Research Article
Characteristics of Patients Underwent Vesico-Vaginal Fistula Repair and their Repair Outcomes at Yirgalem Hamlin Fistula Center, Southern Ethiopia
- Shimelis Tadesse 1*
- Esuyawkal Mislu 2
- Gizu Tola 1
- Alex Ayenew 3
- Mahlet Tesfaye 1
- Fikremariam Endeshaw 4
1Department of Midwifery, College of Health Science, Mattu University, Mattu, Ethiopia.
2Department of Midwifery, School of Midwifery, College of Health Science, Woldia University, Woldia, Ethiopia
3Department of Health Informatics, College of Health Sciences, Mattu University, Mattu, Ethiopia
4Department of Midwifery, College of Medicine and Health Science, Wolkite University, Wolkite, Ethiopia.
*Corresponding Author: Shimelis Tadesse, Department of Midwifery, College of Health Science, Mattu University, Mattu, Ethiopia.
Citation: Tadesse S, Mislu E, Tola G, Ayenew A, Tesfaye M, et al. (2024). Characteristics of Patients Underwent Vesico-Vaginal Fistula Repair and their Repair Outcomes at Yirgalem Hamlin Fistula Center, Southern Ethiopia. Journal of Women Health Care and Gynecology, BioRes Scientia Publishers. 3(5):1-9. DOI: 10.59657/2993-0871.brs.24.045
Copyright: © 2024 Shimelis Tadesse, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: May 11, 2024 | Accepted: May 30, 2024 | Published: June 10, 2024
Abstract
Background: Worldwide, more than 2 million women are affected by obstetric fistula. Better awareness about the characteristics of women who underwent vesicovaginal fistula repair helps formulate future public health interventions to prevent VVF. The main purpose of this study was to assess the sociodemographic and obstetric profiles of women who underwent VVF repair and their closure success over a 2-year period in the Yirgalem Hamline fistula center, Sidama Regional State, Southern Ethiopia.
Methods: A descriptive facility-based cross-sectional study was conducted from January 1, 2019, to December 30, 2020. The data were collected from all patients who underwent VVF repair and met eligibility criteria between January 1, 2029, and December 31, 2020, from September 22, 2021, to October 22, 2020. A descriptive statistical test of the variables means, range, and SD was employed. The frequency and percentages of variables included in this study were sociodemographic variables, obstetric variables, and successful closure of VVF repair.
Results: A total of 169 patients were included in this study. The mean age of patients with VVF repair was 31.07 (SD± 10.770), ranging from 14–61 years. The majority age (41.4%) was above 34 years old, and 62.7% had no formal education; 71.6% were housewives; 84.6% were married; 65.7% had a weight of less than 50 kg; and 47.9% had a height of less than 150 cm. Moreover, the mean age at first pregnancy was 18.57 (SD ±2.870), range 13–28 years, and the majority were multigravida and multipara with proportions of 36.7% and 40.8%, respectively. The majority (63.3%) had no antenatal care follow-up, 28.4% delivered at home, 68.6% had above 2 days’ labor duration, 49.7% delivered by SVD, and 75.1% of pregnancies resulted in stillbirth. A successful VVF closure outcome was found in 94.7% of cases.
Conclusions: This study revealed that the patients' sociodemographic and obstetric profiles were not favorable. However, the successful VVF repair outcome was within the recommended range of the WHO. Therefore, improving sociodemographic status and quality obstetric care are necessary to prevent and manage obstetric VVF.
Keywords: vesicovaginal fistula; sociodemographic characteristics; obstetric profiles; repair outcomes, fistula center; Southern Ethiopia
Introduction
Background
Vesicovaginal fistula (VVF) is defined as an abnormal communication, acquired and direct, between the bladder and the vagina, resulting in continuous, involuntary leakage of urine into the vaginal vault [1, 2]. Despite the interventions of treatment, it remains the most tragic of preventable childbirth complications, which affect more than 2 million women specifically in developing countries such as South Asia and Africa [3, 4].
