A CT scan of the chest and abdomen showed a large polypoid mass in the Upper and mid-esophagus, measuring 25 cm in length and 10 cm in diameter. A biopsy of the mass was inconclusive, and the patient was scheduled for surgery.
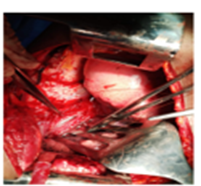
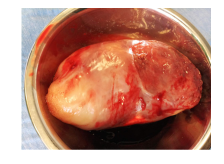
The patient underwent thoracotomy (Figure 1) esophagostomy (Figure 2) and excision of the polyp, which weighed nearly 4 kg. (Figure 4). The polyp was found to arise from the submucosa at the proximal thoracic esophagus, and contain a mixture of fibrous tissue, adipose tissue, and blood vessels consistent with the diagnosis of esophageal fibro-vascular polyp. The patient had an uneventful postoperative course and was discharged on the 6th postoperative day. His symptoms resolved, and he was followed up for three years with no evidence of recurrence.
Figure 1: Thoracotomy and exposure of the hugely dilated esophagus in the posterior mediastinum.
Figure 2: The esophagus is open longitudinally and the polyp popes out to the pleural cavity with pressure.
Figure 3: Closure of the esophagus after excision of the polyp.
Figure 4: The specimen after the resextion
Discussion
EFVPs are rare, benign tumors that arise from the submucosa of the esophagus. They are composed of a mixture of fibrous tissue, adipose tissue, and blood vessels, and they can grow to large sizes. EFVPs are usually asymptomatic, but they can cause obstruction, dysphagia, regurgitation, and respiratory symptoms [1). The diagnosis of EFVPs can be challenging due to their rarity and nonspecific symptoms, and they can be mistaken for other esophageal masses, such as leiomyomas or esophageal carcinomas.
In a case report by Katsinelos et al. (2013), the authors presented a case series and review of the literature on EFVPs. They reported that EFVPs account for less than 1% of all esophageal tumors and that the majority of cases occur in middle-aged adults with a slight male predominance. The authors noted that the most common presenting symptom is dysphagia, which is seen in up to 75% of cases. Other symptoms include regurgitation, chest pain, and weight loss. The diagnosis of EFVPs can be made with imaging studies such as CT scans, MRI, and endoscopic ultrasound, but a definitive diagnosis usually requires histological examination of the excised mass (1,4).
In another case report by Kim et al. (2011), the authors presented a case of an EFVP that presented as upper gastrointestinal bleeding. The patient was initially diagnosed with a bleeding duodenal ulcer and underwent endoscopic hemostasis. However, upper gastrointestinal bleeding persisted, and further investigation revealed a large EFVP in the esophagus. The authors noted that EFVPs can rarely present as upper gastrointestinal bleeding and that a high index of suspicion is necessary to diagnose this rare condition [1,2).
Surgical excision is the treatment of choice for EFVPs, and the prognosis is usually excellent. In a case report by Wang et al. (2015), the authors presented a case of a giant EFVP that was successfully treated with surgical excision. The authors noted that the surgical approach can vary depending on the size and location of the polyp, but complete excision is essential to prevent recurrence [1,5].
Conclusion
Esophageal fibro-vascular polyps (EFVPs) are rare, benign tumors that can cause significant morbidity if not diagnosed and treated promptly. The diagnosis of EFVPs can be challenging due to their nonspecific symptoms and rarity. Imaging studies and endoscopic ultrasound can be helpful in diagnosing EFVPs, but a definitive diagnosis usually requires histological examination of the excised mass. Surgical excision is the treatment of choice for EFVPs, and the prognosis is usually excellent. In this particular case, the patient had suffered from difficulty swallowing for over a decade before being accurately diagnosed with a huge EFVP. The delay in diagnosis highlights the importance of considering rare conditions in the differential diagnosis of common symptoms, particularly if the patient does not respond to initial treatment.
Acknowledgement
We would like to express our sincere gratitude to Hallelujah General Hospital and the staff for their support and assistance in the successful outcome of the surgery for the patient with the huge fibro-vascular polyp of the esophagus. We are grateful to the hospital for allowing us to perform the operation and for providing all the necessary resources and facilities. Without their help, this research would not have been possible.
Declaration
We, the authors of this case report, declare that:
Ethical Conduct: The case report was conducted in accordance with the ethical guidelines and regulations of our institution. We maintained patient confidentiality and obtained informed consent from the patient to publish this case report. We confirm that the patient's personal information has been anonymize to protect their privacy.
Conflict of Interest: We declare that we have no financial or personal relationships that could influence the interpretation of this case report. There are no conflicts of interest to disclose.
Patient Consent: We obtained written informed consent from the patient, who was fully informed about the nature of the case report, its purpose, and the possibility of publication. The patient was given ample time to consider their decision and was free to withdraw their consent at any time. We confirm that the patient's consent form has been retained and can be made available upon request.
Original Work: We declare that this case report is original work and has not been published previously or submitted for publication elsewhere.
Funding: We declare that we did not receive any funding or financial support for this case report.
We acknowledge that any breach of the above declaration may result in the retraction of this case report.
References
- Katsinelos, P., Chatzimavroudis, G., Zavos, C., Pilpilidis, I., & Kountouras, J. (2013). Esophageal fibrovascular polyps: a case series and review of the literature. Journal of gastrointestinal and liver diseases: JGLD, 22(4):439-443.
Publisher | Google Scholor - Kim, E. H., Kim, G. H., Park, D. Y., & Kim, S. (2011). A case of esophageal fibrovascular polyp presenting as upper gastrointestinal bleeding. The Korean journal of gastroenterology = Taehan Sohwagi Hakhoe chi, 57(3):170-173.
Publisher | Google Scholor - Maruotti, A., Miele, V., Grassia,M., Cianciulli, F., et al. (2016). Giant fibrovascular polyp of the esophagus: a case report and review of the literature. World journal of gastrointestinal endoscopy, 8(18):705-710.
Publisher | Google Scholor - Tsai, H. C., Lin, C. K., Chen, Y. C., Lee, et al. (2011). Esophageal fibrovascular polyp presenting as dysphagia: a case report. World journal of gastroenterology, 17(44):4925-4927.
Publisher | Google Scholor - Wang, J., Liu, D., Gao, S., Zhang, C., & Du, J. (2015). Giant esophageal fibrovascular polyp: a case report and review of the literature. World journal of surgical oncology, 13:124.
Publisher | Google Scholor