Case Report
Chimney Technique in The Repair of a Symptomatic Juxtarenal Aneurysm
- Antonio García de Vargas *
Hospital Universitario Virgen del Rocío (Avenida Manuel Siurot SN), Seville, Spain.
*Corresponding Author: Antonio García de Vargas, Hospital Universitario Virgen del Rocío (Avenida Manuel Siurot SN), Seville, Spain.
Citation: Vargas A.G. (2024). Chimney Technique in The Repair of a Symptomatic Juxtarenal Aneurysm. Clinical Case Reports and Studies, BioRes Scientia Publishers. 6(6):1-10. DOI: 10.59657/2837-2565.brs.24.177
Copyright: © 2024 Antonio García de Vargas, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: August 13, 2024 | Accepted: August 30, 2024 | Published: September 13, 2024
Abstract
Endovascular procedures for the management of abdominal aortic injuries have evolved considerably in the last 20 years. Advances in materials, introduction profiles, improvements in the technique and scopy systems, added to the experience of vascular surgeons, have allowed a greater number of patients to be treated using this technique [1,2].
Infrarenal fixation of endovascular prostheses has been one of the limiting factors for endovascular repair of these injuries. Juxta renal aortic aneurysms (JAA) represent between 10 and 15% of all abdominal aortic aneurysms, requiring in many cases for their endovascular treatment the use of fenestrated or branched prostheses that are expensive, complex and require a manufacturing period. and preparation, so it is not applicable in urgent treatment. For this reason, new devices appear such as visceral chimneys (ch-EVAR) [1,2].
Keywords: chimney; juxta renal aortic aneurysms; endovascular
Introduction
The "sandwich or chimney type" treatment was described in 2003 by Greenberg, through the placement of conventional endoprostheses on covered stents, in order to obtain an adequate proximal sealing area and at the same time maintain the patency of visceral arteries [3].
In 2015, the PERICLES study (performing the chimney technique for the treatment of complex lesions) was published, consisting of a total of 13 American and European centers with experience in ch-EVAR, including 517 patients treated between 2008 and 2014. The registry showed results comparable to those of other complex endovascular options, supporting the validity of Ch-EVAR as an immediately available alternative [4, 5].
The mid-term results of Ch-EVAR show high technical success with acceptable patency and absence of endoleaks in selected patients6. Taneva et al. analyzed the data from the long-term PERICLES study and concluded that an acceptable success rate was achieved in the majority of patients operated on using this technique after 5 years [7].
There are two main types of complications associated with this technique [1,2]:
- Occurrence of type I endoleaks: the larger and/or more numerous the chimneys used, the greater the likelihood of these occurring.
- Invagination of the main stent (caused by the chimneys) and compression of the branches (by the main stent).
No gender-specific differences were found for these complications [8].
Clinical Case
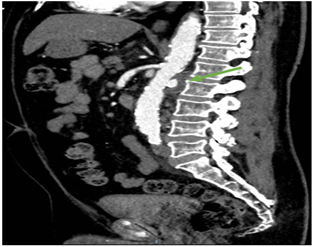
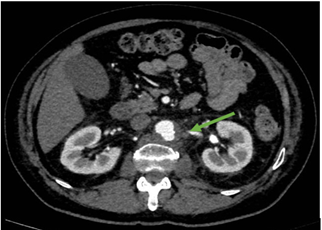
We present a clinical case of a 70-year-old patient, diabetic, hypertensive and dyslipidemic, who began with radiating lumbar pain in a 10-day history that increased in intensity in the last few hours and was not controlled with morphine infusion. On examination, no pulsating mass was observed at the abdominal level with pulses at all levels in the upper extremities and semiology of femoropopliteal obliteration in both lower extremities. In the analysis, it is worth highlighting: 16 thousand leukocytes and hemoglobin at 14 mg/dl with creatinine in the normal range. An urgent CT angiography was requested, in which an aneurysmal dilation in the left posterior wall, measuring 13 x 13 x 16 mm with possible contained rupture, was seen at the juxtarenal level (Figure 1 and 2). It is accompanied by numerous small retroperitoneal nodes, most numerous at the left latero-aortic level.
Figure 1: CT sagittal section. We observed a juxtarenal aneurysmal area.
Figure 2: CT axial section. We observed a juxtarenal aneurysmal area.
Given the high surgical risk, the anatomical characteristics of the aneurysm and the need for early treatment with the impossibility of having a fenestrated or branched endoprosthesis, treatment was decided by endovascular exclusion with "chimney technique in the renal arteries."
The intraoperative arteriography revealed a contained rupture of the juxtarenal aorta on its posterior surface. With the patient in a supine position with the shoulder of the left upper extremity abducted at 90 degrees, the following are placed:
- 12F introducer in the left common femoral artery using antegrade percutaneous puncture. Double presuture with proglide® is previously placed.
- 18F introducer in the right common femoral artery through a transverse incision at the inguinal level.
- Two 7F introducers of 55 and 90cm in the left axillary artery through a longitudinal incision in the axillary fold.