Numerous factors contribute to the development of VVF in developing countries. These contributing factors are poverty, early marriage, young-age pregnancy, malnutrition, low levels of medical services, no access to medical health during childbirth, violence of against women. These factors, in one way or another, contributed to poor pelvic growth and obstructed labor, which finally led to victims of obstetric VVF [5, 6].
Previous studies demonstrated that obstetric VVF women are living in rural areas, have a low level of education or no formal education, are short women, teen age at first marriage or pregnancy or birth, are women of primiparity, have prolonged labor, and deliver at home [7–10]. Therefore, awareness about these factors is important to preventing and managing obstetric VVF, which contributes to the Sustainable Development Goal 3 of improving maternal health [11].
The World Health Organization (WHO) proposes a successful closure rate for the first repair of VVF of85% in each treatment center, with continence achievement among the closed cases at 90% [12]. Patients who remained continent without any urinary leak after catheter removal after three weeks of surgery were considered successful VVF repairs. Based on different studies conducted in different fistula centers and countries, the obstetric VVF repair closure rate ranged from 63 to 100%, as cited by Tebeu et al. [13]. The systematic review conducted from studies done from 1985 to 2018 showed that the outcome of VVF repair was above 90% [14]. The repair of obstetric VVF restores women’s quality of life [15], and the repair was done through the transvaginal route, which has a higher success rate with low morbidity and post-repair complications [16].
Obstetric VVF has long-term medical, social, and psychological effects on the patient and their family [1, 17]. Therefore, prompt diagnosis and timely repair are essential for successful management of these cases [16]. Obstetric VVF can occur in different women with varied socio-economic conditions [18].
Globally, various studies have been conducted on the incidence, causes, risk factors, diagnosis, and treatments of obstetric VVF [14]. However, there is limited research that has analyzed the socio-demographic characteristics and obstetric profiles of VVF patients who underwent surgical repair in the study area of Ethiopia. Therefore, the purpose of this study was to evaluate the sociodemographic characteristics, obstetric profiles, and VVF closure success of patients who underwent repair at the Yirgalem Hamlin fistula center in Sidama Regional State, Southwest Ethiopia.
Awareness of the sociodemographic characteristics, obstetric profiles, and repair outcomes of women who underwent VVF repair helps to formulate strategies and solutions for the future prevention of obstetric VVF cases [19]. Hence, investigating these cases will generate information for health workers, policymakers, and government and non-governmental organizations to formulate strategies and solutions to prevent and manage obstetric VVF.
Methods
Study design, period, and setting
A descriptive facility-based retrospective cross-sectional study was conducted at Yirgalem Hamlin fistula center, Southern Ethiopia, over 2 years-period, and data were collected from September 22, 2021, to October 22, 2021. The study site is in Sidama Regional state, 300 kilometers away from Addis Ababa, Ethiopia. The center provides services with 1 gynecologist, 1 midwife, 4 health officers, and 14 trained aid nurses and has 38 beds [20].
Population and eligibility criteria
Women who underwent VVF repair at Yirgalem Hamlin fistula center between January 01, 2019, and December 31, 2020, were included in this study.
Medical records of all the study population were reviewed in the study. However, medical records with incomplete data records were excluded from the study.
Sample size, sampling techniques and procedures
The study included all women who had VVF repaired in the last 2 years, from January 1, 2019, to December 31, 2020 (n= 169). Among 169 patients, data on 87 and 82 women underwent VVF repairs were collected in 2019 and 2020, respectively. All women between the selected years were included who met the eligibility criteria. The card numbers were identified from the registration book of women who underwent VVF repair and were registered between January 2016 and December 2020. Accordingly, 169 cards were identified as having had a VVF fistula repaired in the previous 2 years. All the cards were reviewed to ensure that they had all the information required for the study.
Data collection tools and procedures
The data collection checklist was used to collect sociodemographic variables, obstetric variables, and closure status of the women who underwent VVF repair in the last 2 years from the patient's chart and operation logbook. Two data collectors and one supervisor with a background of one nurse and two midwives who have a Bachelor of Science degree were assigned.
Validity and reliability of data collection checklist
The validity and reliability of the data collection checklist were assured by using the national fistula patient management recording format and related literature. In addition, a pretest was implemented, and experts have reviewed the data collection checklist.
Data processing and analysis
After the data collection is completed, the data is checked for completeness, coded, and cleaned. Then, the data were entered into EPI Data Version 3.1 and exported into SPSS Version 25.0 to analyze the results.
Descriptive statistics (mean, range, and SD) were used to describe the various variables using a table, histogram, and pie chart.
Study outcomes
The main outcomes of this study were patients' sociodemographic characteristics, obstetric profiles, and VVF repair outcomes.
Operational definition
Successful VVF closure: the status of women who underwent VVF repair as having a closed fistula after 21 days of the repair had been done.
Data quality control
The data quality was assured through training about the objectives of the data collection checklist for a supervisor and data collectors. Moreover, close supervision was employed by the supervisor, and daily activities were checked for completeness, clarity, and consistency by the supervisor and principal investigator.
Results
Sociodemographic characteristics women underwent VVF repair
A total of 169 patients who underwent VVF repairs and met the eligibility criteria were used for the analysis of this study. Among these, 87 and 82 study subjects were collected from 2019 and 2020 data on women who underwent VVF repair, respectively. The mean age of women at repair was 31.07 (SD ± 10.770) with a range between 14 and 61 years old. The majority age (41.4%) group was above 34 years old, and the second highest group (39.6%) was between 20 and 34 years old, followed by 18.9% of patients less than 20 years old (Tables 1 and 2).
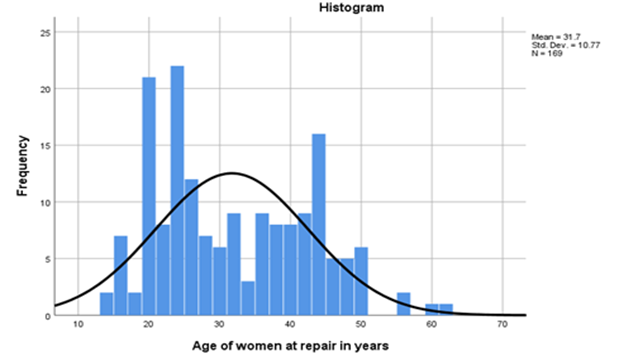
Figure 1: Histogram showing age distribution of women underwent VVF repair
The age distribution of women who underwent VVF repair was almost normally distributed (Figure 1). The age distribution of women who underwent VVF repair was almost normally distributed (Figure 1).
Most of the study subjects (62.7%) have no formal education. About 36.7% of women have some formal education. It was evident that most of the study subjects’ occupations were housewives (71.6%). Regarding the marital status of women who underwent VVF repair, most women are married (84.6%) (Table 2).
In this study, 65.7% of women who underwent VVF repair had a weight less than 50 kg and a height less than 150 cm. The mean weight and height of women who underwent VVF repair in this study were 48.024 (SD ± 7.617) and 151.636 (SD ± 7.991) respectively (Tables 1 and 2).