Both renal arteries are cannulated from the axillary access and two 7F introducers are placed. Under scopy, a 28.5 mm Excluder® Gore® endoprosthesis is placed flush in the superior mesenteric artery. With a left branch of 16x12x120mm and a right branch of 16x14x100mm. Subsequently, two 7x39mm VBX stents were placed in both renal arteries. VBX of the left renal artery was overdilated in its distal portion with an 8x20mm Mustang balloon.
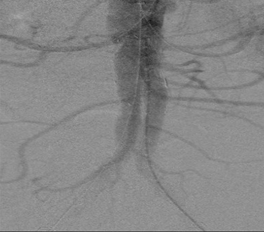
Control arteriography (Figure 3) shows absence of endoleaks and permeability of both kidneys, in addition to no ulcer sac being visualized in the final lateral projection.
Figure 3: Arteriografía control final con permeabilidad de ambas arterias renales.
Closure is performed using two Proglide® in the left groin, 5/0 Prolene in the right common femoral artery and two 6/0 sutures in the axillary accesses. 100 cc of iodinated contrast and 6000 IU of sodium heparin were used at the beginning with basal ACT 110 s; at 60 min 400 sec; at the end of procedure 174 seconds.
In the postoperative phase, antibiotic treatment with ceftriaxone and vancomycin was initiated, as in addition to the leukocytosis and the presence of numerous small retroperitoneal lymph nodes, especially numerous at the left latero-aortic level, a fungal origin of the aortic aneurysm could not be ruled out.
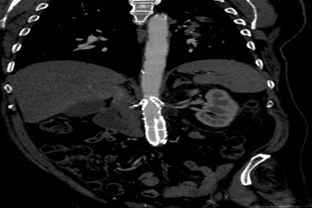
The patient was discharged after completion of antibiotic therapy, with control angiography after one month and after 3 months without endoleaks and with patency of both renal stents (Figure 4 and 5).
Figure 4: Control CT coronal section with permeability of the renal endoprostheses and stents.
Figure 5: control CT axial section showing patency of the renal endoprostheses and stents.
Conclusion
The Ch-EVAR technique has been safely applied to abdominal aortic disease in elective and emergency cases with good results to increase the fixation areas of endoprostheses without the need for conventional surgery in patients with high surgical risk.
Despite the good short, medium and long-term results, the use of this "chimney technique" is still a resource technique in high surgical risk patients with aortic aneurysms that require urgent treatment and closure and when fenestrated or branched prostheses are not available.
References
- P. Bargay Juan, B. Genovés Gascó, M. Ramírez Montoya, J.M. Zaragozá García y E. Ortiz Monzón. (2014). The chimney technique in the repair of a symptomatic aortic juxtarenal aneurysm: presentation of a case. Angiología. 66(2):85-87
Publisher | Google Scholor - Azahara Fernández Carbonell, Pedro Alados Arboledas, Enrique Rodríguez Guerrero, María Eugenia Pérez Montilla, Ignacio Muñoz Carvajal. (2018). Utilidad de la técnica de «chimenea» en el tratamiento de urgencia de aneurismas de aorta abdominal con anatomía desfavorable.Cir Cardiov., 25(3):158-162
Publisher | Google Scholor - Greenberg RK, Clair D, Srivastava S, Bhandari G, Turc A, Hamp- ton J, et al. (2003). Should patients with challenging anatomy be offered endovascular aneurysm repair. J Vasc Surg., 38:990-996.
Publisher | Google Scholor - Donas KP, Lee JT and Lachat M. (2015). PERICLES investiga- tors collected world experience about the performance of the snorkel/chimney endovascular technique in the treatment of complex aortic pathologies: the PERICLES registry. Ann Surg, 262:546-553
Publisher | Google Scholor - Gergana T Taneva, Frank J Criado, Giovanni Torsello, Frank Veith, Salvatore T Scali, Paul Kubilis, et al. (2020). Results of chimney endovascular aneurysm repair as used in the PERICLES Registry to treat patients with suprarenal aortic pathologies. J Vasc Surg.2020;71(5):1521-1527
Publisher | Google Scholor - Eric Ducasse, Caroline Caradu, Coline Brochier, Dominique Midy, Xavier Bérard, Mathieu Poirier, Nicolas Ottaviani. (2019). Midterm Results with the Open Chimney Technique during Endovascular Aneurysm Repair. J Vasc Interv Radiol. 30(4):511-520
Publisher | Google Scholor - Gergana T Taneva, Jason T Lee, Kenneth Tran, Ronald Dalman, Giovanni Torsello, et al. (2021). Long-term chimney/snorkel endovascular aortic aneurysm repair experience for complex abdominal aortic pathologies within the PERICLES registry. J Vasc Surg., 73(6):1942-1949
Publisher | Google Scholor - G Torsello, M V Usai, S Scali, P Kunilis, F J Veith, F Markatis, K P Donas. (2018). Gender-related outcomes of chimney EVAR within the PERICLES registry. 26(6):641-646.
Publisher | Google Scholor