Table 1: Continues sociodemographic variables showing minimum values, maximum value, mean, and SD
| Variables | Minimum value | Maximum value | Mean | SD |
| Age of women at repair | 14 | 61 | 31.70 | 10.770 |
| Weight of women | 31 | 73 | 48.024 | 7.617 |
| Height of women | 125 | 170 | 151.636 | 7.991 |
Table 2: Sociodemographic status of women underwent VVF repair at Yirgalem Hamlin fistula center, Southwest Ethiopia, 2023
| Variables | Category | Frequency (n=169) | Percent (%) |
| Women age at fistula repair | < 20> | 32 | 18.9 |
| 20-34 | 67 | 39.6 | |
| > 34 | 70 | 41.4 | |
| Educational level | Have no formal education | 106 | 62.7 |
| Have some formal education | 62 | 36.7 | |
| Data not found | 1 | 0.6 | |
| Occupation | Housewife | 121 | 71.6 |
| Marital | Farmers | 33 | 19.5 |
| Others | 6 | 3.6 | |
| Data not found | 9 | 5.3 | |
| Marital status | Single | 4 | 2.4 |
| Married | 143 | 84.6 | |
| Divorced/Separated | 13 | 7.7 | |
| Widowed | 2 | 1.2 | |
| Data not found | 7 | 4.1 | |
| Weight in kilograms | < 50> | 111 | 65.7 |
| > or = 50 | 58 | 34.3 | |
| Height in centimeters | < 150> | 81 | 47.9 |
| > or = 150 | 88 | 52.1 |
Obstetric profile of women underwent VVF repair
In this study, among 169 patients, the majority (54.4%) were first-time pregnant during their teen-age period (18 years), while 45.6 were pregnant after age 18 years and above. The mean age at first pregnancy was 18.57 (SD ± 2.870) years; the mean gravida was 3.47 (SD ±2.471), mean number of parities was 3.18 (SD ± 2.274), and the mean duration of labor was 56.48 (SD ± 28.344) hours (Tables 3 and 4). of the study subjects, 36.7% were multigravida and 40.8% were multiparity. In addition, most of the study subjects (63.3%) had no antenatal care follow-up. Moreover, about 28.4% of women had home delivery at the time the fistula developed, and many women had greater than 2 days’ labor duration. About 84 (49.7%) pregnancies resulted in spontaneous vaginal delivery (SVD), and 127 (75.1%) pregnancies resulted in stillbirth (Table 4).
Table 3: Important continuous obstetric variables of minimum value, maximum value, mean, and SD
| Variables | Minimum value | Maximum value | Mean | SD |
| Age of at first pregnancy | 13 | 28 | 18.57 | 2.870 |
| Gravida | 1 | 10 | 3.47 | 2.471 |
| Parity | 1 | 9 | 3.18 | 2.274 |
| Durations of labour | 8 | 168 | 56.48 | 28.344 |
Table 4: Obstetric profiles of women underwent VVF repair at Yirgalem Hamlin fistula center, Southwest Ethiopia, 2023
| Variables | Category | Frequency (n=169) | Percent (%) |
| Age of women at first pregnancy | < 18> | 92 | 54.4 |
| > or = 18 | 77 | 45.6 | |
| Gravida of women | Primigravida | 54 | 32.0 |
| Multigravida | 62 | 36.7 | |
| Grand multigravida | 53 | 31.4 | |
| Parity of women | Primipara | 57 | 33.7 |
| Multipara | 69 | 40.8 | |
| Grand multipara | 43 | 25.4 | |
| Presence of antenatal care | Yes | 57 | 33.7 |
| No | 107 | 63.3 | |
| Data not found | 5 | 3 | |
| Place of delivery at development of fistula | Home | 48 | 28.4 |
| Health facility | 121 | 71.6 | |
| Duration of labor at development of fistula | < or> | 116 | 68.6 |
| < 48> | 53 | 31.4 | |
| Mode of delivery at development of fistula | SVD | 84 | 49.7 |
| Instrumental vaginal delivery | 5 | 3 | |
| Cesarean section | 80 | 47.3 | |
| Fetal outcome at development of fistula | Still birth | 127 | 75.1 |
| Live birth | 42 | 24.9 |
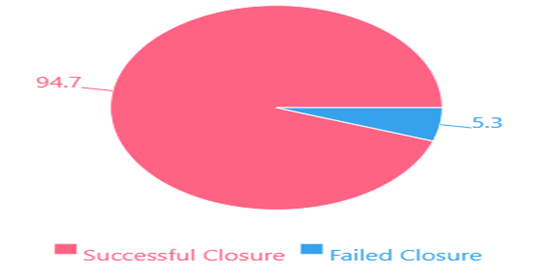
In this study, about 94.7% of women who underwent VVF fistula repair had successful closure at the time of discharge, while 5.3% of women had failed fistula closure (Figure 2).
Figure 2: Proportion of obstetric VVF closure among patients underwent repair in Yirgalem Hamlin fistula center, southwest Ethiopia, 2023 (n=169)
Discussion
In this cross-sectional study, we aimed to describe the characteristics of patients who underwent VVF repair at the Yirgalem Hamlin fistula center in southwest Ethiopia during the 2-year period (January 1, 2019, to December 31, 2020). We analyzed data on sociodemographic factors such as age of patients at repair, education, occupation, marital status, weight, and height; obstetric profiles such as age at first time pregnancy, number of pregnancies, number of deliveries, duration of labor, mode of delivery, place of delivery, fetal outcomes in indexed pregnancies; and VVF repair outcomes among 169 patients who met the eligibility criteria. This study showed that the mean age of patients underwent VVF repair were 31.07 (SD ± 10.770) with a range between 14 and 61. Majority (41.4%) were in the age group of above 34 years, followed by 39.6% in the age group of 20 to 34 years while age below 20 years was accounted for 18.9%. The percentage of age group below 20 years was consistent with the findings from the clinical review done from studies selected in Sub-Saharan African countries and the Middle East [10], and a study done at Bahir Dar Hamlin fistula center which showed the proportion of patients in the age group below 20 years was lowest (11.7%) [21]. The similarities of the study findings could be explained by the similarities of patient’s socio-demographic status and maternal health service utilization. However, this finding was in contrast with the study conducted in Cameroon, which showed the highest age group between 20 and 34, which is 59.5% unlike this study’s findings [13]. The result was also in contrast with the studies conducted in Bangladesh, which showed the mean age was 46.02 (±SD 6.104), ranged from 38 to 70 years, and Nigeria showed the largest percentage below 34 years [18, 22]. The study findings done in Jimma specialized hospital (Ethiopia) also contrast with the present study. The difference might be the small sample size used, which is 86, unlike the current study [23].
In this study, the majority (62.7%) of patients had no formal education, while 71.6% of patients who underwent VVF repair were housewife. The result was in line with the studies conducted at Harar Hamlin fistula center, Jimma specialized hospital (Ethiopia), and Bahir Dar Hamlin fistula center [23, 24]. However, in contrast, regarding marital status, the result is in line with the study conducted in Cameroon [13]. Regarding educational status, the present result was in contrast with the study findings from Nigeria, which showed the smallest proportion of patients (15.4%) with no formal education, whereas the majority had some formal education [22]. The result was also in contrast with the study findings from Zambia, which showed the highest number of patients (80.3%) with some formal education [9]. The difference could be explained by the setting difference. In this study, the majority (84.6%) of patients were married, followed by 7.7% of divorced or separated patients. The result was in line with the study conducted in Harar Hamlin fistula center [24] and a study conducted in Bahir Dar Hamlin fistula center, which showed the highest proportion of women (81.6%) were married [21]. The consistency might be the similarity in demographic data. However, it contrast with the study results of Jimma Specialized Hospital, which showed a large percentage (45.3%) of patients with divorced status, unlike the current study result [23]; and Nigeria, where 50.0% of patients were divorced [22]. The difference might be explained by the study inclusion criteria and settings. The current study showed that the majority (65.7%) of patients who underwent VVF repair had a weight of less than 50 kg and 34.3% of patients had a weight of 50 kilograms and above. This result was in line with the study conducted in Harar Hamlin fistula center (73.9%) and Bahir Dar Hamlin fistula center (58.4%) patients underwent obstetric fistula repair with a weight less than 50 kg [24].
This study also showed that 47.9% of patients had a height less than 150 cm and 52.1 % had a height of 150 cm and above. This result was in contrast with the study conducted in the Harar Hamlin fistula center, which showed about 32.1% of patients had a height of less than 150 cm [24]. Moreover, the study found that the mean age of women during their first pregnancy was 18.57 (SD ± 2.870) years, ranging from 13 to 28 years, and the majority (54.4%) were pregnant at an age less than 18 years. This result is consistent with studies done in Bangladesh, which showed more than 50% were less than 19 years old at their first childbirth [4], and Zambia, where the majority (80.3%) of patients were pregnant at an age less than 20 years old [9] . This early age of pregnancy highlights the need for better family planning and reproductive health education to empower women to make informed choices about their health and reproductive futures. In this study, the majority (36.7%) and majority (40.8%) were multigravida and multipara, respectively, followed by (32.0%) primigravida and (33.7%) primipara. This result was in agreement with the findings from the clinical review done from studies selected in sub-Saharan African countries and the Middle East by Tebeu et al. (2012), which showed that 31.0 to 66.7% were primiparaous [10]. This might show that multiparous women are also at risk of developing obstetric fistula, and they should not be forgotten when addressing fistula [25]. However, the result was in contrast with studies done in Nigeria, which showed the largest percentage of primiparous women were affected (80.9%) [22], and the Bahir Dar Hamlin fistula center showed the highest proportion of primiparous women (43.6%) [21]. In addition, in this study, the majority (63.3%) of patients who underwent VVF repair had no ANC follow-up, while the rest (33.7%) had ANC follow-up for the cause of pregnancy for VVF. The result was consistent with study findings done at Jimma specialized hospital (Ethiopia) [23]. This highlights the need for increased access to and utilization of ANC services.
This study result showed that nearly one-third (28.4%) of patients were delivered at home, while the majority (71.6%) were delivered at health facilities (health centers and hospitals). The result of this study was relatively low compared to the study findings from Jimma Hospital, which showed about 50% of patients were delivered at home in indexed delivery [23]. The difference could be explained by the improvement of maternal health services over time. Regarding the place of delivery, the result was in agreement with the study result of the Bahir Dar Hamlin fistula center, which showed the highest proportion of patients (60.3%) were delivered at a health institution [21].
Regarding the duration of labor at the time of the development of VVF, the mean duration of labor in this study was 56.48 hours, ranging from 8 to 168 hours; the majority (68.6%) had a labor duration of 48 hours and more, and nearly one-third (31.4%) had a labor duration of less than 48 hours. This study result is in line with the study conducted by Tebeu et al. (2012), which showed the range of labor duration from 2.5 to 4 days [10]. The result was also consistent with study findings done in Jimma specialized Hospital (Ethiopia) [23]. The similarities could be explained by the low-level maternal health service during the indexed pregnancy in the country level. Regarding the mode of delivery at the time of the development of the fistula in patients who underwent VVF repair, the majority (49.7%) were delivered by SVD, followed by 47.5% of cesarean section delivery. The result was also consistent with studies done in Jimma specialized hospital (Ethiopia) [23] and Bahir Dar Hamlin fistula center [21]. The high percentage of SVD was consistent with the Ethiopian cultural tradition of vaginal delivery, which could be explained by the high incidence of VVF in Ethiopia.
The present study showed that three fourth (75.1%) patients underwent VVF repair delivered stillbirths. This result was higher than the study findings done in Jimma specialized hospital (Ethiopia), which were 58.1% stillbirths [23]. The result was in line with a study done in Zambia, which revealed the highest stillbirth outcome (78.1%) [9]. This highlights the need for early detection and management of obstetric complications to prevent poor fetal outcomes.
The present study has also shown that among patients who underwent VVF repair, about 94.7% had successful closure of the repair, while only 5.3% had failed fistula closure. The result was in line with the study done in Cameroon, which showed a 92% successful closure obstetric VVF [26]. The result was also in line with the systematic review conducted from studies done from 1985 to 2018, which showed above 90% of patients had successful closure of VVF repair [14]. This result was in the recommended range of WHO genitourinary fistula repair outcomes [14]. This result was in the recommended range of WHO genitourinary fistula repair outcomes [12]. However, it is important to note that this study has some limitations, including the use of a small sample size and a descriptive cross-sectional design that limits the ability to establish causality.
Conclusions
Based on the findings of the study, it is concluded that the study provides valuable insights into the sociodemographic characteristics and obstetric profiles of women who underwent VVF repair surgery at the Yirgalem Hamlin fistula center. The findings revealed that many patients were younger at their first pregnancy, and therefore women who are pregnant at a younger age are most commonly victims of VVF. In addition, patients with unfavorable obstetric profiles may experience complications like VVF. Regarding the VVF patients repair outcomes, there was a higher successful closure rate among patients who underwent VVF repair at the Yirgalem Hamlin fistula center. Therefore, having good sociodemographic status and quality obstetric care during perinatal care are cornerstones to preventing and managing VVF. The present study provides a comprehensive description of the sociodemographic and obstetric characteristics of patients who underwent VVF repair at the Yirgalem Hamlin fistula center.
List of abbreviations
ANC Antenatal Care
SD Standard Deviation
SPSS Statistical Package for Social Science
SVD Spontaneous Vaginal Delivery
VVF Vesicovaginal Fistula
WHO World Health Organization
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board of Hawassa University. Informed consent was obtained from the responsible/managerial bodies of the Yirgalem Hamlin fistula center. Because the data were collected retrospectively from patients’ medical charts, consent was not obtained from individual patients. All the methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing of interests
The authors declare that they have no competing interests.
Funding
Not provided special funding
Authors' contributions
ST contributed to the conception, design, analysis, drafts of the article, and the drafting of the manuscript. MT, GT, and AA contributed to the analysis and interpretation of the data. FE and EM wrote up the draft articles, drafted the manuscript, and revised it. All authors agree to be responsible for ensuring the quality and accuracy of the work and have read and approved the final draft of the manuscript.
Acknowledgements
We are grateful to thank the staff of the Yirgalem Hamlin fistula center for their support during data collection.
References
- E. Sharma, M. Iqbal, and S. Masood. (2021). “Five-Year Retrospective Study on the Management of Vesicovaginal Fistula from a Tertiary Care Centre of Jammu,” JK Sci. 23(4):191-194.
Publisher | Google Scholor - N. KE. (2019). “Epidemiological and Therapeutic Aspects of Obstetric Fistula in The Peri Urban Area of Butembo in the Democratic Republic of Congo,” J. Gynecol. Womens Heal, 17(4):1-3
Publisher | Google Scholor - G. Dangal, K. Thapa, K. Yangzom, and A. Karki. (2014). “Obstetric Fistula in the Developing World: An Agonising Tragedy,” Nepal J. Obstet. Gynaecol, 8(2):5-15.
Publisher | Google Scholor - D. U. S. Bilkish, D. R. Begum, D. S. Apsara, and D. J. Yasmin, “Analysis of Vesicovaginal Fistulas in Sylhet MAG Osmani Medical Hospital: A Two Years Study,” Sch. Int. J. Obstet. Gynecol, 5(11):506-516.
Publisher | Google Scholor - C. J. Hillary, N. I. Osman, P. Hilton, and C. R. Chapple. (2016). “The Aetiology, Treatment, and Outcome of Urogenital Fistulae Managed in Well-and Low-resourced Countries: A Systematic Review,” Eur. Urol, 44:1-15.
Publisher | Google Scholor - J. K. Barageine. (2015). “Genital fistula among Ugandan women: Risk Factors, Treatment Outcomes and Experiences of Patients & Spouses,” Makerere University.
Publisher | Google Scholor - A. Kabore et al. (2021). “Characteristics of Obstetric and Iatrogenic Urogenital Fistulas in Burkina Faso: A Cross-Sectional Study,” Hindawi Adv. Urol.
Publisher | Google Scholor - M. Maheu-Giroux et al. (2016). “Risk factors for vaginal fistula symptoms in Sub-Saharan Africa: a pooled analysis of national household survey data,” BMC Pregnancy Childbirth, 16(82):1-14.
Publisher | Google Scholor - A. Holme, M. Breen, and C. MacArthur. (2007). “Obstetric fistulae: A study of women managed at the Monze Mission Hospital, Zambia,” BJOG An Int. J. Obstet. Gynaecol, 114(8):1010–1017.
Publisher | Google Scholor - P. M. Tebeu, J. N. Fomulu, S. Khaddaj, L. De Bernis, T. Delvaux, and C. H. Rochat. (2012). “Risk factors for obstetric fistula: a clinical review,” Int Urogynecol J, 23:387-394.
Publisher | Google Scholor - Y. Doe. (2020). “Obstetric Fistula in the Developing Countries,”.
Publisher | Google Scholor - L. De Bernis. (2007). “Obstetric fistula: Guiding principles for clinical management and programme development, a new WHO guideline,” Int. J. Gynecol. Obstet, 99: s117-s121.
Publisher | Google Scholor - P. M. Tebeu et al. (2017). “Tebeu’s Pronostic Classi fi cation of Obstetric Fistula According to Anatomopathologic Variables from the University Teaching Hospital, Yaounde Cameroon -,” Int. J. Reprod. Med. Gynecol, 3(1):29-33.
Publisher | Google Scholor - A. S. El-Azab, H. A. Abolella, and M. Farouk. (2019). “Update on vesicovaginal fistula: A systematic review,” Arab J. Urol, 17(1):61-68.
Publisher | Google Scholor - A. Kulkarni, A. Madsen, S. Andiman, A. Nishimwe, and B. S. Hampton. (2019). “Obstetric Fistula Repair in Sub-Saharan Africa: Partnering to Create Sustainable Impact for Patients and Trainees,” R. I. Med. J, 21-24.
Publisher | Google Scholor - S. Rajaian, M. Pragatheeswarane, and A. Panda. (2019). “Vesicovaginal fistula: Review and recent trends,” Indian J. Urol, 35(4):250-258.
Publisher | Google Scholor - M. Muleta, E. C. Hamlin, M. Fantahun, R. C. Kennedy, and B. Tafesse. (2008). “Health and Social Problems Encountered by Treated and Untreated Obstetric Fistula Patients in Rural Ethiopia,” J. Obstet. Gynaecol. Canada, 30(1):44-50.
Publisher | Google Scholor - S. Akter et al. (2020). “Socio-demographic Characteristics of Vesico-vaginal fistula (VVF) patients attended at a tertiary Care Hospital in Bangladesh,” Natl. Inst. Neurosci. Bangladesh, 6(2):114-117.
Publisher | Google Scholor - A. Kay, A. Idrissa, and B. S. Hampton. (2014). “Epidemiologic profile of women presenting to the National Hospital of Niamey, Niger for vaginal fistula repair,” Int. J. Gynecol. Obstet, 126(2):136-139.
Publisher | Google Scholor - S. Tadesse, N. Ejigu, D. Edosa, T. Ashegu, and D. Dulla. (2022). “Obstetric fistula repair failure and its associated factors among women underwent repair in Yirgalem Hamlin fistula center, Sidama Regional State, Southern Ethiopia, 2021: a retrospective cross-sectional study,” BMC Womens. Health, 1-11.
Publisher | Google Scholor - A. A. Aynie, A. G. Yihunie, and A. M. Munae, “The magnitude of repair failure and associated factors among women undergone obstetric fistula repair in Bahir Dar Hamlin Fistula Center, Amhara Region, Northwest Ethiopia,” Int J Sci Rep, 5(11):324-331.
Publisher | Google Scholor - A. J. Umoiyoho, E. C. Inyang-etoh, and E. A. Etukumana. (2012). “Obstetric Fistula Repair: Experience with Hospital-Based Outreach Approach in Nigeria,” Glob. J. Health Sci, 4(5):40-45.
Publisher | Google Scholor - Zegeye Nahome and Dagne Tesfaye. (2017). “Retrospective Study of Obstetric Fistula among Clients Admitted to Fistula Unit Jimma University Specialized Hospital, Oromia Region, South West Ethiopia,” J. Women’s Heal. Care, 6(5):3-6.
Publisher | Google Scholor - S. Hussen and E. Melese. (2017). “Original article Time-to-recovery from obstetric fistula and associated factors: The case of Harar Hamlin Fistula Center,” Ethiop. J. Heal. Dev, 31(2):85-95.
Publisher | Google Scholor - D. Sereke, H. Hailemelecot, Y. Issak, and D. Estifanose. (2020). “Obstetric Vesico-vaginal Fistulae: A Documentary Review of Women Managed in Mendefera Zonal Referral and National Fistula Hospital, Eritrea,” Sci. J. Public Heal, 8(5):149-154.
Publisher | Google Scholor - Tebeu et al. (2010). “Quality care in vesico-vaginal obstetric fistula: case series report from the regional hospital of Maroua-Cameroon,” Pan Afr. Med. J, 5(6):1-7.
Publisher | Google Scholor